Pioglitazone
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: CONGESTIVE HEART FAILURE
See full prescribing information for complete Boxed Warning.
Congestive Heart Failure:
|
Overview
Pioglitazone is a thiazolidinedione and an agonist for peroxisome proliferator-activated receptor (PPAR) gamma that is FDA approved for the {{{indicationType}}} of type 2 diabetes mellitus. There is a Black Box Warning for this drug as shown here. Common adverse reactions include upper respiratory tract infection, headache, sinusitis, myalgia, and pharyngitis.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Type 2 Diabetes Mellitus
- Dosing Information
- Monotherapy and Combination Therapy
- ACTOS is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus in multiple clinical settings.
- Important Limitations of Use
- ACTOS exerts its antihyperglycemic effect only in the presence of endogenous insulin. ACTOS should not be used to treat type 1 diabetes or diabetic ketoacidosis, as it would not be effective in these settings.
- Use caution in patients with liver disease.
- Recommendations for All Patients
- ACTOS should be taken once daily and can be taken without regard to meals.
- The recommended starting dose for patients without congestive heart failure is 15 mg or 30 mg once daily.
- The recommended starting dose for patients with congestive heart failure (NYHA Class I or II) is 15 mg once daily.
- The dose can be titrated in increments of 15 mg up to a maximum of 45 mg once daily based on glycemic response as determined by HbA1c.
- After initiation of ACTOS or with dose increase, monitor patients carefully for adverse reactions related to fluid retention such as weight gain, edema, and signs and symptoms of congestive heart failure.
- Liver tests (serum alanine and aspartate aminotransferases, alkaline phosphatase, and total bilirubin) should be obtained prior to initiating ACTOS. Routine periodic monitoring of liver tests during treatment with ACTOS is not recommended in patients without liver disease. Patients who have liver test abnormalities prior to initiation of ACTOS or who are found to have abnormal liver tests while taking ACTOS should be managed as described under Warnings and Precautions.
- Concomitant Use with an Insulin Secretagogue or Insulin
- If hypoglycemia occurs in a patient co-administered ACTOS and an insulin secretagogue (e.g., sulfonylurea), the dose of the insulin secretagogue should be reduced.
- If hypoglycemia occurs in a patient co-administered ACTOS and insulin, the dose of insulin should be decreased by 10% to 25%. Further adjustments to the insulin dose should be individualized based on glycemic response.
- Concomitant Use with Strong CYP2C8 Inhibitors
- Coadministration of ACTOS and gemfibrozil, a strong CYP2C8 inhibitor, increases pioglitazone exposure approximately 3-fold. Therefore, the maximum recommended dose of ACTOS is 15 mg daily when used in combination with gemfibrozil or other strong CYP2C8 inhibitors.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Pioglitazone in adult patients.
Non–Guideline-Supported Use
Cerebrovascular disease - Impaired glucose tolerance
- Dosing Information
- Pioglitazone 15 mg/day was increased to 30 mg/day after 2 weeks and to 45 mg/day after another 2 weeks.
Diabetes mellitus type 2 - Disorder of cardiovascular system, Secondary disease; Prophylaxis
- Dosing Information
- Pioglitazone (45 mg/day).[1]
Generalized atherosclerosis
- Dosing Information
- Pioglitazone 15 mg.
Polycystic ovary syndrome
- Dosing Information
- Pioglitazone 45 mg/day.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Pioglitazone in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Pioglitazone in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Pioglitazone in pediatric patients.
Contraindications
- Initiation in patients with established NYHA Class III or IV heart failure.
- Use in patients with known hypersensitivity to pioglitazone or any other component of ACTOS.
Warnings
|
WARNING: CONGESTIVE HEART FAILURE
See full prescribing information for complete Boxed Warning.
Congestive Heart Failure:
|
Precautions
- Congestive Heart Failure
- ACTOS, like other thiazolidinediones, can cause dose-related fluid retention when used alone or in combination with other antidiabetic medications and is most common when ACTOS is used in combination with insulin. Fluid retention may lead to or exacerbate congestive heart failure. Patients should be observed for signs and symptoms of congestive heart failure. If congestive heart failure develops, it should be managed according to current standards of care and discontinuation or dose reduction of ACTOS must be considered.
- Hypoglycemia
- Patients receiving ACTOS in combination with insulin or other antidiabetic medications (particularly insulin secretagogues such as sulfonylureas) may be at risk for hypoglycemia. A reduction in the dose of the concomitant antidiabetic medication may be necessary to reduce the risk of hypoglycemia.
- Hepatic Effects
- There have been postmarketing reports of fatal and non-fatal hepatic failure in patients taking ACTOS, although the reports contain insufficient information necessary to establish the probable cause. There has been no evidence of drug-induced hepatotoxicity in the ACTOS controlled clinical trial database to date.
- Patients with type 2 diabetes may have fatty liver disease or cardiac disease with episodic congestive heart failure, both of which may cause liver test abnormalities, and they may also have other forms of liver disease, many of which can be treated or managed. Therefore, obtaining a liver test panel (serum alanine aminotransferase [ALT], aspartate aminotransferase [AST], alkaline phosphatase, and total bilirubin) and assessing the patient is recommended before initiating ACTOS therapy. In patients with abnormal liver tests, ACTOS should be initiated with caution.
- Measure liver tests promptly in patients who report symptoms that may indicate liver injury, including fatigue, anorexia, right upper abdominal discomfort, dark urine or jaundice. In this clinical context, if the patient is found to have abnormal liver tests (ALT greater than 3 times the upper limit of the reference range), ACTOS treatment should be interrupted and investigation done to establish the probable cause. ACTOS should not be restarted in these patients without another explanation for the liver test abnormalities.
- Patients who have serum ALT greater than three times the reference range with serum total bilirubin greater than two times the reference range without alternative etiologies are at risk for severe drug-induced liver injury, and should not be restarted on ACTOS. For patients with lesser elevations of serum ALT or bilirubin and with an alternate probable cause, treatment with ACTOS can be used with caution.
- Urinary Bladder Tumors
- Tumors were observed in the urinary bladder of male rats in the two-year carcinogenicity study. In two 3-year trials in which ACTOS was compared to placebo or glyburide, there were 16/3656 (0.44%) reports of bladder cancer in patients taking ACTOS compared to 5/3679 (0.14%) in patients not taking ACTOS. After excluding patients in whom exposure to study drug was less than one year at the time of diagnosis of bladder cancer, there were six (0.16%) cases on ACTOS and two (0.05%) cases on placebo.
- A five-year interim report of an ongoing 10-year observational cohort study found a non-significant increase in the risk for bladder cancer in subjects ever exposed to ACTOS, compared to subjects never exposed to ACTOS (HR 1.2 [95% CI 0.9 –1.5]). Compared to never exposure, a duration of ACTOS therapy longer than 12 months was associated with an increase in risk (HR 1.4 [95% CI 0.9 –2.1]), which reached statistical significance after more than 24 months of ACTOS use (HR 1.4 [95% CI 1.03 –2.0]). Interim results from this study suggested that taking ACTOS longer than 12 months increased the relative risk of developing bladder cancer in any given year by 40% which equates to an absolute increase of three cases in 10,000 (from approximately seven in 10,000 [without ACTOS] to approximately 10 in 10,000 [with ACTOS]).
- There are insufficient data to determine whether pioglitazone is a tumor promoter for urinary bladder tumors. Consequently, ACTOS should not be used in patients with active bladder cancer and the benefits of glycemic control versus unknown risks for cancer recurrence with ACTOS should be considered in patients with a prior history of bladder cancer.
- Edema
- In controlled clinical trials, edema was reported more frequently in patients treated with ACTOS than in placebo-treated patients and is dose-related. In postmarketing experience, reports of new onset or worsening edema have been received.
- ACTOS should be used with caution in patients with edema. Because thiazolidinediones, including ACTOS, can cause fluid retention, which can exacerbate or lead to congestive heart failure, ACTOS should be used with caution in patients at risk for congestive heart failure. Patients treated with ACTOS should be monitored for signs and symptoms of congestive heart failure.
- Fractures
- In PROactive (the Prospective Pioglitazone Clinical Trial in Macrovascular Events), 5238 patients with type 2 diabetes and a history of macrovascular disease were randomized to ACTOS (N=2605), force-titrated up to 45 mg daily or placebo (N=2633) in addition to standard of care. During a mean follow-up of 34.5 months, the incidence of bone fracture in females was 5.1% (44/870) for ACTOS versus 2.5% (23/905) for placebo. This difference was noted after the first year of treatment and persisted during the course of the study. The majority of fractures observed in female patients were nonvertebral fractures including lower limb and distal upper limb. No increase in the incidence of fracture was observed in men treated with ACTOS (1.7%) versus placebo (2.1%). The risk of fracture should be considered in the care of patients, especially female patients, treated with ACTOS and attention should be given to assessing and maintaining bone health according to current standards of care.
- Macular Edema
- Macular edema has been reported in postmarketing experience in diabetic patients who were taking ACTOS or another thiazolidinedione. Some patients presented with blurred vision or decreased visual acuity, but others were diagnosed on routine ophthalmologic examination.
- Most patients had peripheral edema at the time macular edema was diagnosed. Some patients had improvement in their macular edema after discontinuation of the thiazolidinedione.
- Patients with diabetes should have regular eye exams by an ophthalmologist according to current standards of care. Patients with diabetes who report any visual symptoms should be promptly referred to an ophthalmologist, regardless of the patient's underlying medications or other physical findings.
- Ovulation
- Therapy with ACTOS, like other thiazolidinediones, may result in ovulation in some premenopausal anovulatory women. As a result, these patients may be at an increased risk for pregnancy while taking ACTOS. This effect has not been investigated in clinical trials, so the frequency of this occurrence is not known. Adequate contraception in all premenopausal women treated with ACTOS is recommended.
- Macrovascular Outcomes
- There have been no clinical studies establishing conclusive evidence of macrovascular risk reduction with ACTOS or any other antidiabetic drug.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- Over 8500 patients with type 2 diabetes have been treated with ACTOS in randomized, double-blind, controlled clinical trials, including 2605 patients with type 2 diabetes and macrovascular disease treated with ACTOS in the PROactive clinical trial. In these trials, over 6000 patients have been treated with ACTOS for six months or longer, over 4500 patients have been treated with ACTOS for one year or longer, and over 3000 patients have been treated with ACTOS for at least two years.
- In six pooled 16- to 26-week placebo-controlled monotherapy and 16- to 24-week add-on combination therapy trials, the incidence of withdrawals due to adverse events was 4.5% for patients treated with ACTOS and 5.8% for comparator-treated patients. The most common adverse events leading to withdrawal were related to inadequate glycemic control, although the incidence of these events was lower (1.5%) with ACTOS than with placebo (3.0%).
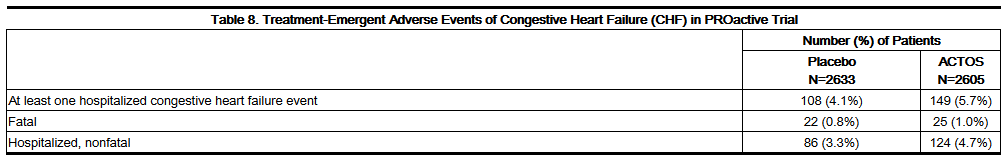
- In the PROactive trial, the incidence of withdrawals due to adverse events was 9.0% for patients treated with ACTOS and 7.7% for placebo-treated patients. Congestive heart failure was the most common serious adverse event leading to withdrawal occurring in 1.3% of patients treated with ACTOS and 0.6% of patients treated with placebo.
- Common Adverse Events: 16- to 26-Week Monotherapy Trials
- A summary of the incidence and type of common adverse events reported in three pooled 16- to 26-week placebo-controlled monotherapy trials of ACTOS is provided in Table 1. Terms that are reported represent those that occurred at an incidence of >5% and more commonly in patients treated with ACTOS than in patients who received placebo. None of these adverse events were related to ACTOS dose.
- Common Adverse Events: 16- to 24-Week Add-on Combination Therapy Trials
- A summary of the overall incidence and types of common adverse events reported in trials of ACTOS add-on to sulfonylurea is provided in Table 2. Terms that are reported represent those that occurred at an incidence of >5% and more commonly with the highest tested dose of ACTOS.
- A summary of the overall incidence and types of common adverse events reported in trials of ACTOS add-on to metformin is provided in Table 3. Terms that are reported represent those that occurred at an incidence of >5% and more commonly with the highest tested dose of ACTOS.
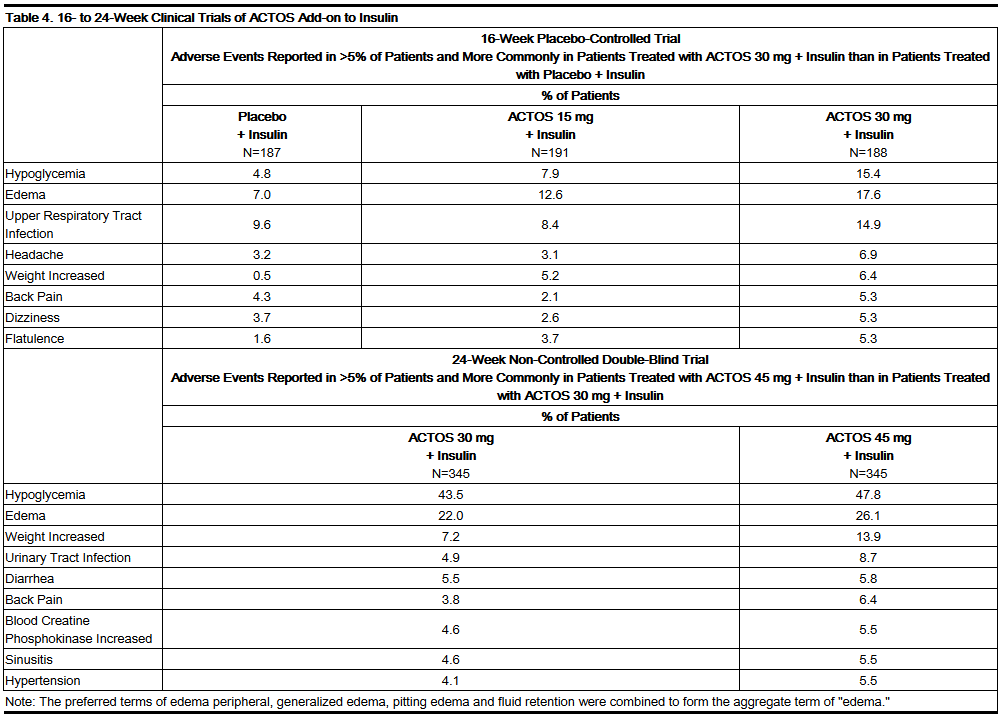
- Table 4 summarizes the incidence and types of common adverse events reported in trials of ACTOS add-on to insulin. Terms that are reported represent those that occurred at an incidence of >5% and more commonly with the highest tested dose of ACTOS.
- A summary of the overall incidence and types of common adverse events reported in the PROactive trial is provided in Table 5. Terms that are reported represent those that occurred at an incidence of >5% and more commonly in patients treated with ACTOS than in patients who received placebo.
- Congestive Heart Failure
- A summary of the incidence of adverse events related to congestive heart failure is provided in Table 6 for the 16- to 24-week add-on to sulfonylurea trials, for the 16- to 24-week add-on to insulin trials, and for the 16- to 24-week add-on to metformin trials. None of the events were fatal.
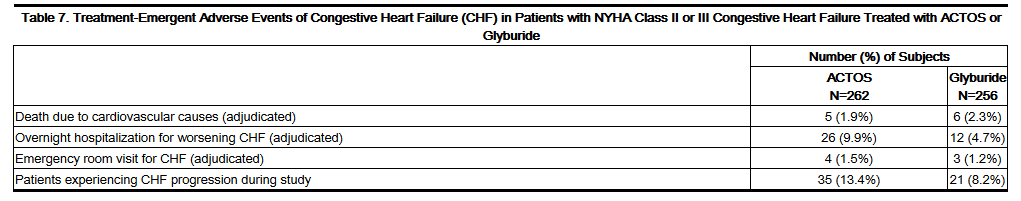
- Patients with type 2 diabetes and NYHA class II or early class III congestive heart failure were randomized to receive 24 weeks of double-blind treatment with either ACTOS at daily doses of 30 mg to 45 mg (n=262) or glyburide at daily doses of 10 mg to 15 mg (n=256). A summary of the incidence of adverse events related to congestive heart failure reported in this study is provided in Table 7.
- Congestive heart failure events leading to hospitalization that occurred during the PROactive trial are summarized in Table 8.
- Cardiovascular Safety
- In the PROactive trial, 5238 patients with type 2 diabetes and a history of macrovascular disease were randomized to ACTOS (N=2605), force-titrated up to 45 mg daily or placebo (N=2633) in addition to standard of care. Almost all patients (95%) were receiving cardiovascular medications (beta blockers, ACE inhibitors, angiotensin II receptor blockers, calcium channel blockers, nitrates, diuretics, aspirin, statins and fibrates). At baseline, patients had a mean age of 62 years, mean duration of diabetes of 9.5 years, and mean HbA1c of 8.1%. Mean duration of follow-up was 34.5 months.
- The primary objective of this trial was to examine the effect of ACTOS on mortality and macrovascular morbidity in patients with type 2 diabetes mellitus who were at high risk for macrovascular events. The primary efficacy variable was the time to the first occurrence of any event in a cardiovascular composite endpoint that included all-cause mortality, nonfatal myocardial infarction (MI) including silent MI, stroke, acute coronary syndrome, cardiac intervention including coronary artery bypass grafting or percutaneous intervention, major leg amputation above the ankle, and bypass surgery or revascularization in the leg. A total of 514 (19.7%) patients treated with ACTOS and 572 (21.7%) placebo-treated patients experienced at least one event from the primary composite endpoint (hazard ratio 0.90; 95% Confidence Interval: 0.80, 1.02; p=0.10).
- Although there was no statistically significant difference between ACTOS and placebo for the three-year incidence of a first event within this composite, there was no increase in mortality or in total macrovascular events with ACTOS. The number of first occurrences and total individual events contributing to the primary composite endpoint is shown in Table 9.
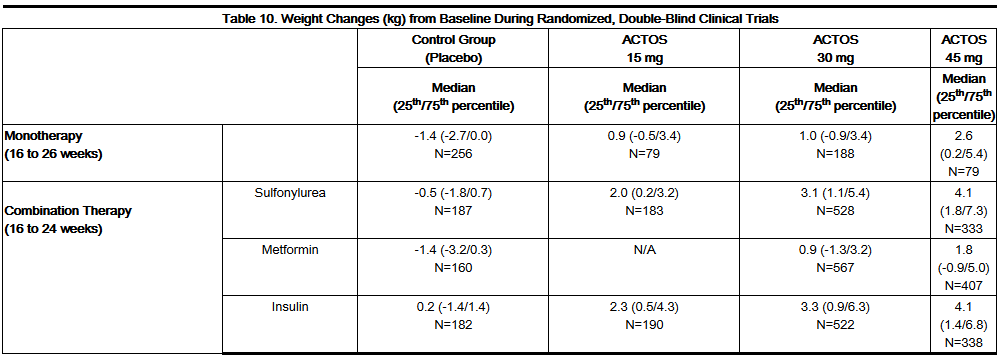
- Weight Gain
- Dose-related weight gain occurs when ACTOS is used alone or in combination with other antidiabetic medications. The mechanism of weight gain is unclear but probably involves a combination of fluid retention and fat accumulation.
- Tables 10 and 11 summarize the changes in body weight with ACTOS and placebo in the 16- to 26-week randomized, double-blind monotherapy and 16- to 24-week combination add-on therapy trials and in the PROactive trial.
- Edema
- Edema induced from taking ACTOS is reversible when ACTOS is discontinued. The edema usually does not require hospitalization unless there is coexisting congestive heart failure. A summary of the frequency and types of edema adverse events occurring in clinical investigations of ACTOS is provided in Table 12.
- Hepatic Effects
- There has been no evidence of induced hepatotoxicity with ACTOS in the ACTOS controlled clinical trial database to date. One randomized, double-blind 3-year trial comparing ACTOS to glyburide as add-on to metformin and insulin therapy was specifically designed to evaluate the incidence of serum ALT elevation to greater than three times the upper limit of the reference range, measured every eight weeks for the first 48 weeks of the trial then every 12 weeks thereafter. A total of 3/1051 (0.3%) patients treated with ACTOS and 9/1046 (0.9%) patients treated with glyburide developed ALT values greater than three times the upper limit of the reference range. None of the patients treated with ACTOS in the ACTOS controlled clinical trial database to date have had a serum ALT greater than three times the upper limit of the reference range and a corresponding total bilirubin greater than two times the upper limit of the reference range, a combination predictive of the potential for severe drug-induced liver injury.
- Hypoglycemia
- In the ACTOS clinical trials, adverse events of hypoglycemia were reported based on clinical judgment of the investigators and did not require confirmation with fingerstick glucose testing.
- In the 16-week add-on to sulfonylurea trial, the incidence of reported hypoglycemia was 3.7% with ACTOS 30 mg and 0.5% with placebo. In the 16-week add-on to insulin trial, the incidence of reported hypoglycemia was 7.9% with ACTOS 15 mg, 15.4% with ACTOS 30 mg, and 4.8% with placebo.
- The incidence of reported hypoglycemia was higher with ACTOS 45 mg compared to ACTOS 30 mg in both the 24-week add-on to sulfonylurea trial (15.7% vs. 13.4%) and in the 24-week add-on to insulin trial (47.8% vs. 43.5%).
- Three patients in these four trials were hospitalized due to hypoglycemia. All three patients were receiving ACTOS 30 mg (0.9%) in the 24-week add-on to insulin trial. An additional 14 patients reported severe hypoglycemia (defined as causing considerable interference with patient's usual activities) that did not require hospitalization. These patients were receiving ACTOS 45 mg in combination with sulfonylurea (n=2) or ACTOS 30 mg or 45 mg in combination with insulin (n=12).
- Urinary Bladder Tumors
- Tumors were observed in the urinary bladder of male rats in the two-year carcinogenicity study. In two 3-year trials in which ACTOS was compared to placebo or glyburide, there were 16/3656 (0.44%) reports of bladder cancer in patients taking ACTOS compared to 5/3679 (0.14%) in patients not taking ACTOS. After excluding patients in whom exposure to study drug was less than one year at the time of diagnosis of bladder cancer, there were six (0.16%) cases on ACTOS and two (0.05%) cases on placebo. There are too few events of bladder cancer to establish causality.
- Laboratory Abnormalities
- Hematologic Effects
- ACTOS may cause decreases in hemoglobin and hematocrit. In placebo-controlled monotherapy trials, mean hemoglobin values declined by 2% to 4% in patients treated with ACTOS compared with a mean change in hemoglobin of -1% to +1% in placebo-treated patients. These changes primarily occurred within the first 4 to 12 weeks of therapy and remained relatively constant thereafter. These changes may be related to increased plasma volume associated with ACTOS therapy and are not likely to be associated with any clinically significant hematologic effects.
- Creatine Phosphokinase
- During protocol-specified measurement of serum creatine phosphokinase (CPK) in ACTOS clinical trials, an isolated elevation in CPK to greater than 10 times the upper limit of the reference range was noted in nine (0.2%) patients treated with ACTOS (values of 2150 to 11400 IU/L) and in no comparator-treated patients. Six of these nine patients continued to receive ACTOS, two patients were noted to have the CPK elevation on the last day of dosing and one patient discontinued ACTOS due to the elevation. These elevations resolved without any apparent clinical sequelae. The relationship of these events to ACTOS therapy is unknown.
Postmarketing Experience
- The following adverse reactions have been identified during post-approval use of ACTOS. Because these reactions are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- New onset or worsening diabetic macular edema with decreased visual acuity.
- Fatal and nonfatal hepatic failure.
- Postmarketing reports of congestive heart failure have been reported in patients treated with ACTOS, both with and without previously known heart disease and both with and without concomitant insulin administration.
- In postmarketing experience, there have been reports of unusually rapid increases in weight and increases in excess of that generally observed in clinical trials. Patients who experience such increases should be assessed for fluid accumulation and volume-related events such as excessive edema and congestive heart failure.
Drug Interactions
- Strong CYP2C8 Inhibitors
- An inhibitor of CYP2C8 (e.g., gemfibrozil) significantly increases the exposure (area under the serum concentration-time curve or AUC) and half-life (t1/2) of pioglitazone. Therefore, the maximum recommended dose of ACTOS is 15 mg daily if used in combination with gemfibrozil or other strong CYP2C8 inhibitors.
- CYP2C8 Inducers
- An inducer of CYP2C8 (e.g., rifampin) may significantly decrease the exposure (AUC) of pioglitazone. Therefore, if an inducer of CYP2C8 is started or stopped during treatment with ACTOS, changes in diabetes treatment may be needed based on clinical response without exceeding the maximum recommended daily dose of 45 mg for ACTOS.
Use in Specific Populations
Pregnancy
- Pregnancy Category C
- There are no adequate and well-controlled studies of ACTOS in pregnant women. Animal studies show increased rates of post-implantation loss, delayed development, reduced fetal weights, and delayed parturition at doses 10 to 40 times the maximum recommended human dose. ACTOS should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Clinical Considerations
- Abnormal blood glucose concentrations during pregnancy are associated with a higher incidence of congenital anomalies, as well as increased neonatal morbidity and mortality. Most experts recommend the use of insulin during pregnancy to maintain blood glucose concentrations as close to normal as possible for patients with diabetes.
- Animal Data
- In animal reproductive studies, pregnant rats and rabbits received pioglitazone at doses up to approximately 17 (rat) and 40 (rabbit) times the maximum recommended human oral dose (MRHD) based on body surface area (mg/m2); no teratogenicity was observed. Increases in embryotoxicity (increased postimplantation losses, delayed development, reduced fetal weights, and delayed parturition) occurred in rats that received oral doses approximately 10 or more times the MRHD (mg/m2 basis). No functional or behavioral toxicity was observed in rat offspring. When pregnant rats received pioglitazone during late gestation and lactation, delayed postnatal development, attributed to decreased body weight, occurred in rat offspring at oral maternal doses approximately two or more times the MRHD (mg/m2 basis). In rabbits, embryotoxicity occurred at oral doses approximately 40 times the MRHD (mg/m2 basis).
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Pioglitazone in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Pioglitazone during labor and delivery.
Nursing Mothers
- It is not known whether ACTOS is secreted in human milk. Pioglitazone is secreted in the milk of lactating rats. Because many drugs are excreted in human milk, and because of the potential for ACTOS to cause serious adverse reactions in nursing infants, a decision should be made to discontinue nursing or discontinue ACTOS, taking into account the importance of ACTOS to the mother.
Pediatric Use
- Safety and effectiveness of ACTOS in pediatric patients have not been established.
- ACTOS is not recommended for use in pediatric patients based on adverse effects observed in adults, including fluid retention and congestive heart failure, fractures, and urinary bladder tumors.
Geriatic Use
- A total of 92 patients (15.2%) treated with ACTOS in the three pooled 16- to 26-week double-blind, placebo-controlled, monotherapy trials were ≥65 years old and two patients (0.3%) were ≥75 years old. In the two pooled 16- to 24-week add-on to sulfonylurea trials, 201 patients (18.7%) treated with ACTOS were ≥65 years old and 19 (1.8%) were ≥75 years old. In the two pooled 16- to 24-week add-on to metformin trials, 155 patients (15.5%) treated with ACTOS were ≥65 years old and 19 (1.9%) were ≥75 years old. In the two pooled 16- to 24-week add-on to insulin trials, 272 patients (25.4%) treated with ACTOS were ≥65 years old and 22 (2.1%) were ≥75 years old.
- In PROactive, 1068 patients (41.0%) treated with ACTOS were ≥65 years old and 42 (1.6%) were ≥75 years old.
- In pharmacokinetic studies with pioglitazone, no significant differences were observed in pharmacokinetic parameters between elderly and younger patients.
- Although clinical experiences have not identified differences in effectiveness and safety between the elderly (≥65 years) and younger patients, these conclusions are limited by small sample sizes for patients ≥75 years old.
Gender
There is no FDA guidance on the use of Pioglitazone with respect to specific gender populations.
Race
There is no FDA guidance on the use of Pioglitazone with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Pioglitazone in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Pioglitazone in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Pioglitazone in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Pioglitazone in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
- After initiation of ACTOS, and after dose increases, monitor patients carefully for signs and symptoms of heart failure (e.g., excessive, rapid weight gain, dyspnea, and/or edema). If heart failure develops, it should be managed according to current standards of care and discontinuation or dose reduction of ACTOS must be considered.
IV Compatibility
There is limited information regarding IV Compatibility of Pioglitazone in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- During controlled clinical trials, one case of overdose with ACTOS was reported. A male patient took 120 mg per day for four days, then 180 mg per day for seven days. The patient denied any clinical symptoms during this period.
Management
- In the event of overdosage, appropriate supportive treatment should be initiated according to the patient's clinical signs and symptoms.
Chronic Overdose
There is limited information regarding Chronic Overdose of Pioglitazone in the drug label.
Pharmacology
| |
1 : 1 mixture (racemate)Pioglitazone
| |
| Systematic (IUPAC) name | |
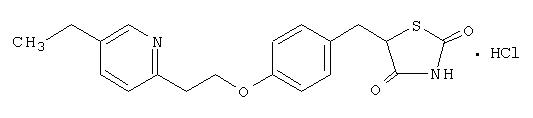
| (RS)-5-(4-[2-(5-ethylpyridin-2-yl)ethoxy]benzyl)thiazolidine-2,4-dione | |
| Identifiers | |
| CAS number | |
| ATC code | A10 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 356.44 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Protein binding | >99% |
| Metabolism | liver (CYP2C8) |
| Half life | 3–7 hours |
| Excretion | in bile |
| Therapeutic considerations | |
| Licence data |
, |
| Pregnancy cat. |
C |
| Legal status |
POM(UK) [[Prescription drug|Template:Unicode-only]](US) |
| Routes | oral |
Mechanism of Action
- ACTOS is a thiazolidinedione that depends on the presence of insulin for its mechanism of action. ACTOS decreases insulin resistance in the periphery and in the liver resulting in increased insulin-dependent glucose disposal and decreased hepatic glucose output. Pioglitazone is not an insulin secretagogue. Pioglitazone is an agonist for peroxisome proliferator-activated receptor-gamma (PPARγ). PPAR receptors are found in tissues important for insulin action such as adipose tissue, skeletal muscle, and liver. Activation of PPARγ nuclear receptors modulates the transcription of a number of insulin responsive genes involved in the control of glucose and lipid metabolism.
- In animal models of diabetes, pioglitazone reduces the hyperglycemia, hyperinsulinemia, and hypertriglyceridemia characteristic of insulin-resistant states such as type 2 diabetes. The metabolic changes produced by pioglitazone result in increased responsiveness of insulin-dependent tissues and are observed in numerous animal models of insulin resistance.
- Because pioglitazone enhances the effects of circulating insulin (by decreasing insulin resistance), it does not lower blood glucose in animal models that lack endogenous insulin.
Structure
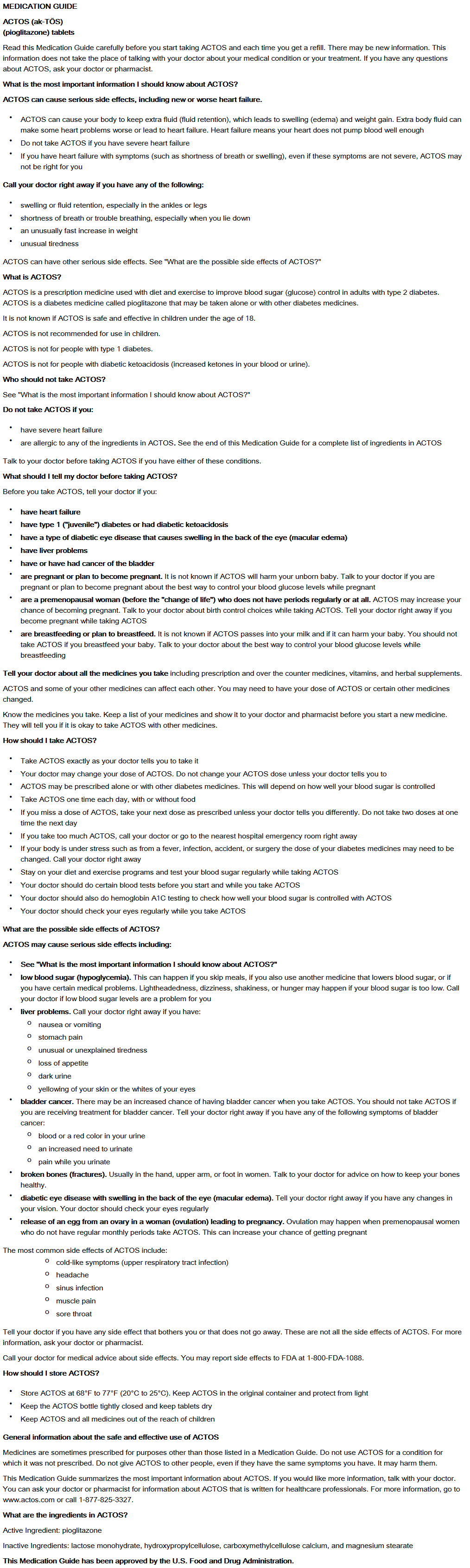
- ACTOS tablets are a thiazolidinedione and an agonist for peroxisome proliferator-activated receptor (PPAR) gamma that contains an oral antidiabetic medication: pioglitazone.
- Pioglitazone [(±)-5-[4-[2-(5-ethyl-2-pyridinyl) ethoxy] phenyl] methyl]-2,4-] thiazolidinedione monohydrochloride contains one asymmetric carbon, and the compound is synthesized and used as the racemic mixture. The two enantiomers of pioglitazone interconvert in vivo. No differences were found in the pharmacologic activity between the two enantiomers. The structural formula is as shown:
- Pioglitazone hydrochloride is an odorless white crystalline powder that has a molecular formula of C19H20N2O3S•HCl and a molecular weight of 392.90 daltons. It is soluble in N,N-dimethylformamide, slightly soluble in anhydrous ethanol, very slightly soluble in acetone and acetonitrile, practically insoluble in water, and insoluble in ether.
- ACTOS is available as a tablet for oral administration containing 15 mg, 30 mg, or 45 mg of pioglitazone (as the base) formulated with the following excipients: lactose monohydrate NF, hydroxypropylcellulose NF, carboxymethylcellulose calcium NF, and magnesium stearate NF.
Pharmacodynamics
- Clinical studies demonstrate that ACTOS improves insulin sensitivity in insulin-resistant patients. ACTOS enhances cellular responsiveness to insulin, increases insulin-dependent glucose disposal and improves hepatic sensitivity to insulin. In patients with type 2 diabetes, the decreased insulin resistance produced by ACTOS results in lower plasma glucose concentrations, lower plasma insulin concentrations, and lower HbA1c values. In controlled clinical trials, ACTOS had an additive effect on glycemic control when used in combination with a sulfonylurea, metformin, or insulin.
- Patients with lipid abnormalities were included in clinical trials with ACTOS. Overall, patients treated with ACTOS had mean decreases in serum triglycerides, mean increases in HDL cholesterol, and no consistent mean changes in LDL and total cholesterol. There is no conclusive evidence of macrovascular benefit with ACTOS or any other antidiabetic medication.
- In a 26-week, placebo-controlled, dose-ranging monotherapy study, mean serum triglycerides decreased in the 15 mg, 30 mg, and 45 mg ACTOS dose groups compared to a mean increase in the placebo group. Mean HDL cholesterol increased to a greater extent in patients treated with ACTOS than in the placebo-treated patients. There were no consistent differences for LDL and total cholesterol in patients treated with ACTOS compared to placebo (see Table 14).
- In the two other monotherapy studies (16 weeks and 24 weeks) and in combination therapy studies with sulfonylurea (16 weeks and 24 weeks), metformin (16 weeks and 24 weeks) or insulin (16 weeks and 24 weeks), the results were generally consistent with the data above.
Pharmacokinetics
- Following once-daily administration of ACTOS, steady-state serum concentrations of both pioglitazone and its major active metabolites, M-III (keto derivative of pioglitazone) and M-IV (hydroxyl derivative of pioglitazone), are achieved within seven days. At steady-state, M-III and M-IV reach serum concentrations equal to or greater than that of pioglitazone. At steady-state, in both healthy volunteers and patients with type 2 diabetes, pioglitazone comprises approximately 30% to 50% of the peak total pioglitazone serum concentrations (pioglitazone plus active metabolites) and 20% to 25% of the total AUC.
- Cmax, AUC, and trough serum concentrations (Cmin) for pioglitazone and M-III and M-IV, increased proportionally with administered doses of 15 mg and 30 mg per day.
- Absorption
- Following oral administration of pioglitazone, Tmax of pioglitazone was within two hours. Food delays the Tmax to three to four hours but does not alter the extent of absorption (AUC).
- Distribution
- The mean apparent volume of distribution (Vd/F) of pioglitazone following single-dose administration is 0.63 ± 0.41 (mean ± SD) L/kg of body weight. Pioglitazone is extensively protein bound (>99%) in human serum, principally to serum albumin. Pioglitazone also binds to other serum proteins, but with lower affinity. M-III and M-IV are also extensively bound (>98%) to serum albumin.
- Metabolism
- Pioglitazone is extensively metabolized by hydroxylation and oxidation; the metabolites also partly convert to glucuronide or sulfate conjugates. Metabolites M-III and M-IV are the major circulating active metabolites in humans.
- In vitro data demonstrate that multiple CYP isoforms are involved in the metabolism of pioglitazone, which include CYP2C8 and, to a lesser degree, CYP3A4 with additional contributions from a variety of other isoforms including the mainly extrahepatic CYP1A1. In vivo study of pioglitazone in combination with gemfibrozil, a strong CYP2C8 inhibitor, showed that pioglitazone is a CYP2C8 substrate. Urinary 6ß-hydroxycortisol/cortisol ratios measured in patients treated with ACTOS showed that pioglitazone is not a strong CYP3A4 enzyme inducer.
- Excretion and Elimination
- Following oral administration, approximately 15% to 30% of the pioglitazone dose is recovered in the urine. Renal elimination of pioglitazone is negligible, and the drug is excreted primarily as metabolites and their conjugates. It is presumed that most of the oral dose is excreted into the bile either unchanged or as metabolites and eliminated in the feces.
- The mean serum half-life (t1/2) of pioglitazone and its metabolites (M-III and M-IV) range from three to seven hours and 16 to 24 hours, respectively. Pioglitazone has an apparent clearance, CL/F, calculated to be five to seven L/hr.
- Renal Impairment
- The serum elimination half-life of pioglitazone, M-III, and M-IV remains unchanged in patients with moderate (creatinine clearance [CLcr] 30 to 50 mL/min) and severe (CLcr <30 mL/min) renal impairment when compared to subjects with normal renal function. Therefore, no dose adjustment in patients with renal impairment is required.
- Hepatic Impairment
- Compared with healthy controls, subjects with impaired hepatic function (Child-Turcotte-Pugh Grade B/C) have an approximate 45% reduction in pioglitazone and total pioglitazone (pioglitazone, M-III, and M-IV) mean Cmax but no change in the mean AUC values. Therefore, no dose adjustment in patients with hepatic impairment is required.
- There are postmarketing reports of liver failure with ACTOS and clinical trials have generally excluded patients with serum ALT >2.5 times the upper limit of the reference range. Use caution in patients with liver disease.
- Geriatric Patients
- In healthy elderly subjects, Cmax of pioglitazone was not significantly different, but AUC values were approximately 21% higher than those achieved in younger subjects. The mean t1/2 of pioglitazone was also prolonged in elderly subjects (about ten hours) as compared to younger subjects (about seven hours). These changes were not of a magnitude that would be considered clinically relevant.
- Pediatric Patients
- Safety and efficacy of pioglitazone in pediatric patients have not been established. ACTOS is not recommended for use in pediatric patients.
- Gender
- The mean Cmax and AUC values of pioglitazone were increased 20% to 60% in women compared to men. In controlled clinical trials, HbA1c decreases from baseline were generally greater for females than for males (average mean difference in HbA1c 0.5%). Because therapy should be individualized for each patient to achieve glycemic control, no dose adjustment is recommended based on gender alone.
- Ethnicity
- Pharmacokinetic data among various ethnic groups are not available.
- Drug-Drug Interactions
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- A two-year carcinogenicity study was conducted in male and female rats at oral doses up to 63 mg/kg (approximately 14 times the maximum recommended human oral dose of 45 mg based on mg/m2). Drug-induced tumors were not observed in any organ except for the urinary bladder of male rats. Benign and/or malignant transitional cell neoplasms were observed in male rats at 4 mg/kg/day and above (approximately equal to the maximum recommended human oral dose based on mg/m2). Urinary calculi with subsequent irritation and hyperplasia were postulated as the mechanism for bladder tumors observed in male rats. A two-year mechanistic study in male rats utilizing dietary acidification to reduce calculi formation was completed in 2009. Dietary acidification decreased but did not abolish the hyperplastic changes in the bladder. The presence of calculi exacerbated the hyperplastic response to pioglitazone but was not considered the primary cause of the hyperplastic changes.
- The relevance to humans of the bladder findings in the male rat cannot be excluded.
- A two-year carcinogenicity study was also conducted in male and female mice at oral doses up to 100 mg/kg/day (approximately 11 times the maximum recommended human oral dose based on mg/m2). No drug-induced tumors were observed in any organ.
- Pioglitazone hydrochloride was not mutagenic in a battery of genetic toxicology studies, including the Ames bacterial assay, a mammalian cell forward gene mutation assay (CHO/HPRT and AS52/XPRT), an in vitro cytogenetics assay using CHL cells, an unscheduled DNA synthesis assay, and an in vivo micronucleus assay.
- No adverse effects upon fertility were observed in male and female rats at oral doses up to 40 mg/kg pioglitazone hydrochloride daily prior to and throughout mating and gestation (approximately nine times the maximum recommended human oral dose based on mg/m2).
Animal Toxicology and/or Pharmacology
- Heart enlargement has been observed in mice (100 mg/kg), rats (4 mg/kg and above) and dogs (3 mg/kg) treated orally with pioglitazone hydrochloride (approximately 11, 1, and 2 times the maximum recommended human oral dose for mice, rats, and dogs, respectively, based on mg/m2). In a one-year rat study, drug-related early death due to apparent heart dysfunction occurred at an oral dose of 160 mg/kg/day (approximately 35 times the maximum recommended human oral dose based on mg/m2). Heart enlargement was seen in a 13-week study in monkeys at oral doses of 8.9 mg/kg and above (approximately four times the maximum recommended human oral dose based on mg/m2), but not in a 52-week study at oral doses up to 32 mg/kg (approximately 13 times the maximum recommended human oral dose based on mg/m2).
Clinical Studies
- Monotherapy
- Three randomized, double-blind, placebo-controlled trials with durations from 16 to 26 weeks were conducted to evaluate the use of ACTOS as monotherapy in patients with type 2 diabetes. These trials examined ACTOS at doses up to 45 mg or placebo once daily in a total of 865 patients.
- In a 26-week dose-ranging monotherapy trial, 408 patients with type 2 diabetes were randomized to receive 7.5 mg, 15 mg, 30 mg, or 45 mg of ACTOS, or placebo once daily. Therapy with any previous antidiabetic agent was discontinued eight weeks prior to the double-blind period. Treatment with 15 mg, 30 mg, and 45 mg of ACTOS produced statistically significant improvements in HbA1c and fasting plasma glucose (FPG) at endpoint compared to placebo (see Figure 1, Table 17).
- Figure 1 shows the time course for changes in HbA1c in this 26-week study.
- In a 24-week placebo-controlled monotherapy trial, 260 patients with type 2 diabetes were randomized to one of two forced-titration ACTOS treatment groups or a mock-titration placebo group. Therapy with any previous antidiabetic agent was discontinued six weeks prior to the double-blind period. In one ACTOS treatment group, patients received an initial dose of 7.5 mg once daily. After four weeks, the dose was increased to 15 mg once daily and after another four weeks, the dose was increased to 30 mg once daily for the remainder of the trial (16 weeks). In the second ACTOS treatment group, patients received an initial dose of 15 mg once daily and were titrated to 30 mg once daily and 45 mg once daily in a similar manner. Treatment with ACTOS, as described, produced statistically significant improvements in HbA1c and FPG at endpoint compared to placebo (see Table 18).
- In a 16-week monotherapy trial, 197 patients with type 2 diabetes were randomized to treatment with 30 mg of ACTOS or placebo once daily. Therapy with any previous antidiabetic agent was discontinued six weeks prior to the double-blind period. Treatment with 30 mg of ACTOS produced statistically significant improvements in HbA1c and FPG at endpoint compared to placebo (see Table 19).
- Combination Therapy
- Three 16-week, randomized, double-blind, placebo-controlled clinical trials were conducted to evaluate the effects of ACTOS (15 mg and/or 30 mg) on glycemic control in patients with type 2 diabetes who were inadequately controlled (HbA1c ≥8%) despite current therapy with a sulfonylurea, metformin, or insulin. In addition, three 24-week randomized, double-blind clinical trials were conducted to evaluate the effects of ACTOS 30 mg vs. ACTOS 45 mg on glycemic control in patients with type 2 diabetes who were inadequately controlled (HbA1c ≥8%) despite current therapy with a sulfonylurea, metformin, or insulin. Previous diabetes treatment may have been monotherapy or combination therapy.
- Add-on to Sulfonylurea Trials
- Two clinical trials were conducted with ACTOS in combination with a sulfonylurea. Both studies included patients with type 2 diabetes on any dose of a sulfonylurea, either alone or in combination with another antidiabetic agent. All other antidiabetic agents were withdrawn at least three weeks prior to starting study treatment.
- In the first study, 560 patients were randomized to receive 15 mg or 30 mg of ACTOS or placebo once daily for 16 weeks in addition to their current sulfonylurea regimen. Treatment with ACTOS as add-on to sulfonylurea produced statistically significant improvements in HbA1c and FPG at endpoint compared to placebo add-on to sulfonylurea (see Table 20).
- In the second trial, 702 patients were randomized to receive 30 mg or 45 mg of ACTOS once daily for 24 weeks in addition to their current sulfonylurea regimen. The mean reduction from baseline at Week 24 in HbA1c was 1.6% for the 30 mg dose and 1.7% for the 45 mg dose (see Table 21). The mean reduction from baseline at Week 24 in FPG was 52 mg/dL for the 30 mg dose and 56 mg/dL for the 45 mg dose.
- The therapeutic effect of ACTOS in combination with sulfonylurea was observed in patients regardless of the sulfonylurea dose.
- Add-on to Metformin Trials
- Two clinical trials were conducted with ACTOS in combination with metformin. Both trials included patients with type 2 diabetes on any dose of metformin, either alone or in combination with another antidiabetic agent. All other antidiabetic agents were withdrawn at least three weeks prior to starting study treatment.
- In the first trial, 328 patients were randomized to receive either 30 mg of ACTOS or placebo once daily for 16 weeks in addition to their current metformin regimen. Treatment with ACTOS as add-on to metformin produced statistically significant improvements in HbA1c and FPG at endpoint compared to placebo add-on to metformin (see Table 22).
- In the second trial, 827 patients were randomized to receive either 30 mg or 45 mg of ACTOS once daily for 24 weeks in addition to their current metformin regimen. The mean reduction from baseline at Week 24 in HbA1c was 0.8% for the 30 mg dose and 1.0% for the 45 mg dose (see Table 23). The mean reduction from baseline at Week 24 in FPG was 38 mg/dL for the 30 mg dose and 51 mg/dL for the 45 mg dose.
- The therapeutic effect of ACTOS in combination with metformin was observed in patients regardless of the metformin dose.
- Add-on to Insulin Trials
- Two clinical trials were conducted with ACTOS in combination with insulin. Both trials included patients with type 2 diabetes on insulin, either alone or in combination with another antidiabetic agent. All other antidiabetic agents were withdrawn prior to starting study treatment. In the first trial, 566 patients were randomized to receive either 15 mg or 30 mg of ACTOS or placebo once daily for 16 weeks in addition to their insulin regimen. Treatment with ACTOS as add-on to insulin produced statistically significant improvements in HbA1c and FPG at endpoint compared to placebo add-on to insulin (see Table 24). The mean daily insulin dose at baseline in each treatment group was approximately 70 units. The majority of patients (75% overall, 86% treated with placebo, 77% treated with ACTOS 15 mg, and 61% treated with ACTOS 30 mg) had no change in their daily insulin dose from baseline to the final study visit. The mean change from baseline in daily dose of insulin (including patients with no insulin dose modifications) was -3 units in the patients treated with ACTOS 15 mg, -8 units in the patients treated with ACTOS 30 mg, and -1 unit in patients treated with placebo.
- In the second trial, 690 patients receiving a median of 60 units per day of insulin were randomized to receive either 30 mg or 45 mg of ACTOS once daily for 24 weeks in addition to their current insulin regimen. The mean reduction from baseline at Week 24 in HbA1c was 1.2% for the 30 mg dose and 1.5% for the 45 mg dose. The mean reduction from baseline at Week 24 in FPG was 32 mg/dL for the 30 mg dose and 46 mg/dL for the 45 mg dose (see Table 25). The mean daily insulin dose at baseline in both treatment groups was approximately 70 units. The majority of patients (55% overall, 58% treated with ACTOS 30 mg, and 52% treated with ACTOS 45 mg) had no change in their daily insulin dose from baseline to the final study visit. The mean change from baseline in daily dose of insulin (including patients with no insulin dose modifications) was -5 units in the patients treated with ACTOS 30 mg and -8 units in the patients treated with ACTOS 45 mg.
- The therapeutic effect of ACTOS in combination with insulin was observed in patients regardless of the insulin dose.
How Supplied
- ACTOS is available in 15 mg, 30 mg, and 45 mg tablets as follows:
- 15 mg tablet: White to off-white, round, convex, nonscored tablet with "ACTOS" on one side, and "15" on the other, available in:
- NDC 64764-151-04 Bottles of 30
- NDC 64764-151-05 Bottles of 90
- NDC 64764-151-06 Bottles of 500
- 15 mg tablet: White to off-white, round, convex, nonscored tablet with "ACTOS" on one side, and "15" on the other, available in:
- 30 mg tablet: White to off-white, round, flat, nonscored tablet with "ACTOS" on one side, and "30" on the other, available in:
- NDC 64764-301-14 Bottles of 30
- NDC 64764-301-15 Bottles of 90
- NDC 64764-301-16 Bottles of 500
- 30 mg tablet: White to off-white, round, flat, nonscored tablet with "ACTOS" on one side, and "30" on the other, available in:
- 45 mg tablet: White to off-white, round, flat, nonscored tablet with "ACTOS" on one side, and "45" on the other, available in:
- NDC 64764-451-24 Bottles of 30
- NDC 64764-451-25 Bottles of 90
- NDC 64764-451-26 Bottles of 500
- 45 mg tablet: White to off-white, round, flat, nonscored tablet with "ACTOS" on one side, and "45" on the other, available in:
- Storage
- Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F). Keep container tightly closed, and protect from light, moisture and humidity.
Storage
There is limited information regarding Pioglitazone Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Pioglitazone |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
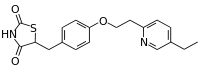
Package and Label Display Panel
{{#ask: Label Page::Pioglitazone |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- It is important to instruct patients to adhere to dietary instructions and to have blood glucose and glycosylated hemoglobin tested regularly. During periods of stress such as fever, trauma, infection, or surgery, medication requirements may change and patients should be reminded to seek medical advice promptly.
- Patients who experience an unusually rapid increase in weight or edema or who develop shortness of breath or other symptoms of heart failure while on ACTOS should immediately report these symptoms to a physician.
- Tell patients to promptly stop taking ACTOS and seek immediate medical advice if there is unexplained nausea, vomiting, abdominal pain, fatigue, anorexia, or dark urine as these symptoms may be due to hepatotoxicity.
- Tell patients to promptly report any sign of macroscopic hematuria or other symptoms such as dysuria or urinary urgency that develop or increase during treatment as these may be due to bladder cancer.
- Tell patients to take ACTOS once daily. ACTOS can be taken with or without meals. If a dose is missed on one day, the dose should not be doubled the following day.
- When using combination therapy with insulin or other antidiabetic medications, the risks of hypoglycemia, its symptoms and treatment, and conditions that predispose to its development should be explained to patients and their family members.
- Inform patients that therapy with ACTOS, like other thiazolidinediones, may result in ovulation in some premenopausal anovulatory women. As a result, these patients may be at an increased risk for pregnancy while taking ACTOS. Therefore, adequate contraception should be recommended for all premenopausal women who are prescribed ACTOS.
Precautions with Alcohol
- Alcohol-Pioglitazone interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Actos®[2]
Look-Alike Drug Names
- Actos® — Actonel®[3]
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK; et al. (2005). "Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial". Lancet. 366 (9493): 1279–89. doi:10.1016/S0140-6736(05)67528-9. PMID 16214598. Review in: Evid Based Med. 2006 Apr;11(2):47 Review in: ACP J Club. 2006 Mar-Apr;144(2):34
- ↑ "ACTOS (pioglitazone) tablet [Takeda Pharmaceuticals America, Inc.]".
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Pioglitazone |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Pioglitazone |Label Name=Pioglitazone27.png
}}
{{#subobject:
|Label Page=Pioglitazone |Label Name=Pioglitazone28.png
}}
{{#subobject:
|Label Page=Pioglitazone |Label Name=Pioglitazone29.png
}}
{{#subobject:
|Label Page=Pioglitazone |Label Name=Pioglitazone30.png
}}