Thymoma differential diagnosis: Difference between revisions
Sergekorjian (talk | contribs) |
No edit summary |
||
| Line 35: | Line 35: | ||
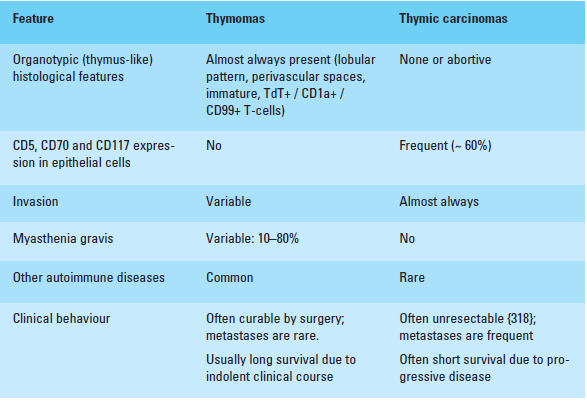
| [[File:diff.png|800px|thumb|Differential diagnosis of thymomas types A, AB, B and [[Thymic cancer|thymic carcinomas]].<ref>{{Cite web | last = | first = | title = http://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb10/BB10.pdf | url = http://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb10/BB10.pdf | publisher = | date = | accessdate = }}</ref>]] | | [[File:diff.png|800px|thumb|Differential diagnosis of thymomas types A, AB, B and [[Thymic cancer|thymic carcinomas]].<ref>{{Cite web | last = | first = | title = http://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb10/BB10.pdf | url = http://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb10/BB10.pdf | publisher = | date = | accessdate = }}</ref>]] | ||
|} | |} | ||
==Other differentials== | |||
Thymoma must be differentiated from other similar conditions which lead to multiple endocrine disorders such as [[POEMS syndrome]], Hirata syndrome, [[Kearns–Sayre syndrome]] and [[Wolfram syndrome|Wolfram syndromes]].<ref name="pmid21533467">{{cite journal |vauthors=Sherer Y, Bardayan Y, Shoenfeld Y |title=Thymoma, thymic hyperplasia, thymectomy and autoimmune diseases (Review) |journal=Int. J. Oncol. |volume=10 |issue=5 |pages=939–43 |year=1997 |pmid=21533467 |doi= |url=}}</ref><ref name="Nozza2017">{{cite journal|last1=Nozza|first1=Andrea|title=POEMS SYNDROME: AN UPDATE|journal=Mediterranean Journal of Hematology and Infectious Diseases|volume=9|issue=1|year=2017|pages=e2017051|issn=2035-3006|doi=10.4084/mjhid.2017.051}}</ref><ref name="pmid17342029">{{cite journal |vauthors=Maceluch JA, Niedziela M |title=The clinical diagnosis and molecular genetics of kearns-sayre syndrome: a complex mitochondrial encephalomyopathy |journal=Pediatr Endocrinol Rev |volume=4 |issue=2 |pages=117–37 |year=2006 |pmid=17342029 |doi= |url=}}</ref><ref name="pmid22790102">{{cite journal |vauthors=Rigoli L, Di Bella C |title=Wolfram syndrome 1 and Wolfram syndrome 2 |journal=Curr. Opin. Pediatr. |volume=24 |issue=4 |pages=512–7 |year=2012 |pmid=22790102 |doi=10.1097/MOP.0b013e328354ccdf |url=}}</ref><ref name="HusebyeAnderson2010">{{cite journal|last1=Husebye|first1=Eystein S.|last2=Anderson|first2=Mark S.|title=Autoimmune Polyendocrine Syndromes: Clues to Type 1 Diabetes Pathogenesis|journal=Immunity|volume=32|issue=4|year=2010|pages=479–487|issn=10747613|doi=10.1016/j.immuni.2010.03.016}}</ref> | |||
{| class="wikitable" | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Disease | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Addison's disease | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Type 1 diabetes mellitus | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Hypothyroidism | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Other disorders present | |||
|- | |||
|APS type 1 | |||
|<nowiki>+</nowiki> | |||
|Less common | |||
|Less common | |||
|[[Hypoparathyroidism]]<br>[[Candidiasis]]<br>[[Hypogonadism]] | |||
|- | |||
|APS type 2 | |||
| + | |||
| + | |||
| + | |||
|[[Hypogonadism]]<br>[[Malabsorption]] | |||
|- | |||
|APS type 3 | |||
|<nowiki>-</nowiki> | |||
| + | |||
|<nowiki>+</nowiki> | |||
|[[Malabsorption]] | |||
|- | |||
|[[Thymoma]] | |||
| + | |||
|<nowiki>-</nowiki> | |||
| + | |||
|[[Myasthenia gravis]]<br>[[Cushing syndrome]] | |||
|- | |||
|[[Chromosomal abnormalities]]<br>([[Turner syndrome]],<br>[[Down's syndrome]]) | |||
| - | |||
| + | |||
| + | |||
|[[Cardiac dysfunction ]] | |||
|- | |||
|[[Kearns–Sayre syndrome]] | |||
|<nowiki>-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |||
|[[Myopathy]]<br>[[Hypoparathyroidism]]<br>[[Hypogonadism]] | |||
|- | |||
|[[Wolfram syndrome]] | |||
|<nowiki>-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |||
|[[Diabetes insipidus]]<br>[[Optic atrophy]]<br>[[Deafness]]<br> | |||
|- | |||
|[[POEMS syndrome]] | |||
|<nowiki>-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |||
|[[Polyneuropathy]]<br>[[Hypogonadism]]<br>[[Plasma cell dyscrasia|Plasma cell dyscrasias]] | |||
|} | |||
==References== | ==References== | ||
Revision as of 19:57, 27 October 2017
|
Thymoma Microchapters |
|
Diagnosis |
|---|
|
Case Studies |
|
Thymoma differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Thymoma differential diagnosis |
|
Risk calculators and risk factors for Thymoma differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Amr Marawan, M.D. [2] Ahmad Al Maradni, M.D. [3]
Overview
Thymoma must be differentiated from other diseases such as thymic carcinoma, thymic cyst, thymic hyperplasia and germ cell tumors.
Differential Diagnosis
Thymoma must be differentiated from other diseases such as:
- Thymic masses
- Thymic cyst: It is an incidental mass that may be congenital or acquired. It might contain parathyroid or salivary tissue, as they have a common embryological origin.
- Thymic hyperplasia: Resected only if associated paraneoplastic syndrome.
- Thymolipoma: Increased thymic size with mixed adipose tissue.
- Thymic carcinoma: Rare thymic tumor, poor survival rate, high rate of recurrence. Sometimes called type C thymoma.
- Thymic carcinoid: Also called thymic neuroendocrine tumor, uncommon and presents as a mass in the anterior mediastinum.
- Ectopic parathyroid tissue
- Germ cell tumors
- The most common site of extragonadal germ cell tumors is the mediastinum.
- Germ cell tumors include:
- Teratomas: Represents two thirds of mediastinal germ cell tumors. Usually benign, but when malignant, it's very aggressive and has a very poor prognosis.
- Dermoid cysts: Very rare tumor, only 118 cases have been reported.[1]
- Malignant germ cell tumor: 90% of malignant mediastinal germ cell tumors occur in males. A full physical examination and scrotal ultrasound is required.
- Seminomas: Slightly more common, grows slowly but might reach large sizes.
- Non-seminomatous germ cell tumor: Consists of yolk sac tumors, embryonal cell carcinoma, and/or choriocarcinoma. Commonly occurs between 20 and 40 years of age.
- Lymphoma (anterior mediatinal lymphoma, also known as terrible lymphoma, may be middle or posterior mediastinal)
- Nodular sclerosing Hodgkin’s lymphoma and primary mediastinal B-cell lymphoma are the two common types that present in the mediastinum.
- Usually has systemic symptoms such as fever, weight loss, and night sweats and may also have other symptoms as chest pain, wheezing, dyspnea or superior vena cava syndrome.
- Thyroid (intrathyroid goiter)
- Grave's disease and Hashimoto's thyroiditis are usually associated with goiter.
- Presents with shortness of breath or dysphagia.
 |
Other differentials
Thymoma must be differentiated from other similar conditions which lead to multiple endocrine disorders such as POEMS syndrome, Hirata syndrome, Kearns–Sayre syndrome and Wolfram syndromes.[3][4][5][6][7]
| Disease | Addison's disease | Type 1 diabetes mellitus | Hypothyroidism | Other disorders present |
|---|---|---|---|---|
| APS type 1 | + | Less common | Less common | Hypoparathyroidism Candidiasis Hypogonadism |
| APS type 2 | + | + | + | Hypogonadism Malabsorption |
| APS type 3 | - | + | + | Malabsorption |
| Thymoma | + | - | + | Myasthenia gravis Cushing syndrome |
| Chromosomal abnormalities (Turner syndrome, Down's syndrome) |
- | + | + | Cardiac dysfunction |
| Kearns–Sayre syndrome | - | + | - | Myopathy Hypoparathyroidism Hypogonadism |
| Wolfram syndrome | - | + | - | Diabetes insipidus Optic atrophy Deafness |
| POEMS syndrome | - | + | - | Polyneuropathy Hypogonadism Plasma cell dyscrasias |
References
- ↑ Ripa, LW. (1992). "Rinses for the control of dental caries". Int Dent J. 42 (4 Suppl 1): 263–9. PMID 1399044. Unknown parameter
|month=ignored (help) - ↑ "http://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb10/BB10.pdf" (PDF). External link in
|title=(help) - ↑ Sherer Y, Bardayan Y, Shoenfeld Y (1997). "Thymoma, thymic hyperplasia, thymectomy and autoimmune diseases (Review)". Int. J. Oncol. 10 (5): 939–43. PMID 21533467.
- ↑ Nozza, Andrea (2017). "POEMS SYNDROME: AN UPDATE". Mediterranean Journal of Hematology and Infectious Diseases. 9 (1): e2017051. doi:10.4084/mjhid.2017.051. ISSN 2035-3006.
- ↑ Maceluch JA, Niedziela M (2006). "The clinical diagnosis and molecular genetics of kearns-sayre syndrome: a complex mitochondrial encephalomyopathy". Pediatr Endocrinol Rev. 4 (2): 117–37. PMID 17342029.
- ↑ Rigoli L, Di Bella C (2012). "Wolfram syndrome 1 and Wolfram syndrome 2". Curr. Opin. Pediatr. 24 (4): 512–7. doi:10.1097/MOP.0b013e328354ccdf. PMID 22790102.
- ↑ Husebye, Eystein S.; Anderson, Mark S. (2010). "Autoimmune Polyendocrine Syndromes: Clues to Type 1 Diabetes Pathogenesis". Immunity. 32 (4): 479–487. doi:10.1016/j.immuni.2010.03.016. ISSN 1074-7613.