|
|
| (41 intermediate revisions by 11 users not shown) |
| Line 1: |
Line 1: |
| | __NOTOC__ |
| | {| class="infobox" style="float:right;" |
| | |- |
| | | [[File:Siren.gif|link=Thrombocytopenia resident survival guide|41x41px]] |
| | | [[Thrombocytopenia resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] |
| | |} |
| | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' |
| {{Infobox_Disease | | | {{Infobox_Disease | |
| Name = Thrombocytopenia | | | Name = Thrombocytopenia | |
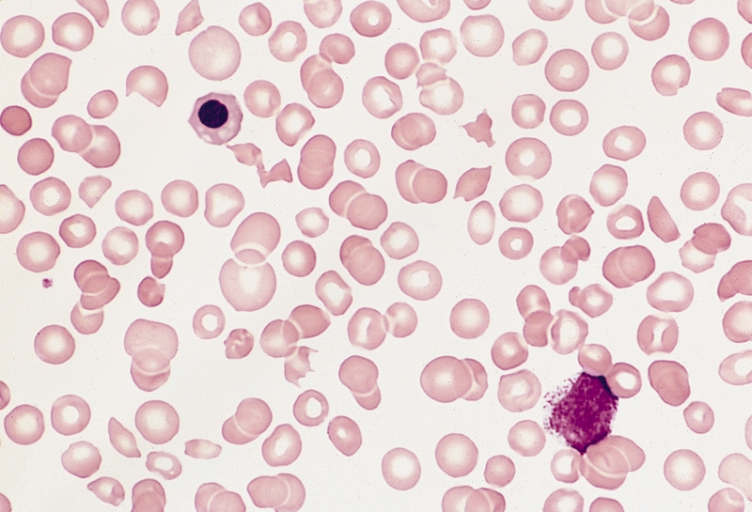
| Image = | | | Image = Thrombocytopenia 001.jpg| |
| Caption = | | | Caption = Marked thrombocytopenia and fragmented red blood cells.<br> <small> [http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] </small>| |
| DiseasesDB = 27522 |
| |
| ICD10 = {{ICD10|D|69|6|d|65}}, {{ICD10|P|61|0|p|50}} |
| |
| ICD9 = {{ICD9|287.3}}, {{ICD9|287.4}}, {{ICD9|287.5}} |
| |
| ICDO = |
| |
| OMIM = 188000 |
| |
| OMIM_mult = {{OMIM2|313900}} |
| |
| MedlinePlus = 000586 |
| |
| eMedicineSubj = |
| |
| eMedicineTopic = |
| |
| MeshID = D013921 |
| |
| }} | | }} |
|
| |
|
| {{SI}} | | {{Thrombocytopenia}} |
| {{CMG}} | | {{CMG}}, {{AE}} {{FZ}} |
|
| |
|
| {{Editor Join}} | | {{SK}} Congenital amegakaryocytic thrombocytopenia, CAMT |
|
| |
|
| '''Thrombocytopenia''' (or '''-paenia''', or '''thrombopenia''' in short) is the presence of relatively few [[platelets]] in [[blood]].
| | ==[[Thrombocytopenia overview|Overview]]== |
|
| |
|
| Generally speaking a normal platelet count ranges from 150,000 and 450,000 per mm<sup>3</sup>. These limits, however, are determined by the 2.5th lower and upper [[percentile]], and a deviation does not necessarily imply any form of disease. The number of platelets in a blood sample also decreases rather quickly with time and a low platelet count may be caused by a delay between sampling and analysis.
| | ==[[Thrombocytopenia historical perspective|Historical Perspective]]== |
|
| |
|
| ==Signs and symptoms== | | ==[[Thrombocytopenia classification|Classification]]== |
| Often, low platelet levels do not lead to clinical problems; rather, they are picked up on a routine [[full blood count]] (or CBC, [[complete blood count]] ). Occasionally, there may be [[bruising]], particularly [[purpura]] in the forearms, [[nosebleed]]s and/or bleeding [[gums]].
| |
|
| |
|
| It is vital that a full medical history is elicited, to ensure the low platelet count is not due to a secondary process. It is also important to ensure that the other blood cell types [[red blood cells]], and [[white blood cells]], are not also suppressed.
| | ==[[Thrombocytopenia pathophysiology|Pathophysiology]]== |
|
| |
|
| ==Diagnosis== | | ==[[Thrombocytopenia causes|Causes]]== |
| Laboratory tests might include: [[full blood count]], [[liver enzyme]]s, [[renal function]], [[vitamin B12]] levels, [[folic acid]] levels, [[erythrocyte sedimentation rate]], and peripheral blood smear.
| |
|
| |
|
| If the cause for the low platelet count remains unclear, [[bone marrow biopsy]] is often undertaken, to differentiate whether the low platelet count is due to ''decreased production'' or ''peripheral destruction''.
| | ==[[Thrombocytopenia differential diagnosis|Differentiating Thrombocytopenia from other Diseases]]== |
|
| |
|
| ==Causes== | | ==[[Thrombocytopenia risk factors|Risk Factors]]== |
| There are two broad mechanisms of thrombocytopenia: reduced platelet production and increased platelet destruction. Thormbocytopenia is seen in a variety of infectious and genetic disorders as well as a side effect of a large list of phramacotherapies.
| |
|
| |
|
| ----
| | ==[[Thrombocytopenia screening|Screening]]== |
| ===Decreased production=== | |
|
| |
|
| ====Vitamin deficiencies==== | | ==[[Thrombocytopenia natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| *[[vitamin B12]] or [[folic acid]] deficiency
| |
|
| |
|
| ====Hematologic disorders==== | | ==Diagnosis== |
| *[[leukemia]] or [[myelodysplastic syndrome]]
| | [[Thrombocytopenia diagnostic study of choice|Diagnostic Study of Choice]] | [[Thrombocytopenia history and symptoms|History and Symptoms]] | [[Thrombocytopenia physical examination|Physical Examination]] | [[Thrombocytopenia laboratory findings|Laboratory Findings]] | [[Thrombocytopenia electrocardiogram|Electrocardiogram]] | [[Thrombocytopenia x-ray|X-ray]] | [[Thrombocytopenia echocardiography and ultrasound|Echocardiography and Ultrasound]] | [[Thrombocytopenia ct|CT]] | [[Thrombocytopenia mri|MRI]] | [[Thrombocytopenia other imaging findings|Other Imaging Findings]] | [[Thrombocytopenia other diagnostic studies|Other Diagnostic Studies]] |
| | |
| ====Reduced thrombopoiesis due to reduced thrombopoietin production====
| |
| *Decreased production of [[thrombopoietin]] by the [[liver]] in [[liver failure]].
| |
| | |
| ====Infectious etiologies====
| |
| *[[Sepsis]], systemic [[viral]] or [[bacterial infection]]
| |
| *[[Dengue fever]] can cause thrombocytopenia by direct infection of [[bone marrow]] [[megakaryocytes]] as well as immunological shortened [[platelet]] survival
| |
| *Protozoa and protozoal conditions
| |
| *Visceral [[leishmaniasis]]
| |
| *Human granulocytic [[ehrlichiosis]]
| |
| *Human monocytotropic [[ehrlichiosis]]
| |
| *[[Mycoplasma pneumonia]]
| |
| *Staphylococcal [[toxic shock syndrome]]
| |
| *[[Epstein-Barr virus]]
| |
| *[[Hantavirus]]
| |
| *[[HIV-1]] disease
| |
| *[[Infectious mononucleosis]]
| |
| *[[Lassa fever]]
| |
| *[[Measles]]
| |
| *[[Mumps]]
| |
| *Oklahoma tick fever
| |
| *[[Rubella]]
| |
| *Severe [[acute respiratory distress syndrome]]
| |
| *Tick born encephalitis
| |
| | |
| ====Intrauterine acquired conditions====
| |
| *Neonatal alloimmune thrombocytopenia
| |
| *[[Rubella]], congenital
| |
| *[[Syphilis]], congenital
| |
| | |
| ====Hereditary syndromes====
| |
| *Congenital Amegakaryocytic Thrombocytopenia (CAMT)
| |
| *[[Bernard-Soulier syndrome]], associated with large platelets
| |
| *[[May-Hegglin]] anomaly, the combination of thrombocytopenia, pale-blue leuckocyte inclusions, and giant platelets
| |
| *[[Grey platelet syndrome]]
| |
| *[[Alport syndrome]]
| |
| | |
| =====Chromosomal abnormalities=====
| |
| *[[Jacobsen syndrome]]
| |
| | |
| =====Mendelian inherited conditions=====
| |
| *Autoimmune lymphoproliferative syndrome type 1
| |
| *Autoimmune lymphoproliferative syndrome type 2
| |
| *Radial aplasia-thrombocytopenia syndrome or [[Thrombocytopenia absent radius]] syndrome
| |
| *[[von Willebrand disease]], platelet type
| |
| | |
| =====Autosomal dominant conditions=====
| |
| *Arias oculootoradial syndrome
| |
| *Complement [[factor H|factor H deficiency]]
| |
| *[[Fechtner syndrome]]
| |
| *[[May-Hegglin anomaly]]
| |
| *Platelet glycoprotein 4 deficiency
| |
| *[[Sebastian platelet syndrome]]
| |
| | |
| =====Autosomal recessive conditions=====
| |
| *[[Chediak-Higashi disease]]
| |
| *Dibasic [[aminoaciduria]] type 2
| |
| *Familial [[histiocytic reticulosis]]
| |
| *[[Fanconi anaemia]]
| |
| *[[Folate]] malabsorption hereditary
| |
| *[[Gaucher disease]]
| |
| *[[Griscelli syndrome]] type 1
| |
| *[[Holocarboxylase synthase deficiency]]
| |
| *[[Iminodipeptiduria]]
| |
| *[[Isovaleric acidaemia]]
| |
| *[[Methylmalonic aciduria]] type 2
| |
| *Neuroectodermal melanolysosomal disease
| |
| *[[Niemann-Pick disease]] type B
| |
| *[[Omenn syndrome]]
| |
| *[[Platelet glycoprotein Ib deficiency]]
| |
| *[[Propionyl-CoA carboxylase deficiency]] PCCA type
| |
| *[[Sea blue histiocytosis]]
| |
| *[[Shwachman-Diamond syndrome]]
| |
| | |
| =====X-linked inherited conditions=====
| |
| *GATA1-related cytopenia
| |
| *Immunodysregulation polyendocrinopathy and enteropathy, X-linked
| |
| *[[Wiskott-Aldrich syndrome]]
| |
| *X-linked hyperimmunoglobulin M syndrome
| |
| *Mitochondrial genome inherited conditions
| |
| *[[MELAS]]
| |
| | |
| ----
| |
| | |
| ===Increased destruction===
| |
| ====Hematologic Disorders====
| |
| *[[Idiopathic thrombocytopenic purpura]] (ITP)
| |
| *[[Thrombotic thrombocytopenic purpura]] (TTP)
| |
| *[[Hemolytic-uremic syndrome]] (HUS)
| |
| *[[Disseminated intravascular coagulation]] (DIC)
| |
| *[[Paroxysmal nocturnal hemoglobinuria]] (PNH)
| |
| *[[Neonatal alloimmune thrombocytopenia]] (NAITP)
| |
| | |
| ====Autoimmunde Disorders====
| |
| *[[Antiphospholipid syndrome]]
| |
| *[[Systemic lupus erythematosus]] (SLE)
| |
| *post [[transfusion]] [[purpura]]
| |
| | |
| ====Infectious Disorders====
| |
| *[[Dengue fever]] has been shown to cause shortened platelet survival and immunological platelet destruction
| |
| *HIV [http://linkinghub.elsevier.com/retrieve/pii/S0268960X01901882]
| |
| | |
| ====Other disorders====
| |
| *Splenic sequestration of platelets due to [[hypersplenism]]
| |
| | |
| ===Medication-induced===
| |
| | |
| ====Mechanisms====
| |
| =====Direct myelosuppression=====
| |
| *[[Valproic acid]]
| |
| *[[Methotrexate]]
| |
| *[[Carboplatin]]
| |
| *[[Interferon]]
| |
| *Other [[chemotherapy]] drugs
| |
| | |
| =====Immunological platelet destruction=====
| |
| *Drug binds [[Fragment antigen binding|Fab]] portion of an [[antibody]]. The classic example of this mechanism is the [[quinidine]] group of drugs. The Fc portion of the antibody molecule is not involved in the binding process.
| |
| *Drug binds to Fc, and drug-antibody complex binds and activates platelets. [[Heparin induced thrombocytopenia]] (HIT) is the classic example of this phenomenon. In HIT, the heparin-antibody-platelet factor 4 (PF4) complex binds to Fc receptors on the surface of the platelet. Since Fc portion of the antibody is bound to the platelets, they are not available to the Fc receptors of the reticulo-endothelial cells, so therefore this system cannot destroy platelets as usual. This may explain why severe thrombocytopenia is not a common feature of HIT.
| |
| | |
| =====[[Heparin-induced thrombocytopenia]]=====
| |
| (HIT or ''white clot syndrome''): this is a rare but serious condition that may occur in a hospitalized population. The most common clinical setting for HIT is in postoperative coronary artery bypass graft recipients, who may receive large quantities of heparin during surgery. HIT typically occurs about a week after exposure to heparin. The heparin-PF4 antibody complex will activate the platelets, and this can often lead to [[thrombosis]]. The term HITT, where the last T stands for thrombosis, denotes the concept that heparin-induced thrombocytopenia often is associated with [[thrombosis]].
| |
| | |
| | |
| =====List of potential etiologies:=====
| |
| {{col-begin}}
| |
| {{col-break}}
| |
| | |
| [[Low molecular weight heparin]]s
| |
| | |
| Sulphonamides
| |
| | |
| Drugs, hormones and mediators
| |
| | |
| [[5-Azacytidine]]
| |
| | |
| [[Abciximab]]
| |
| | |
| Aclarubicin
| |
| | |
| [[Actinomycin D]]
| |
| | |
| [[Aggrastat]]
| |
| | |
| [[Albendazole]]
| |
| | |
| [[Alemtuzumab]]
| |
| | |
| [[Altretamine]]
| |
| | |
| [[Amiodarone]]
| |
| | |
| [[Amrinone]]
| |
| | |
| [[Anagrelide]]
| |
| | |
| Anazolene
| |
| | |
| Antithymocyte globulin
| |
| | |
| [[Ardeparin]]
| |
| | |
| [[Arsenic]] trioxide
| |
| | |
| [[Azathioprine]]
| |
| | |
| [[Bendamustine]]
| |
| | |
| [[Benoxaprofen]]
| |
| | |
| [[Bortezomib]]
| |
| | |
| [[Captopril]]
| |
| | |
| [[Caspofungin]]
| |
| | |
| [[Chloramphenicol]]
| |
| | |
| [[Cilazapril]]
| |
| | |
| [[Cimetidine]]
| |
| | |
| [[Cladribine]]
| |
| | |
| [[Clofarabine]]
| |
| | |
| [[Dasatinib]]
| |
| | |
| [[Decitabine]]
| |
| | |
| [[Desferrioxamine]]
| |
| | |
| [[Doxorubicin]]
| |
| | |
| [[Efalizumab]]
| |
| | |
| {{col-break}}
| |
| | |
| [[Eflornithine]]
| |
| | |
| [[Epirubicin]]
| |
| | |
| [[Eptifibatide]]
| |
| | |
| [[Ethanol]]
| |
| | |
| [[Flucytosine]]
| |
| | |
| [[Fondaparinux]]
| |
| | |
| [[Ganciclovir]]
| |
| | |
| [[Gemcitabine]]
| |
| | |
| [[Gemtuzumab ozogamicin]]
| |
| | |
| [[Gold salts]]
| |
| | |
| Guanidinium
| |
| | |
| Haem arginate
| |
| | |
| [[Heparin]]
| |
| | |
| [[Ibritumomab tiuxetan]]
| |
| | |
| [[Idarubicin]]
| |
| | |
| [[Imatinib mesylate]]
| |
| | |
| [[Indomethacin]]
| |
| | |
| [[Integrilin]]
| |
| | |
| [[Interferon alpha]]
| |
| | |
| [[Interleukin 10]]
| |
| | |
| [[Interleukin 2]]
| |
| | |
| [[Irinotecan]]
| |
| | |
| [[Ixabepilone]]
| |
| | |
| [[Lenalidomide]]
| |
| | |
| [[Lomustine]]
| |
| | |
| [[Melphalan]]
| |
| | |
| [[Mercaptopurine]]
| |
| | |
| [[Methyldopa]]
| |
| | |
| Methyldopate
| |
| | |
| [[Mithramycin]]
| |
| | |
| [[Nelarabine]]
| |
| | |
| [[Nilotinib]]
| |
| | |
| {{col-break}}
| |
| [[Nitisinone]]
| |
| | |
| [[Oxaliplatin]]
| |
| | |
| Para-amino [[salicylic acid]]
| |
| | |
| [[Pemetrexed]]
| |
| | |
| [[Penicillamine]]
| |
| | |
| [[Pentamidine]]
| |
| | |
| [[Phenylbutazone]]
| |
| | |
| [[Pyrimethamine]]
| |
| | |
| [[Quinidine]]
| |
| | |
| [[Quinine]]
| |
| | |
| [[Ranitidine]]
| |
| | |
| [[ReoPro]]
| |
| | |
| [[Rifampicin]]
| |
| | |
| [[Sirolimus]]
| |
| | |
| [[Sorafenib]]
| |
| | |
| [[Stiripentol]]
| |
| | |
| Sulphasalazine
| |
| | |
| Sunitinib malate
| |
| | |
| [[Temozolomide]]
| |
| | |
| [[Ticlopidine]]
| |
| | |
| [[Tirofiban]]
| |
| | |
| [[Topotecan]]
| |
| | |
| [[Trabectedin]]
| |
| | |
| [[Trimetrexate]]
| |
| | |
| [[Valganciclovir]]
| |
| | |
| [[Valproic acid]]
| |
| | |
| [[Vancomycin]]
| |
| | |
| [[Vinorelbine]]
| |
| | |
| [[Vorinostat]]
| |
| | |
| |}
| |
| | |
| ==Complete Differential Diagnosis of Thrombocytopenia==
| |
| Haematological abnormalities
| |
| Pancytopenia
| |
| (Specific kind of Thrombocytopenia) Shortcut to causes of Pancytopenia
| |
| Epiphenomena
| |
| Kasabach-Merritt syndrome
| |
| Paraneoplastic syndrome
| |
| Miscellaneous syndromes
| |
| Aplastic anemia
| |
| Hypersplenism
| |
| Myelodysplastic syndrome
| |
| Myelofibrosis
| |
| Thrombotic thrombocytopenic purpura
| |
| Splenomegaly
| |
| Haematological abnormalities
| |
| Disseminated intravascular coagulation
| |
| Posttransfusion alloimmune thrombocytopenia
| |
| | |
| Nutritional conditions
| |
| Iron deficiency
| |
| Cardiac and vascular conditions
| |
| Cholesterol embolism
| |
| Autoimmune conditions
| |
| Anticardiolipin syndrome
| |
| Evans syndrome
| |
| Idiopathic thrombocytopenic purpura
| |
| Systemic lupus erythematosus
| |
| Inflammatory conditions
| |
| Macrophage activation syndrome
| |
| Neoplastic conditions
| |
| Histiocytosis X
| |
| Malignant neoplastic conditions
| |
| Acute lymphoblastic leukemia
| |
| Acute myeloid leukemia
| |
| Chronic lymphocytic leukaemia
| |
| Chronic myeloid leukaemia
| |
| Hairy cell leukaemia
| |
| Myeloma
| |
| Non-Hodgkin lymphoma
| |
| Obstetric conditions
| |
| Eclampsia
| |
| HELLP syndrome
| |
| Pre-eclampsia
| |
| | |
| Iatrogenic conditions
| |
| Blood transfusion and complications
| |
| Chemicals
| |
| Strontium-89
| |
| Zinc
| |
| Drug groups
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| Treatment is guided by etiology and disease severity. The main concept in treating thrombocytopenia is to eliminate the underlying problem, whether that means discontinuing suspected drugs that cause thrombocytopenia, or treating underlying sepsis. Diagnosis and treatment of serious thrombocytopenia is usually directed by a [[hematologist]].
| | [[Thrombocytopenia medical therapy|Medical Therapy]] | [[Thrombocytopenia surgery|Surgery]] | [[Thrombocytopenia primary prevention|Primary Prevention]] | [[Thrombocytopenia secondary prevention|Secondary Prevention]] | [[Thrombocytopenia cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Thrombocytopenia future or investigational therapies|Future or Investigational Therapies]] |
| | |
| Specific treatment plans often depend on the underlying [[etiology]] of the thrombocytopenia.
| |
| | |
| ===Thrombotic thrombocytopenic purpura (TTP)===
| |
| Treatment of [[thrombotic thrombocytopenic purpura]] is a medical emergency, since the [[hemolytic anemia]] and platelet activation can lead to [[renal failure]] and changes in the level of consciousness. Treatment of [[thrombotic thrombocytopenic purpura|TTP]] was revolutionized in the 1980s with the application of [[plasmapheresis]]. According to the Furlan-Tsai hypothesis
| |
| <ref>{{cite journal |author=Furlan M, Lämmle B |title=Aetiology and pathogenesis of thrombotic thrombocytopenic purpura and haemolytic uraemic syndrome: the role of von Willebrand factor-cleaving protease |journal=Best Pract Res Clin Haematol |volume=14 |issue=2 |pages=437-54 |year=2001 |pmid=11686108}}</ref>
| |
| <ref>{{cite journal |author=Tsai H |title=Advances in the pathogenesis, diagnosis, and treatment of thrombotic thrombocytopenic purpura |journal=J Am Soc Nephrol |volume=14 |issue=4 |pages=1072-81 |year=2003 |pmid=12660343}}</ref>
| |
| , this treatment theoretically works by removing [[antibodies]] directed against the [[von Willebrand factor]] cleaving [[protease]], [[ADAMTS13|ADAMTS-13]]. The [[plasmapheresis]] procedure also adds active [[ADAMTS13|ADAMTS-13]] [[protease]] [[proteins]] to the patient, restoring a more physiological state of [[von Willebrand factor]] multimers. Patients with persistent antibodies against [[ADAMTS-13]] do not always manifest [[thrombotic thrombocytopenic purpura|TTP]], and these antibodies alone are not sufficient to explain the how [[plasmapheresis]] treats [[thrombotic thrombocytopenic purpura|TTP]].
| |
| | |
| ===ITP===
| |
| In many cases, ITP is self-limited, and does not require treatment. Platelet counts less than ten thousand per mm3 usually require treatment(less than fifty thousand requires treatment, less than ten thousand is a potentially dangerous situation) and patients with significant bleeding and thrombocytopenia due to ITP are also usually treated. The threshold for treating ITP has decreased since the 1990s, and hematologists recognize that patients rarely bleed with platelet counts greater than ten thousand, though there are documented exceptions to this observation. Treatments for ITP include:
| |
| *[[Prednisone]] and other [[corticosteroids]]
| |
| *[[Intravenous gamma globulin]]
| |
| *[[Splenectomy]]
| |
| *[[Danazol]]
| |
| *[[Rituximab]]
| |
| | |
| Thrombopoetin analogues have been tested extensively for the treatment of ITP. These agents had previously shown promise but had been found to stimulate antibodies against endogenous [[thrombopoeitin]] or lead to [[thrombosis]].
| |
| | |
| A medication known as AMG 531 was found to be safe and effective for the treatment of ITP in refractory patients.
| |
| <ref>{{cite journal |author=Bussel J, Kuter D, George J, McMillan R, Aledort L, Conklin G, Lichtin A, Lyons R, Nieva J, Wasser J, Wiznitzer I, Kelly R, Chen C, Nichol J |title=AMG 531, a thrombopoiesis-stimulating protein, for chronic ITP |journal=N Engl J Med |volume=355 |issue=16 |pages=1672-81 |year=2006 |pmid=17050891}}</ref>
| |
| AMG 531 is a [[peptide]] that bears no [[sequence homology]] with endogenous [[human]] [[thrombopoeitin]], so it is not as likely to lead to neutralizing antibodies as previous peptide [[thrombopoeitin]] analogues.
| |
| <ref>{{cite journal |author=Broudy V, Lin N |title=AMG531 stimulates megakaryopoiesis in vitro by binding to Mpl |journal=Cytokine |volume=25 |issue=2 |pages=52-60 |year=2004 |pmid=14693160}}</ref>
| |
| | |
| ===Heparin-induced thrombocytopenia and thrombosis (HITT)===
| |
| Discontinuation of heparin is critical in a case of HITT. Beyond that, however, care must be taken to avoid a thrombosis, and patients started directly on [[warfarin]] after a diagnosis of HITT are at excess risk of venous limb gangrene. For this reason, patients are usually treated with a type of [[blood thinner]] called a [[direct thrombin inhibitor]] such as the [[FDA]]-approved [[lepirudin]] or [[argatroban]]. Other [[blood thinners]] sometimes used in this setting that are not [[FDA]]-approved for treatment of HITT include [[bivalirudin]] and [[fondaparinux]]. [[Platelet transfusions]] are not a routine component of the treatment of [[HITT]], since thrombosis, not bleeding, is the usual associated problem in this illness.
| |
| | |
| ===Congenital amegakaryocytic thrombocytopenia (CAMT)===
| |
| Bone Marrow/Stem Cell Transplant is the only thing that ultimately cures this genetic disease. Frequent platelet transfusions are required to keep the patient from bleeding to death until transplant is done.
| |
| | |
| ==References==
| |
| {{reflist|2}}
| |
| | |
| ==External links==
| |
| * {{MerckManual|11|133|b}}
| |
| | |
| * [http://www.lowplatelets.com/?rotation=27016898&banner=199576400&placement={placement} Low platelets.com] a resource for patients with thrombocytopenia.
| |
|
| |
|
| {{Hematology}}
| | ==Case Studies== |
| {{SIB}}
| | [[Thrombocytopenia case study one|Case #1]] |
|
| |
|
| [[Category:Blood disorders]] | | [[Category:Blood disorders]] |
| [[Category:Hematology]] | | [[Category:Hematology]] |
|
| |
| [[de:Thrombozytopenie]]
| |
| [[es:Trombocitopenia]]
| |
| [[fr:Thrombocytopénie]]
| |
| [[hr:Trombocitopenija]]
| |
| [[id:Trombositopenia]]
| |
| [[it:Piastrinopenia]]
| |
| [[mk:Тромбоцитопенија]]
| |
| [[nl:Trombocytopenie]]
| |
| [[pl:Małopłytkowość]]
| |
| [[pt:Trombocitopenia]]
| |
| [[ru:Тромбоцитопения]]
| |
| [[sv:Trombocytopeni]]
| |
| [[tr:Trombositopeni]]
| |
|
| |
|
| {{WikiDoc Help Menu}} | | {{WikiDoc Help Menu}} |
| {{WikiDoc Sources}} | | {{WikiDoc Sources}} |