Thoracentesis
Template:Interventions infobox
|
WikiDoc Resources for Thoracentesis |
|
Articles |
|---|
|
Most recent articles on Thoracentesis Most cited articles on Thoracentesis |
|
Media |
|
Powerpoint slides on Thoracentesis |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Thoracentesis at Clinical Trials.gov Trial results on Thoracentesis Clinical Trials on Thoracentesis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Thoracentesis NICE Guidance on Thoracentesis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Thoracentesis Discussion groups on Thoracentesis Patient Handouts on Thoracentesis Directions to Hospitals Treating Thoracentesis Risk calculators and risk factors for Thoracentesis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Thoracentesis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For the WikiPatient page for this topic, click here
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
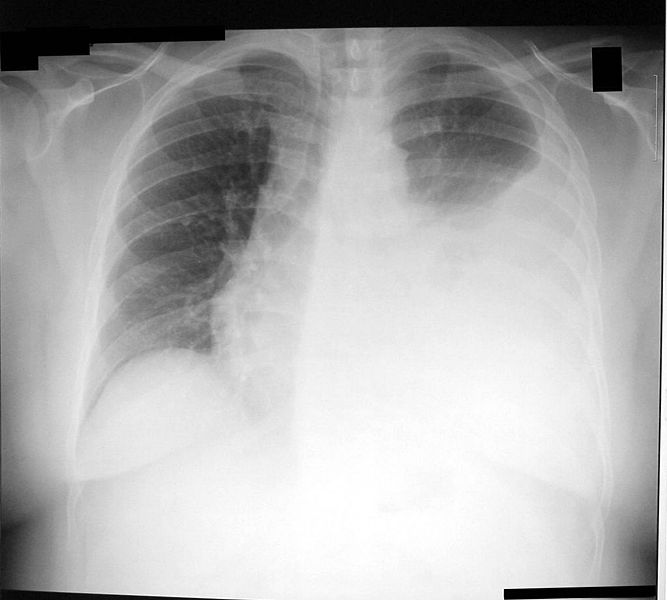
Thoracentesis (also known as thoracocentesis or pleural tap) is an invasive procedure to remove fluid or air from the pleural space for diagnostic or therapeutic purposes. A cannula, or hollow needle, is carefully introduced into the thorax, generally after administration of local anesthesia. The procedure was first described in 1852.
Indications
This procedure is indicated when unexplained fluid accumulates in the chest cavity outside the lung. In more than 90% of cases analysis of pleural fluid yields clinically useful information. If a large amount of fluid is present, then this procedure can also be used therapeutically to remove that fluid and improve patient comfort and lung function.
The most common causes of pleural effusions are cancer, congestive heart failure, pneumonia, and recent surgery. In countries where tuberculosis is common, this is also a common cause of pleural effusions.
When cardiopulmonary status is compromised (i.e. when the fluid or air has its repercussions on the function of heart and lungs), due to air (significant pneumothorax), fluid (pleural fluid) or blood (hemothorax) outside the lung, then this procedure is usually replaced with tube thoracostomy, the placement of a large tube in the pleural space.
Contraindications
An uncooperative patient or a coagulation disorder that can not be corrected are absolute contraindications.
Relative contraindications are site of insertion has known bullous disease (e.g. emphysema), use of positive end-expiratory pressure (PEEP, see mechanical ventilation) and only one functioning lung (due to diminished reserve).
Complications
Major complications are pneumothorax (3-30%), hemopneumothorax, hemorrhage, hypotension (low blood pressure due to a vasovagal response) and reexpansion pulmonary edema.
Minor complications include a dry tap (no fluid return), subcutaneous hematoma or seroma, anxiety, dyspnea and cough (after removing large volume of fluid).
Interpretation of pleural fluid analysis
Several diagnostic tools are available to determine the etiology of pleural fluid.
Transudate versus exudate
First the fluid is either transudate or exudate.
A transudate is defined as pleural fluid to serum total protein ratio of less than 0.5, pleural fluid to serum LDH ratio < 0.6, and absolute pleural fluid LDH < 200 IU or < 2/3 of the normal serum level.
An exudate is any pleural fluid that does not meet aforementioned criteria.
Exudate
- hemorrhage
- Infection
- Inflammation
- Malignancy
- Iatrogenic
- Connective tissue disease
- Endocrine disorders
- Lymphatic disorders vs Constrictive pericarditis
Transudate
- Congestive heart failure
- Nephrotic syndrome
- Hypoalbuminemia
- Cirrhosis
- Atelectasis
- trapped lung
- Peritoneal dialysis
- Superior vena cava obstruction
Amylase
A high amylase level (twice the serum level or the absolute value is greater than 160 Somogy units) in the pleural fluid is indicative of either acute or chronic pancreatitis, pancreatic pseudocyst that has dissected or ruptured into the pleural space, cancer or esophageal rupture.
Glucose
This is considered low if pleural fluid value is less than 50% of normal serum value. The differential diagnosis for this is:
- rheumatoid effusion
- lupus effusion
- bacterial empyema
- malignancy
- tuberculosis
- esophageal rupture (Boerhaave syndrome)
pH
Normal pleural fluid pH is approximately 7.60. A pleural fluid pH below 7.30 with normal arterial blood pH has the same differential diagnosis as low pleural fluid glucose.
Triglyceride and cholesterol
Chylothorax (fluid from lymph vessels leaking into the pleural cavity) may be identified by determining triglyceride and cholesterol levels, which are relatively high in lymph. A triglyceride level over 110 mg/dl and the presence of chylomicrons indicate a chylous effusion. The appearance is generally milky but can be serous.
The main cause for chylothorax is rupture of the thoracic duct, most frequently as a result of trauma or malignancy (such as lymphoma).
Cell count and differential
The number of white blood cells can give an indication of infection. The specific subtypes can also give clues as to the type on infection. The amount of red blood cells are an obvious sign of bleeding.
Cultures and stains
If the effusion is caused by infection, microbiological culture may yield the infectious organism responsible for the infection, sometimes before other cultures (e.g. blood cultures and sputum cultures) become positive. A Gram stain may give a rough indication of the causative organism. A Ziehl-Neelsen stain may identify tuberculosis or other mycobacterial diseases.
Cytology
Cytology is an important tool in identifying effusions due to malignancy. The most common causes for pleural fluid are lung cancer, metastasis from elsewhere and mesothelioma. The latter often presents with an effusion. Normal cytology results do not reliably rule out malignancy, but make the diagnosis more unlikely.
References
- Intensive Care Medicine by Irwin and Rippe
- The ICU Book by Marino
- Procedures and Techniques in Intensive Care Medicine by Irwin and Rippe
- Pulmonary - Critical Care Associates of East Texas
- Thoracentesis from THE MERCK MANUAL, Sec. 6, Ch. 65, Special Procedures
External links
- A photo gallery of thoracentesis showing the procedure step-by-step. V. Dimov, B. Altaqi, Clinical Notes, 2005. A free PDA version.
- Diagnostic Thoracentesis Virtual Cancer Centre
- Therapeutic Thoracentesis Virtual Cancer Centre
Template:Respiratory system surgeries and other procedures Template:SIB