Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery: Difference between revisions
Gerald Chi (talk | contribs) |
Gerald Chi (talk | contribs) m (→SYNTAX Score) |
||
| Line 12: | Line 12: | ||
==SYNTAX Score== | ==SYNTAX Score== | ||
<!--Under Construction--> | |||
Diagnostic angiograms were assessed by staff at an independent core laboratory who were unaware of treatment status of patients. A SYNTAX Score was designed for scoring of the coronary angiograms according to the complexity and severity of the coronary artery disease.<ref name="urlSYNTAX Score">{{cite web |url=http://www.syntaxscore.com/ |title=SYNTAX Score |format= |work= |accessdate=}}</ref> The SYNTAX score was used as a diagnostic tool for comprehensive anatomical assessment of patients with coronary artery disease .Higher scores reflect more complex disease and lower scores less severe.Patients with left main disease with 1 or 2 vessel disease had higher scores as compared to 3-vessel disease.A high score was considered > 33 and a low score was defined as < 22.<ref name="pmid19228612">{{cite journal |author=Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW |title=Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease |journal=[[N. Engl. J. Med.]] |volume=360 |issue=10 |pages=961–72 |year=2009 |month=March |pmid=19228612 |doi=10.1056/NEJMoa0804626 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=19228612&promo=ONFLNS19}}</ref> | Diagnostic angiograms were assessed by staff at an independent core laboratory who were unaware of treatment status of patients. A SYNTAX Score was designed for scoring of the coronary angiograms according to the complexity and severity of the coronary artery disease.<ref name="urlSYNTAX Score">{{cite web |url=http://www.syntaxscore.com/ |title=SYNTAX Score |format= |work= |accessdate=}}</ref> The SYNTAX score was used as a diagnostic tool for comprehensive anatomical assessment of patients with coronary artery disease .Higher scores reflect more complex disease and lower scores less severe.Patients with left main disease with 1 or 2 vessel disease had higher scores as compared to 3-vessel disease.A high score was considered > 33 and a low score was defined as < 22.<ref name="pmid19228612">{{cite journal |author=Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW |title=Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease |journal=[[N. Engl. J. Med.]] |volume=360 |issue=10 |pages=961–72 |year=2009 |month=March |pmid=19228612 |doi=10.1056/NEJMoa0804626 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=19228612&promo=ONFLNS19}}</ref> | ||
=== | ====Definition of the Coronary Tree Segments==== | ||
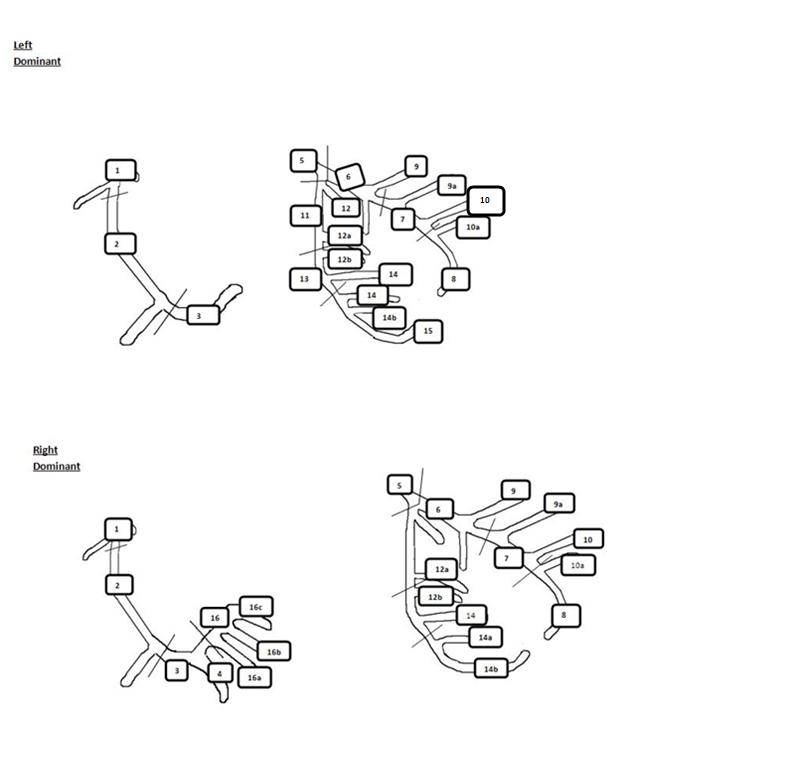
[[Image:SYNTAX_Coronary_Arterial_Segments_Definitions.JPG |center|800px|SYNTAX Coronary Arterial Tree Segments]] | |||
[[Image:SYNTAX_Coronary_Arterial_Segments_Definitions.JPG |center| | '''1.''' RCA Proximal: From the ostium to one half the distance to the acute margin of the heart.<br> | ||
'''2.''' RCA Mid: From the end of the first segment to acute margin of the heart.<br> | |||
'''3.''' RCA Distal: From the acute margin of the heart to the origin of the posterior descending artery<br> | |||
'''4.''' Posterior descending artery: Running in the posterior interventricular groove.<br> | |||
'''16.''' Posterolateral branch from the RCA: Posterolateral branch originating from the distal coronary artery distal to the crux.<br> | |||
'''16a.''' Posterolateral branch from the RCA: First posterolateral branch from segment 16.<br> | |||
'''16b.''' Posterolateral branch from the RCA: Second posterolateral branch from the segment 16.<br> | |||
'''16c.''' Posterolateral branch from the RCA: Third posterolateral branch from the segment 16. <br> | |||
'''5.''' Left main: From the ostium of the LCA through bifurcation into the left anterior descending and left circumflex branches.<br> | |||
'''6.''' LAD Proximal: Proximal to and including first major septal branch.<br> | |||
'''7.''' LAD Mid: LAD immediately distal to the origin of first septal branch and extending to the point where LAD forms an angle (RAO view). If this angle is not identifiable this segment ends at one half the distance from the first septal to the apex of the heart.<br> | |||
'''8.''' LAD Apical: Terminal portion of LAD, beginning at the end of previous sement and extending to or beyond the apex.<br> | |||
'''9.''' First Diagonal: The first diagonal originating from segment 6 or 7.<br> | |||
'''9a.''' First Diagonal a: Additional first diagonal originating from segment 6 or 7, before segment 8.<br> | |||
'''10.''' Second Diagonal: Orginating from segment 8 or the transition between segment 7 and 8.<br> | |||
'''10a.''' Second Diagonal a: Additional second diagonal originating from segment 8.<br> | |||
'''11.''' Proximal Circumflex: Main stem of circumflex from its origin of left main and including origin of first obtuse marginal branch.<br> | |||
'''12.''' Intermediate/anterolateral artery: Branch from trifurcating left main other than proximal LAD or LCX. It belongs to the circumflex territory.<br> | |||
'''12a.''' Obtuse marginal a: First side branch of circumflex running in general to the area of obtuse margin of the heart.<br> | |||
'''12b.''' Obtuse marginal b: Second additional branch of circumflex running in the same direction as 12.<br> | |||
'''13.''' Distal Circumflex artery: The stem of circumflex distal to the origin from the most distal obtuse marginal branch, and running along the posterior left atrioventricular groove. Caliber may be small or artery absent.<br> | |||
'''14.''' Left Posterolateral: Running to the posterolateral surface of the left ventricle. May be absent or a division of obtuse marginal branch.<br> | |||
'''14a.''' Left Posterolateral a: Distal from 14 and running in the same direction.<br> | |||
'''14b.''' Left Posterolateral b: Distal from 14 and 14a and running in the same direction.<br> | |||
'''15.''' Posterior descending: Most distal part of dominant left circumflex when present. It gives origin to the septal branches. When this artery is present, segment 4 is usually absent.<br> | |||
<table style="width:70%; height:180px" border="1" align="center" > | |||
<tr style="background:grey"> | <tr style="background:grey"> | ||
<td>'''Segment No'''</td> | <td>'''Segment No'''</td> | ||
| Line 24: | Line 50: | ||
<td>'''Left Dominance Score'''</td> | <td>'''Left Dominance Score'''</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>1</td> | <td>1</td> | ||
<td>RCA Proximal</td> | <td>RCA Proximal</td> | ||
| Line 30: | Line 56: | ||
<td>0</td> | <td>0</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>2</td> | <td>2</td> | ||
<td>RCA Mid</td> | <td>RCA Mid</td> | ||
| Line 36: | Line 62: | ||
<td>0</td> | <td>0</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>3</td> | <td>3</td> | ||
<td>RCA Distal</td> | <td>RCA Distal</td> | ||
| Line 42: | Line 68: | ||
<td>0</td> | <td>0</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>4</td> | <td>4</td> | ||
<td>Posterior Descending Artery</td> | <td>Posterior Descending Artery</td> | ||
| Line 48: | Line 74: | ||
<td>n.a.</td> | <td>n.a.</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>16</td> | <td>16</td> | ||
<td>Postero-lateral branch from RCA</td> | <td>Postero-lateral branch from RCA</td> | ||
| Line 54: | Line 80: | ||
<td>n.a.</td> | <td>n.a.</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>16a</td> | <td>16a</td> | ||
<td>Postero-lateral branch from RCA</td> | <td>Postero-lateral branch from RCA</td> | ||
| Line 60: | Line 86: | ||
<td>n.a.</td> | <td>n.a.</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>16b</td> | <td>16b</td> | ||
<td>Postero-lateral branch from RCA</td> | <td>Postero-lateral branch from RCA</td> | ||
| Line 66: | Line 92: | ||
<td>n.a.</td> | <td>n.a.</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>16c</td> | <td>16c</td> | ||
<td>Postero-lateral branch from RCA</td> | <td>Postero-lateral branch from RCA</td> | ||
| Line 72: | Line 98: | ||
<td>n.a.</td> | <td>n.a.</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>5</td> | <td>5</td> | ||
<td>Left Main</td> | <td>Left Main</td> | ||
| Line 78: | Line 104: | ||
<td>6</td> | <td>6</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>6</td> | <td>6</td> | ||
<td>LAD Proximal</td> | <td>LAD Proximal</td> | ||
| Line 84: | Line 110: | ||
<td>2.5</td> | <td>2.5</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>7</td> | <td>7</td> | ||
<td>LAD Mid</td> | <td>LAD Mid</td> | ||
| Line 90: | Line 116: | ||
<td>2.5</td> | <td>2.5</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>8</td> | <td>8</td> | ||
<td>LAD Apical</td> | <td>LAD Apical</td> | ||
| Line 96: | Line 122: | ||
<td>1</td> | <td>1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>9</td> | <td>9</td> | ||
<td>First Diagonal</td> | <td>First Diagonal</td> | ||
| Line 102: | Line 128: | ||
<td>1</td> | <td>1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>9a</td> | <td>9a</td> | ||
<td>First Diagonal a </td> | <td>First Diagonal a </td> | ||
| Line 108: | Line 134: | ||
<td>1</td> | <td>1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>10</td> | <td>10</td> | ||
<td>Second Diagonal </td> | <td>Second Diagonal </td> | ||
| Line 114: | Line 140: | ||
<td>0.5</td> | <td>0.5</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>10a</td> | <td>10a</td> | ||
<td>Second Diagonal a</td> | <td>Second Diagonal a</td> | ||
| Line 120: | Line 146: | ||
<td>0.5</td> | <td>0.5</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>11</td> | <td>11</td> | ||
<td>Proximal Circumflex Artery</td> | <td>Proximal Circumflex Artery</td> | ||
| Line 126: | Line 152: | ||
<td>2.5</td> | <td>2.5</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>12</td> | <td>12</td> | ||
<td>Intermediate/anterolateral artery</td> | <td>Intermediate/anterolateral artery</td> | ||
| Line 132: | Line 158: | ||
<td>1</td> | <td>1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>12a</td> | <td>12a</td> | ||
<td>Obtuse marginal a</td> | <td>Obtuse marginal a</td> | ||
| Line 138: | Line 164: | ||
<td>1</td> | <td>1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>12b</td> | <td>12b</td> | ||
<td>Obtuse marginal b</td> | <td>Obtuse marginal b</td> | ||
| Line 144: | Line 170: | ||
<td>1</td> | <td>1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>13</td> | <td>13</td> | ||
<td>Distal Cicumflex</td> | <td>Distal Cicumflex</td> | ||
| Line 150: | Line 176: | ||
<td>1.5</td> | <td>1.5</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>14</td> | <td>14</td> | ||
<td>Left Posterolateral </td> | <td>Left Posterolateral </td> | ||
| Line 156: | Line 182: | ||
<td>1</td> | <td>1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>14a</td> | <td>14a</td> | ||
<td>Left Posterolateral a</td> | <td>Left Posterolateral a</td> | ||
| Line 162: | Line 188: | ||
<td>1</td> | <td>1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>14b</td> | <td>14b</td> | ||
<td>Left Posterolateral b</td> | <td>Left Posterolateral b</td> | ||
| Line 168: | Line 194: | ||
<td>1</td> | <td>1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>15</td> | <td>15</td> | ||
<td>Posterior Descending Artery</td> | <td>Posterior Descending Artery</td> | ||
| Line 174: | Line 200: | ||
<td>1</td> | <td>1</td> | ||
</tr> | </tr> | ||
</table> | |||
====Scoring for Adverse Lesions Characteristics==== | ====Scoring for Adverse Lesions Characteristics==== | ||
Adverse lesions are more specifically scored according to their particular characteristic by either multiplying or adding by a certain factor. | Adverse lesions are more specifically scored according to their particular characteristic by either multiplying or adding by a certain factor. | ||
<table style="width:70%; align="right"> | |||
<table style="width: | |||
<td>'''Diameter Reduction'''</td> | <td>'''Diameter Reduction'''</td> | ||
<td>'''Scoring''' </td> | <td>'''Scoring''' </td> | ||
<tr> | <tr> | ||
<td>Total Occlusion </td> | <td>Total Occlusion </td> | ||
<td> x5 </td> | |||
</tr> | </tr> | ||
<tr> | |||
<td> Significant lesion | <td> Significant lesion </td> | ||
<td> x2 </td> | |||
</tr> | </tr> | ||
<tr> | |||
<td>''' Total Occlusion''' | <td>''' Total Occlusion''' </td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>Age> 3months or unknown</td> | <td>Age> 3months or unknown</td> | ||
<td>+1</td> | <td>+1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>Blunt stump</td> | <td>Blunt stump</td> | ||
<td>+1</td> | <td>+1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>Bridging </td> | <td>Bridging </td> | ||
<td>+1</td> | <td>+1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>First segment visble beyond TO </td> | <td>First segment visble beyond TO </td> | ||
<td>1/per non-visible segment </td> | <td>1/per non-visible segment </td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>Side branch (SB)For both < and ≥1.5</td> | <td>Side branch (SB)For both < and ≥1.5</td> | ||
<td> +1</td> | <td> +1</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>'''Aorto ostial stenosis '''</td> | |||
<td>'''Aorto ostial stenosis '''</td> | <td>+1 </td> | ||
<td>+1 </td> | |||
</tr> | </tr> | ||
<tr> | |||
<td>'''Severe Totuosity '''</td> | <td>'''Severe Totuosity '''</td> | ||
<td> | <td> +2 </td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>'''Lenght >20 mm '''</td> | <td>'''Lenght >20 mm '''</td> | ||
<td>+1 </td> | <td>+1 </td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>'''Heavy Classification '''</td> | <td>'''Heavy Classification '''</td> | ||
<td>+2</td> | <td>+2</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>'''Thrombus ''' | <td>'''Thrombus ''' | ||
<td> +1 </td> | <td> +1 </td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>'''Diffuse disease/small vessels ''' </td> | <td>'''Diffuse disease/small vessels ''' </td> | ||
<td>+1/ per segment number</td> | <td>+1/ per segment number</td> | ||
</tr> | </tr> | ||
<tr> | |||
</tr> | </tr> | ||
<tr> | |||
<br> | <br> | ||
<td>'''Trifurcations '''</td> | <td>'''Trifurcations '''</td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>1 diseased segment </td> | |||
<td>+3 </td> | |||
</tr> | |||
<tr> | |||
<td>2 diseased segments </td> | <td>2 diseased segments </td> | ||
<td> +4 </td> | <td> +4 </td> | ||
</tr> | </tr> | ||
<tr> | |||
<td> 3 diseased segments </td> | <td> 3 diseased segments </td> | ||
<td>+5 </td> | <td>+5 </td> | ||
</tr> | </tr> | ||
<tr> | |||
<td>4 diseased segments | <td>4 diseased segments </td> | ||
<td> +6 </td> | <td> +6 </td> | ||
</tr> | </tr> | ||
<tr> | |||
</tr> | </tr> | ||
<tr> | |||
<br> | <br> | ||
<td>'''Bifurcations '''</td> | |||
<td>'''Bifurcations '''</td> | |||
</tr> | </tr> | ||
<tr> | |||
<td>Type A,B,C </td> | |||
<td>Type A,B,C </td> | <td> +1 </td> | ||
<td> | |||
</tr> | </tr> | ||
<tr> | |||
<td>Type D,E,F </td> | <td>Type D,E,F </td> | ||
<td> +2 </td> | |||
</tr> | </tr> | ||
<tr> | |||
<td>Angulation <70° </td> | <td>Angulation <70° </td> | ||
<td> +1 </td> | |||
</tr> | </tr> | ||
</table> | |||
'''Type A''' lesions are defined as lesions not involving the ostium of side branch, in the main vessel proximal to the ostium of the side branch.<br> | '''Type A''' lesions are defined as lesions not involving the ostium of side branch, in the main vessel proximal to the ostium of the side branch.<br> | ||
'''Type B''' lesions are defined as lesions not involving the ostium of side branch, in the main vessel distal to the ostium of the side branch.<br> | '''Type B''' lesions are defined as lesions not involving the ostium of side branch, in the main vessel distal to the ostium of the side branch.<br> | ||
Revision as of 02:34, 17 October 2013
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: SYNTAX; SYNTAX score
Overview
SYNTAX which is the abbreviation for "Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery" was a prospective clinical trial conducted in 85 sites in 17 countries across Europe and the United States. The purpose of this study was to compare percutaneous stenting and cardiac surgery revascularization strategies for patients with previously untreated 3-vessel disease or left main coronary artery disease and to identify the populations for whom one strategy would be better than the other. Previous clinical trials comparing bare metal stents with coronary artery bypass graft (CABG) surgery had shown similar survival rates but higher revascularization rates in patients treated with bare metal stents. Randomized clinical trials have also shown drug eluting stents (DES) as compared with Bare Metal Stents (BMS), to show better results in terms of repeat revascularization. The SYNTAX trial was conducted to assess the efficacy of Taxus which is a Paclitaxel drug eluting stent as compared to CABG for effective means of revascularization in patients with three vessel disease or left main disease.
SYNTAX Trial Design
1,800 patients were enrolled in the SYNTAX trial. Both an interventional cardiologist and a cardiac surgeon assessed patients eligible for the study according to the study criteria.[1] Patients who were deemed to have similar outcomes by either CABG or PCI were randomly assigned to one revascularization either arm. Patients who were deemed to be more effectively treated with PCI were assigned to a parallel PCI registry for CABG ineligible patients and likewise to a CABG registry for PCI ineligible patients.
SYNTAX Score
Diagnostic angiograms were assessed by staff at an independent core laboratory who were unaware of treatment status of patients. A SYNTAX Score was designed for scoring of the coronary angiograms according to the complexity and severity of the coronary artery disease.[2] The SYNTAX score was used as a diagnostic tool for comprehensive anatomical assessment of patients with coronary artery disease .Higher scores reflect more complex disease and lower scores less severe.Patients with left main disease with 1 or 2 vessel disease had higher scores as compared to 3-vessel disease.A high score was considered > 33 and a low score was defined as < 22.[3]
Definition of the Coronary Tree Segments
1. RCA Proximal: From the ostium to one half the distance to the acute margin of the heart.
2. RCA Mid: From the end of the first segment to acute margin of the heart.
3. RCA Distal: From the acute margin of the heart to the origin of the posterior descending artery
4. Posterior descending artery: Running in the posterior interventricular groove.
16. Posterolateral branch from the RCA: Posterolateral branch originating from the distal coronary artery distal to the crux.
16a. Posterolateral branch from the RCA: First posterolateral branch from segment 16.
16b. Posterolateral branch from the RCA: Second posterolateral branch from the segment 16.
16c. Posterolateral branch from the RCA: Third posterolateral branch from the segment 16.
5. Left main: From the ostium of the LCA through bifurcation into the left anterior descending and left circumflex branches.
6. LAD Proximal: Proximal to and including first major septal branch.
7. LAD Mid: LAD immediately distal to the origin of first septal branch and extending to the point where LAD forms an angle (RAO view). If this angle is not identifiable this segment ends at one half the distance from the first septal to the apex of the heart.
8. LAD Apical: Terminal portion of LAD, beginning at the end of previous sement and extending to or beyond the apex.
9. First Diagonal: The first diagonal originating from segment 6 or 7.
9a. First Diagonal a: Additional first diagonal originating from segment 6 or 7, before segment 8.
10. Second Diagonal: Orginating from segment 8 or the transition between segment 7 and 8.
10a. Second Diagonal a: Additional second diagonal originating from segment 8.
11. Proximal Circumflex: Main stem of circumflex from its origin of left main and including origin of first obtuse marginal branch.
12. Intermediate/anterolateral artery: Branch from trifurcating left main other than proximal LAD or LCX. It belongs to the circumflex territory.
12a. Obtuse marginal a: First side branch of circumflex running in general to the area of obtuse margin of the heart.
12b. Obtuse marginal b: Second additional branch of circumflex running in the same direction as 12.
13. Distal Circumflex artery: The stem of circumflex distal to the origin from the most distal obtuse marginal branch, and running along the posterior left atrioventricular groove. Caliber may be small or artery absent.
14. Left Posterolateral: Running to the posterolateral surface of the left ventricle. May be absent or a division of obtuse marginal branch.
14a. Left Posterolateral a: Distal from 14 and running in the same direction.
14b. Left Posterolateral b: Distal from 14 and 14a and running in the same direction.
15. Posterior descending: Most distal part of dominant left circumflex when present. It gives origin to the septal branches. When this artery is present, segment 4 is usually absent.
| Segment No | Segment | Right Dominance Score | Left Dominance Score |
| 1 | RCA Proximal | 1 | 0 |
| 2 | RCA Mid | 1 | 0 |
| 3 | RCA Distal | 1 | 0 |
| 4 | Posterior Descending Artery | 1 | n.a. |
| 16 | Postero-lateral branch from RCA | 0.5 | n.a. |
| 16a | Postero-lateral branch from RCA | 0.5 | n.a. |
| 16b | Postero-lateral branch from RCA | 0.5 | n.a. |
| 16c | Postero-lateral branch from RCA | 0.5 | n.a. |
| 5 | Left Main | 5 | 6 |
| 6 | LAD Proximal | 3.5 | 2.5 |
| 7 | LAD Mid | 2.5 | 2.5 |
| 8 | LAD Apical | 1 | 1 |
| 9 | First Diagonal | 1 | 1 |
| 9a | First Diagonal a | 1 | 1 |
| 10 | Second Diagonal | 0.5 | 0.5 |
| 10a | Second Diagonal a | 0.5 | 0.5 |
| 11 | Proximal Circumflex Artery | 1.5 | 2.5 |
| 12 | Intermediate/anterolateral artery | 1 | 1 |
| 12a | Obtuse marginal a | 1 | 1 |
| 12b | Obtuse marginal b | 1 | 1 |
| 13 | Distal Cicumflex | 0.5 | 1.5 |
| 14 | Left Posterolateral | 0.5 | 1 |
| 14a | Left Posterolateral a | 0.5 | 1 |
| 14b | Left Posterolateral b | 0.5 | 1 |
| 15 | Posterior Descending Artery | n.a. | 1 |
Scoring for Adverse Lesions Characteristics
Adverse lesions are more specifically scored according to their particular characteristic by either multiplying or adding by a certain factor.
| Diameter Reduction | Scoring |
| Total Occlusion | x5 |
| Significant lesion | x2 |
| Total Occlusion | |
| Age> 3months or unknown | +1 |
| Blunt stump | +1 |
| Bridging | +1 |
| First segment visble beyond TO | 1/per non-visible segment |
| Side branch (SB)For both < and ≥1.5 | +1 |
| Aorto ostial stenosis | +1 |
| Severe Totuosity | +2 |
| Lenght >20 mm | +1 |
| Heavy Classification | +2 |
| Thrombus | +1 |
| Diffuse disease/small vessels | +1/ per segment number |
| Trifurcations | |
| 1 diseased segment | +3 |
| 2 diseased segments | +4 |
| 3 diseased segments | +5 |
| 4 diseased segments | +6 |
| Bifurcations | |
| Type A,B,C | +1 |
| Type D,E,F | +2 |
| Angulation <70° | +1 |
Type A lesions are defined as lesions not involving the ostium of side branch, in the main vessel proximal to the ostium of the side branch.
Type B lesions are defined as lesions not involving the ostium of side branch, in the main vessel distal to the ostium of the side branch.
Type C lesions are defined as lesions not involving the ostium of side branch, in the main vessel both proximal and distal to the ostium of the side branch.
Type D lesions are defined as lesions involving the ostium of side branch, in the main vessel proximal and distal to the ostium of the side branch.
Type E lesions are defined as lesions involving only the ostium of side branch.
Type F lesions are defined as lesions involving only the ostium of side branch,in the main vessel proximal to the ostium of the side branch.
Type G lesions are defined as lesions involving only the ostium of side branch,in the main vessel distal to the ostium of the side branch.
- Trifurcations are scored for segments 3/4/16/16a, 5/6/11/12, 11/12a/12b/13, 6/7/9/9a and 7/8/10/10a.
- Bifurcations are scored for segments 5/6/11, 6/7/9, 7/8/10, 11/13/12a, 13/14/14a, 3/4/16 and 13/14/15.
- Severe tortuosity was defined one or more bends of 90° or more, three or more bends of 45° to 90° proximal of the diseased segment.
- Aorto-ostial was defined for immediate origin of coronary arteries from the aorta.
- Diffuse/small vessels disease was defined as diseases involving more then 75% of the of length of the segment of 2 mm vessel diameter.
- Co-dominance is not used as a option while scoring for dominance.
Adapted from publication Sianos G, Morel MA, Kappetein AP; et al. (2005). "The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease". EuroIntervention : Journal of EuroPCR in Collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 1 (2): 219–27. PMID 19758907. Unknown parameter |month= ignored (help)
Clinical SYNTAX Score
There has been a debate over the prognostic implications of the SYNTAX score. To improve this and include clinical variables, a Clinical SYNTAX Score (CSS) was calculated which is
Clinical SYNTAX Score = SYNTAX Score X modified ACEF score
whereby the modified ACEF score is patients age(years), ejection fraction + 1 point for every 10 ml the creatinine clearance \60 ml min per 1.73 m2. Patients with lower scores (less than 15.6) had higher MACCE as compared to patients with high CSS (Clinical SYNTAX Score) i.e. greater than 27. The c-statistic for the CSS was 0.69 and 0.62 for 5 year mortality and for 5-year MACCE respectively. The c-scores for the corresponding SYNTAX score for 5-year mortality and MACCE were 0.62 and 0.59 respectively. Thus, the inclusion of clinical variables in the SYNTAX score improved its prognostic outcomes significantly.
New Risk Stratification Score (NERS)
The New Risk Stratification score was developed as a prognostic score for patients undergoing left main stenting. The score is based upon a total of 54 variables with 17 being clinical, 33 angiographic and 4 procedural. The NERS score was derived from 260 patients who had unprotected left main coronary artery (ULMCA) disease who underwent PCI and stenting. The score was also based upon 337 patients from a left main registry.
A NERS score of more than 25 was associated with a sensitivity of 92.0% and a specificity of 74.1% for MACCE. The New Risk Stratification Score was found to be a superior score with respect to prognosis as compared to the SYNTAX score, but only for patients undergoing left main stenting. Additional studies are needed to further validate the SYNTAX score.
SYNTAX Score II
The SYNTAX II score was designed and validated as an individualized assessment of long-term mortality for patients with complex coronary artery disease (with or without unprotected left main coronary artery disease) proposing to undergo coronary artery bypass graft (CABG) or percutaneous coronary intervention (PCI).[4]
Eight predictors of the SYNTAX II score were identified by applying a multivariable Cox proportional hazards model to the randomized allcomers SYNTAX trial:
- Anatomical SYNTAX score
- Age
- Creatinine clearance (CrCl)
- Left ventricular ejection fraction (LVEF)
- Presence of unprotected left main coronary artery (ULMCA) disease
- Peripheral vascular disease (PVD)
- Female sex
- Chronic obstructive pulmonary disease (COPD)
The SYNTAX score II, calculated as the total points for these eight risk factors, provides an improved prediction of 4-year mortality after PCI or CABG in complex CAD than does the SYNTAX score.
References
- ↑ "SYNTAX Study: TAXUS Drug-Eluting Stent Versus Coronary Artery Bypass Surgery for the Treatment of Narrowed Arteries - Full Text View - ClinicalTrials.gov".
- ↑ "SYNTAX Score".
- ↑ Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW (2009). "Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease". N. Engl. J. Med. 360 (10): 961–72. doi:10.1056/NEJMoa0804626. PMID 19228612. Unknown parameter
|month=ignored (help) - ↑ Farooq, V.; van Klaveren, D.; Steyerberg, EW.; Meliga, E.; Vergouwe, Y.; Chieffo, A.; Kappetein, AP.; Colombo, A.; Holmes, DR. (2013). "Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II". Lancet. 381 (9867): 639–50. doi:10.1016/S0140-6736(13)60108-7. PMID 23439103. Unknown parameter
|month=ignored (help)