Quinidine detailed information
 | |
| Clinical data | |
|---|---|
| Synonyms |
|
| Routes of administration | Oral |
| ATC code | |
| Pharmacokinetic data | |
| Bioavailability | 70-80% |
| Metabolism | 50-90% Hepatic |
| Elimination half-life | 6-8h |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
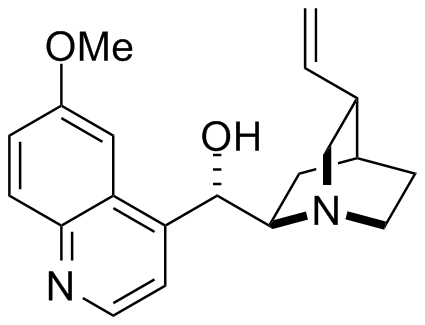
| Formula | C20H24N2O2 |
| Molar mass | 324.417 g/mol |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
For patient information, click here
Quinidine is a pharmaceutical agent that acts as a class I antiarrhythmic agent in the heart. It is a stereoisomer of quinine, originally derived from the bark of the cinchona tree.
Mechanism
Like all other class I antiarrhythmic agents, quinidine primarily works by blocking the fast inward sodium current (INa). Quinidine's effect on INa is known as a use dependent block. This means that at higher heart rates, the block increases, while at lower heart rates the block decreases. The effect of blocking the fast inward sodium current causes the phase 0 depolarization of the cardiac action potential to decrease (decreased Vmax).
Quinidine also blocks the slowly inactivating tetrodotoxin-sensitive Na current, the slow inward calcium current (ICa), the rapid (IKr) and slow (IKs) components of the delayed potassium rectifier current, the inward potassium rectifier current (IKI), the ATP-sensitive potassium channel (IKATP) and Ito.
The effect of quinidine on the ion channels is to prolong the cardiac action potential, thereby prolonging the QT interval on the surface ECG.
Elimination
The half life of oral quinidine is 6 to 8 hours, and it is eliminated by the cytochrome P450 system in the liver. About 20 percent is excreted unchanged via the kidneys.
Side effects and other uses
Quinidine is also an inhibitor of the cytochrome P450 enzyme 2D6, and can lead to increased blood levels of lidocaine, Beta blockers, opioids, and some anti-depressants.
Quinidine also inhibits the transport protein P-glycoprotein and so can cause some peripherally acting drugs such as loperamide to have CNS side effects such as respiratory depression if the two drugs are co-administered.[1]
Intravenous quinidine is also indicated for treatment of P. falciparum malaria.
Quinidine-induced thrombocytopenia (low platelet count) is mediated by the immune system, and may lead to thrombocytic purpura.
Quinidine intoxication can lead to a collection of symptoms collectively known as cinchonism with tinnitus (ringing in the ears) being among the most characteristic and common symptoms of this toxicity syndrome.
Quinidine-based ligands are used in AD-mix-β for Sharpless asymmetric dihydroxylation.
References
- ↑ Sadeque AJ, Wandel C, He H, Shah S, and Wood AJ (2000) Increased drug delivery to the brain by p-glycoprotein inhibition. Clin Pharmacol Ther 68:231–237.
See also
- Pages with script errors
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Drugs with no legal status
- Articles containing unverified chemical infoboxes
- Antiarrhythmic agents
- Quinolines
- Drugs