Pulmonary hypertension physical examination: Difference between revisions
Ralph Matar (talk | contribs) No edit summary |
m (Robot: Changing Category:Disease state to Category:Disease) |
||
| Line 86: | Line 86: | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Pulmonology]] | [[Category:Pulmonology]] | ||
[[Category:Disease | [[Category:Disease]] | ||
[[Category:Mature chapter]] | [[Category:Mature chapter]] | ||
Revision as of 22:39, 9 December 2011
|
Pulmonary Hypertension Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pulmonary hypertension physical examination On the Web |
|
American Roentgen Ray Society Images of Pulmonary hypertension physical examination |
|
Risk calculators and risk factors for Pulmonary hypertension physical examination |
Editor(s)-in-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753; Assistant Editor(s)-in-Chief: Lisa Prior,Ralph Matar,
Overview
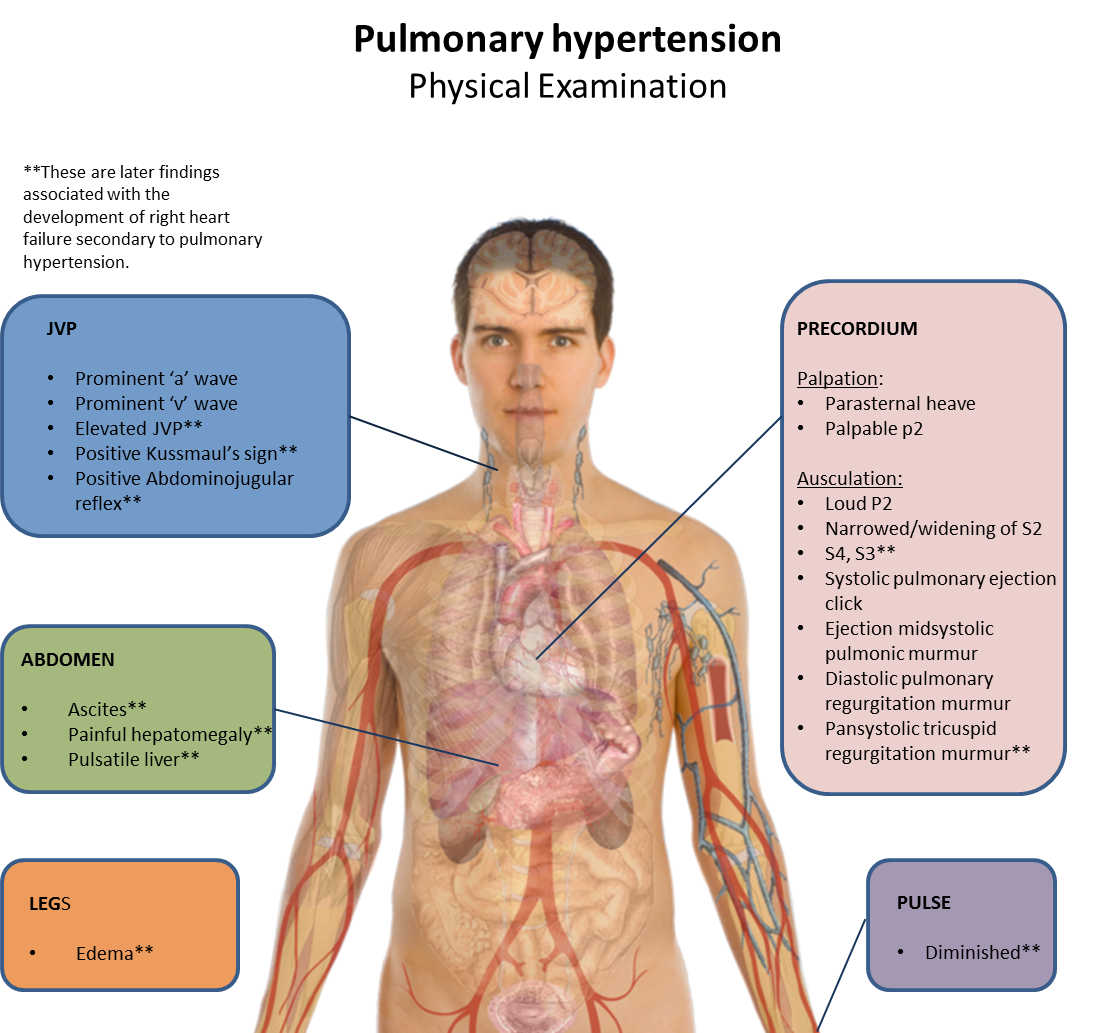
- Physical examination is performed to look for typical signs of pulmonary hypertension.
- Pulmonary hypertension can present with a myriad of physical signs that develop on a spectrum corresponding to the severity of the disease.
- The condition is often initially associated with a loud P2, (para)sternal heave, and narrowed splitting of the second heart sound on physical examination. S3 or third heart sound, and pulmonary regurgitation may also be heard on auscultation.
- As pulmonary hypertension worsens, right ventricular failure can develop, which can present with findings such as increased JVP, ascites and peripheral edema, hepatojugular reflux, and clubbing.
- Physical examination evidence of tricuspid insufficiency is also sought and, if present, is consistent with the presence of long-standing pulmonary hypertension.
A more comprehensive discussion on physical findings is discussed in the sections below categorised by examination site
General appearance
The appearance of the patient may give clues as to the etiology of the condition. For example in COPD, one of the most common causes of pulmonary hypertension, the patient may appear dyspneic with pursed lips breathing and use of accessory muscles. Later on in severe disease, the patient may appear cyanotic with extremities cold to the touch. [1]
Pulse
The pulse may be low volume. This usually occurs in more severe disease. [1]
JVP
Assessment of the JVP in pulmonary hypertension involves assessing the 'a' wave (coincides with atrial contraction), the 'v' wave (coincides with atrial filling) and the height of the JVP column above the sternal angle. Physical findings may include:
- Prominent 'a' wave: due to forced atrial contraction
- Prominent 'v' wave: later if tricuspid regurgitation develops with right ventricular failure.
- Elevated JVP: can be present if right ventricular failure develops
- Postive Kussmaul's sign: JVP elevation during inspiration (the opposite of what normally happens) because of right ventricular failure [1]
- Positive Abdominojugular reflux: JVP rises and remains elevated during a period of over 10 seconds whilst abdominal pressure is applied. This may be present if right ventricular failure develops [1]
Precordium
An holistic precordial assessment of pulmonary hypertension involves palpating the precordium for heaves and thrills and ausculatating to assess first and second heart sounds, splitting of the second heart sound and determining if there any added heart sounds or murmurs. Physical findings may include the following:
Palpation
- Parasternal heave: due to hyperdynamic right ventricle
- Palpable P2: correlates with severe disease [1]
Ausculation
First and second heart sound (S1,S2) assessment
- Loud P2 component of S2: this is due to forceful closure of the valve because of increased pulmonary pressure. It can be heard mostly in pulmonary area (upper right sternal border). If it is evident at the cardiac apex, this indicates more severe disease. It is best appreciated on inspiration. [2]
Splitting of S2 assessment
- Narrowed splitting of S2: in chronic pulmonary hypertension, pulmonary artery compliance decreases leading to earlier pulmonary valve closure and narrowed splitting. [3]
- Widened splitting of S2: widened splitting may occur later if right ventricular failure or bundle branch block develops. [2]
Extra heart sounds assessment
- s4: due to right ventricular hypertrophy and therefore reduced compliance secondary to pulmonary hypertension. It is increased with inspiration.
- s3: if right ventricular failure develops. Increased with inspiration. [1]
Additional sounds assessment
- Systolic pulmonary ejection click: increased with inspiration
Murmurs assessment
- Ejection midsystolic pulmonic murmur: increased with inspiration
- Diastolic pulmonary regurgitation murmur (Graham-Steele murmur): indicates more severe disease
- Pansystolic tricuspuid regurgitation murmur: indicates developing right ventricular failure [4]
Abdomen
Findings in the abdomen include:
- Ascites: indicates right ventricular failure
- Painful hepatomegaly: indicates right ventricular failure
- Pulsatile liver: due to tricuspid regurgitation [1]
Legs
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Simon O'Connor MBBS FRACP DDU; Nicholas P. Hirsch MBBS FRCA FRCP (2009). Clinical Examination: A Systematic Guide to Physical Diagnosis. Edinburgh: Churchill Livingstone. ISBN 0-7295-3905-9.
- ↑ 2.0 2.1 Thompson, Paul Richard; Topol, Eric J.; Califf, Robert M.; Prystowsky, Eric N.; Thomas, James Alan (2007). Textbook of cardiovascular medicine. Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 0-7817-7012-2.
- ↑ Alexander, R. McNeill; Hurst, J. Willis; Schlant, Robert C. (1994). The Heart, arteries and veins. New York: McGraw-Hill, Health Professions Division. ISBN 0-07-055417-X.
- ↑ Clark, Michael; Kumar, Parveen J. (2009). Kumar and Clark's clinical medicine. St. Louis, Mo: Elsevier Saunders. ISBN 0-7020-2993-9.