Providencia
| style="background:#Template:Taxobox colour;"|Providencia | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
 Providencia alcalifaciens
| ||||||||||||
| style="background:#Template:Taxobox colour;" | Scientific classification | ||||||||||||
| ||||||||||||
| Species | ||||||||||||
|
P. stuartii |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
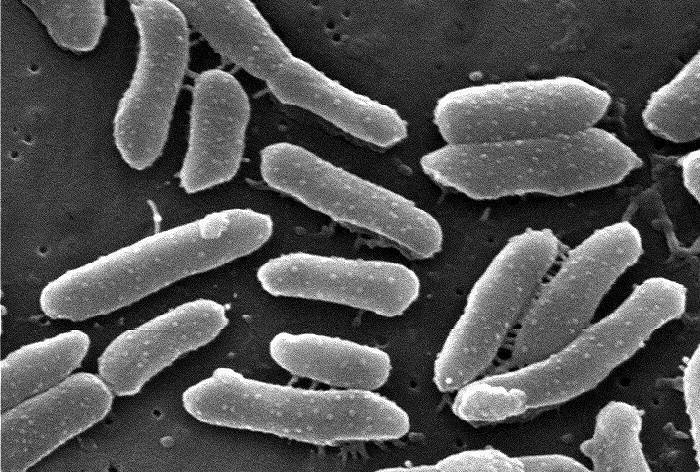
Providencia is a Gram negative, motile bacterium of the family Enterobacteriaceae. Some strains (P. stuartii, for example) are opportunistic pathogens in humans and can cause urinary tract infections, particularly in patients with long-term indwelling urinary catheters or extensive severe burns. Other strains (for example P. burhodogranariea and P. sneebia) are found in the haemolymph of Drosophila melanogaster fruit flies. Some strains are sensitive to ampicillin.
Organism
Role in Disease
Providencia stuartii is the most common Providencia species capable of causing human infections. Providencia stuartii is an opportunistic pathogen seen in patients with severe burns or long-term indwelling urinary catheters. This puts elderly individuals at a greater risk for P. stuartii infections. In animals P. stuartii infections can cause neonatal diarrhea due to P. stuartii infection in dairy cows. In humans, P. stuartii can be isolated from urine (most common), stool, and blood, as well as from sputum, skin, and wound cultures. P. stuartii septicemia is primarily of urinary origin. It is the most common cause of purple urine bag syndrome.[1] Upon physical examination, P stuartii bloodstream infection is associated with fever, tachycardia, and hypotension.
Diagnosis and Testing
Gallery
-
Providencia alcalifaciens bacteria cultured on a blood agar plate (BAP). From Public Health Image Library (PHIL). [2]
Antimicrobial regimen
- Providencia[3]
- 1. Complicated uti/bacteremia/acute prostatitis
- Preferred regimen (1): Ciprofloxacin 500-750 mg PO q12h or 400 mg IV q8-12h
- Preferred regimen (2): Levofloxacin 500 mg IV/PO q24h
- Preferred regimen (3): Piperacillin-Tazobactam 3.375 mg IV q6h
- Preferred regimen (4): Ceftriaxone 1-2 g IV q24h (donot use if ESBL suspected or critically ill)
- Preferred regimen (5): Meropenem 1 g IV q8h (consider if critically ill or ESBL suspected)
- Preferred regimen (6): Amikacin 7.5 mg/kg IV q12h
- Preferred regimen (7): Gentamicin
- Preferred regimen (8): Tobramycin acceptable if susceptible but many species are resistant
- Note (1): Duration of treatment for (UTI) is 7 days common or 3-5 days after defervescence or control/elimination of complicating factors (e.g.,removal of foreign material catheter).
- Note (2): Duration of treatment for (bacteremia) is 10-14 days or 3-5 days after defervescence or control/elimination of complicating factors
- Note (3): Duration for acute prostatitis (2 weeks), shorter than chronic prostatitis (4-6 weeks)
- Alternative regimen: TMP-SMX DS PO q12h for 10-14 days or TMP 5-10 mg/kg/day IV q6h
References
- Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. ISBN 0-8385-8529-9.
- ↑ Lin, CH; Huang HT; Chien CC; et al. (December 2008). "Purple urine bag syndrome in nursing homes: ten elderly case reports and a literature review". Clinical Interventions in Aging. 3 (4): 729–734. PMC 2682405. PMID 19281065.
- ↑ "Public Health Image Library (PHIL)".
- ↑ Bartlett, John (2012). Johns Hopkins ABX guide : diagnosis and treatment of infectious diseases. Burlington, MA: Jones and Bartlett Learning. ISBN 978-1449625580.
![Providencia alcalifaciens bacteria cultured on a blood agar plate (BAP). From Public Health Image Library (PHIL). [2]](/images/e/ef/Enterobacteria42.jpeg)