Pancreatic pseudocyst
| Pancreatic pseudocyst | |
 | |
|---|---|
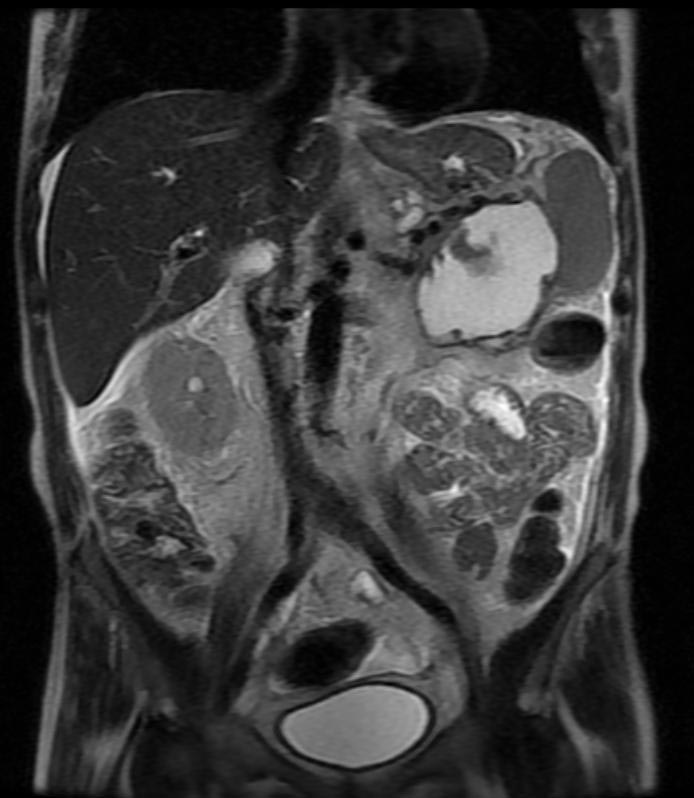
| Pancreatic pseudocyst. Image courtesy of RadsWiki | |
| ICD-10 | K86.3 |
| ICD-9 | 577.2 |
| DiseasesDB | 9530 |
| MedlinePlus | 000272 |
| MeSH | D010192 |
For patient information click here
|
Pancreatic pseudocyst Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pancreatic pseudocyst On the Web |
|
American Roentgen Ray Society Images of Pancreatic pseudocyst |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Contributors: Cafer Zorkun M.D., PhD.
Overview
A pancreatic pseudocyst is a circumscribed collection of fluid rich in amylase and other pancreatic enzymes, blood and necrotic tissue typically located in the lesser sac. It has a non-epithelialised lining made of granulation tissue and hence the name pseudocyst (pseudo - false). By contrast, true cysts have an epithelial lining. This is typically a complication of acute pancreatitis, but may also occur following abdominal trauma. [1]
Pancreatic pseudocysts account for approximately 75% of all pancreatic masses.[2]
Pathophysiology
Acute pancreatitis results amongst other things in the disruption of pancreatic parenchyma and the ductal system. This results in extravasation of pancreatic enzymes which in turn digest the adjoining tissues. This results in a collection of fluid containing pancreatic enzymes, hemolysed blood and necrotic debris around the pancreas. The lesser sac being a potential space, the fluid collects here preferentially. This is called an acute pancreatic collection. Some of these collections resolve on their own as the patient recovers from the acute episode. However, others become more organised and get walled-off within a thick wall of granulation tissue and fibrosis. This takes several weeks to occur and results in a pancreatic pseudocyst.
Causes
Complications and Prognosis
Complications
- A pancreatic abscess can develop if the pseudocyst becomes infected
- Rupture of the pseudocyst
- The pseudocyst may press down on (compress) nearby organs
- Abdominal bleeding
- Shock
Prognosis
The outcome is generally good with treatment.
Diagnosis
History
The questions that need to be answered are:
- Where, how big and how many?
- Is there a communication with the pancreatic ductal system? Draining such a pseudocyst carries an increased risk of pancreatic fistula.
Symptoms
- Abdominal pain - constant pain or deep ache in the abdomen, which may also be felt in the back
- Abdominal mass
- Bloating of the abdomen
- Difficulty eating and digesting food
Physical Examination
Abdomen
Laboratory Findings
Imaging[3]
Ultrasonography
The role of ultrasonography in imaging the pancreas is limited by patient habitus, operator experience and the fact that the pancreas lies behind the stomach (and so a gas-filled stomach will obscure the pancreas).[4][5][6][7]
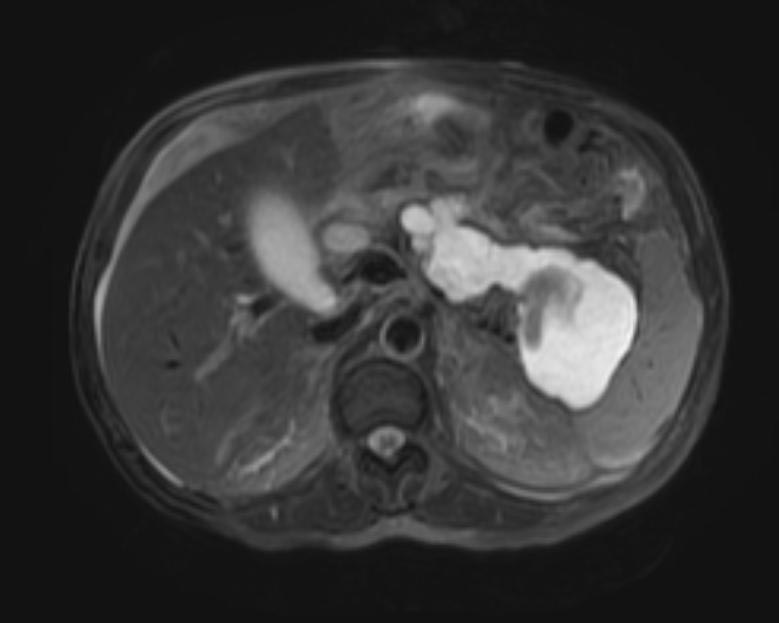
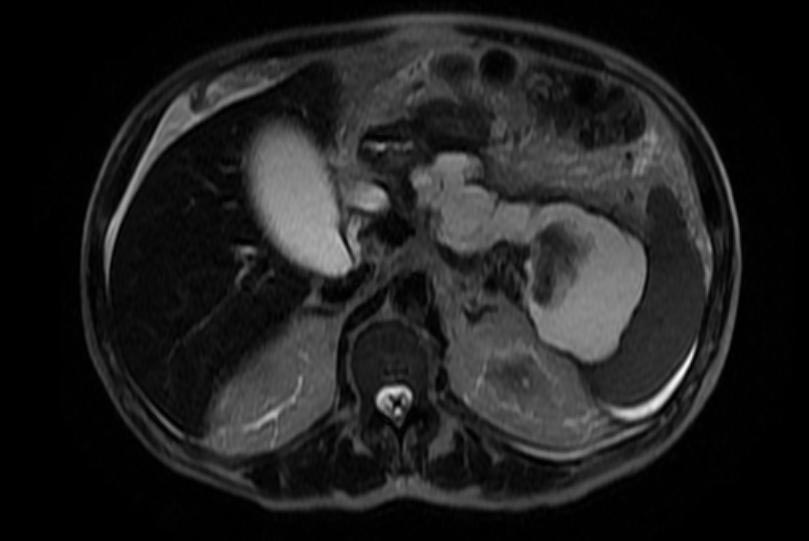
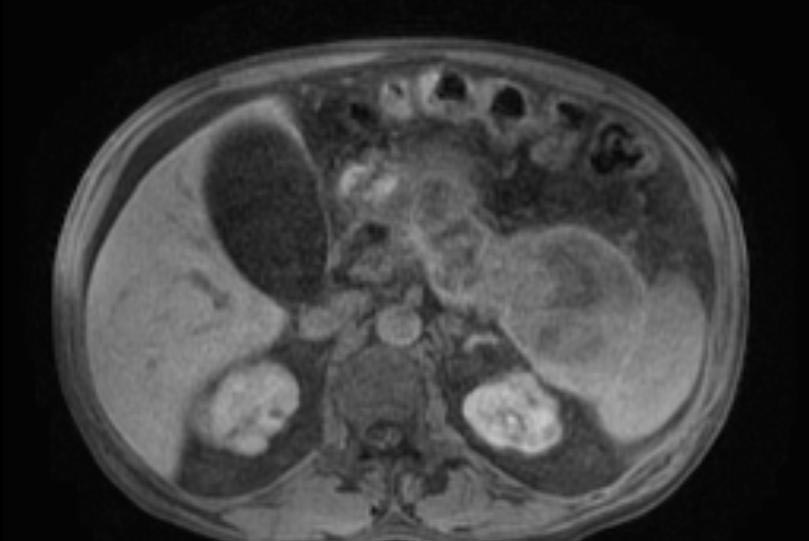
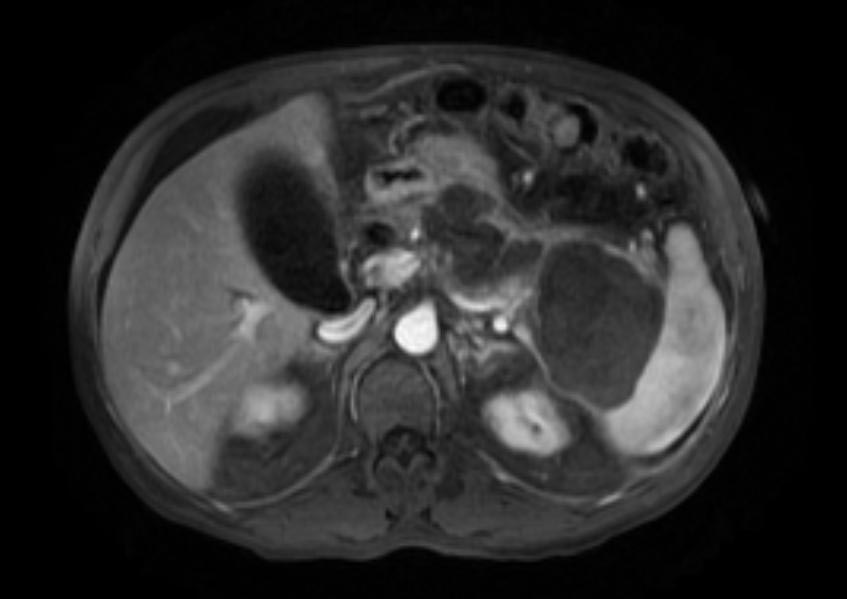
Computerized tomography[8][9]
This is the gold standard for initial assessment and follow-up
-
Pancreatic pseudocyst
-
Pancreatic pseudocyst
-
Pancreatic pseudocyst
-
Pancreatic pseudocyst
-
Pancreatic pseudocyst
-
Pancreatic pseudocyst
Magnetic Resonance Cholangio-pancreatography
To establish the relationship of the pseudocyst to the pancreatic ducts.[10][11][12]
Treatment
A small pseudocyst that is not causing any symptoms may be managed conservatively. However, a large proportion of them will need some form of treatment, The interventions available are:[13][14][15]
- Endoscopic trans-gastric drainage
- Imaging guided percutaneous drainage[16][17][18][19]
- Laparoscopic / open cystogastrostomy[20][21]
References
- ↑ Cooperman AM. An overview of pancreatic pseudocysts: the emperors new clothes revisited. Surg Clin North Am. Apr 2001;81(2):391-7, xii.
- ↑ Bradley EL, Gonzalez AC, Clements JL Jr. Acute pancreatic pseudocysts: incidence and implications. Ann Surg. Dec 1976;184(6):734-7.
- ↑ Kim YH, Saini S, Sahani D, Hahn PF, Mueller PR, Auh YH. Imaging diagnosis of cystic pancreatic lesions: pseudocyst versus nonpseudocyst. Radiographics. May-Jun 2005;25(3):671-85.
- ↑ Aranha GV, Prinz RA, Esguerra AC, Greenlee HB. The nature and course of cystic pancreatic lesions diagnosed by ultrasound. Arch Surg. Apr 1983;118(4):486-8.
- ↑ Brugge WR. The role of endoscopic ultrasound in pancreatic disorders. Int J Pancreatol. Aug 1996;20(1):1-10.
- ↑ Laing FC, Gooding GA, Brown T, Leopold GR. Atypical pseudocysts of the pancreas: an ultrasonographic evaluation. J Clin Ultrasound. Feb 1979;7(1):27-33.
- ↑ Lee CM, Chang-Chien CS, Lin DY, et al. The real-time ultrasonography of pancreatic pseudocyst: comparison of infected and noninfected pseudocysts. J Clin Ultrasound. Jul-Aug 1988;16(6):393-8.
- ↑ Yeo CJ, Bastidas JA, Lynch-Nyhan A, et al. The natural history of pancreatic pseudocysts documented by computed tomography. Surg Gynecol Obstet. May 1990;170(5):411-7.
- ↑ Vick CW, Simeone JF, Ferrucci JT Jr, et al. Pancreatitis-associated fluid collections involving the spleen: sonographic and computed tomographic appearance. Gastrointest Radiol. 1981;6(3):247-50.
- ↑ Dani R, Cundari AM, Nogueira CE, et al. Magnetic resonance cholangiopancreatography in cystic lesions of the pancreas. Pancreas. Apr 2000;20(3):313-8.
- ↑ Megibow AJ, Lavelle MT, Rofsky NM. MR imaging of the pancreas. Surg Clin North Am. Apr 2001;81(2):307-20, ix-x.
- ↑ Morgan DE, Baron TH, Smith JK, et al. Pancreatic fluid collections prior to intervention: evaluation with MR imaging compared with CT and US. Radiology. Jun 1997;203(3):773-8.
- ↑ Beebe DS, Bubrick MP, Onstad GR, Hitchcock CR. Management of pancreatic pseudocysts. Surg Gynecol Obstet. Dec 1984;159(6):562-4.
- ↑ Bradley EL, Clements JL Jr, Gonzalez AC. The natural history of pancreatic pseudocysts: a unified concept of management. Am J Surg. Jan 1979;137(1):135-41.
- ↑ Vitas GJ, Sarr MG. Selected management of pancreatic pseudocysts: operative versus expectant management. Surgery. Feb 1992;111(2):123-30.
- ↑ Adams DB, Anderson MC. Percutaneous catheter drainage compared with internal drainage in the management of pancreatic pseudocyst. Ann Surg. Jun 1992;215(6):571-6; discussion 576-8.
- ↑ Ahlawat SK, Charabaty-Pishvaian A, Jackson PG, Haddad NG. Single-step EUS-guided pancreatic pseudocyst drainage using a large channel linear array echoendoscope and cystotome: results in 11 patients. JOP. 2006;7(6):616-24.
- ↑ Criado E, De Stefano AA, Weiner TM, Jacques PF. Long term results of percutaneous catheter drainage of pancreatic pseudocysts. Surg Gynecol Obstet. Oct 1992;175(4):293-8.
- ↑ vanSonnenberg E, Wittich GR, Casola G, et al. Percutaneous drainage of infected and noninfected pancreatic pseudocysts: experience in 101 cases. Radiology. Mar 1989;170(3 Pt 1):757-61.
- ↑ Barragan B, Love L, Wachtel M, Griswold JA, Frezza EE. A comparison of anterior and posterior approaches for the surgical treatment of pancreatic pseudocyst using laparoscopic cystogastrostomy. J Laparoendosc Adv Surg Tech A. Dec 2005;15(6):596-600.
- ↑ Lang EK, Paolini RM, Pottmeyer A. The efficacy of palliative and definitive percutaneous versus surgical drainage of pancreatic abscesses and pseudocysts: a prospective study of 85 patients. South Med J. Jan 1991;84(1):55-64.