Ocriplasmin: Difference between revisions
No edit summary |
m (Protected "Ocriplasmin": Bot: Protecting all pages from category Drug ([Edit=Allow only administrators] (indefinite) [Move=Allow only administrators] (indefinite))) |
||
| (20 intermediate revisions by one other user not shown) | |||
| Line 3: | Line 3: | ||
|genericName=Ocriplasmin | |genericName=Ocriplasmin | ||
|aOrAn=a | |aOrAn=a | ||
|drugClass=proteolytic enzyme | |drugClass=[[proteolytic enzyme]] | ||
|indicationType=treatment | |indicationType=treatment | ||
|indication=symptomatic vitreomacular adhesion | |indication=symptomatic [[vitreomacular adhesion]] | ||
|adverseReactions= | |adverseReactions=[[blurred vision]], [[conjunctival hemorrhage]], [[macular hole]], [[pain]] in [[eye]], [[photopsia]], [[retinal edema]], [[uveitis]], [[visual impairment]], [[vitreous floaters]] | ||
|blackBoxWarningTitle=<b><span style="color:#FF0000;">TITLE</span></b> | |blackBoxWarningTitle=<b><span style="color:#FF0000;">TITLE</span></b> | ||
|blackBoxWarningBody=<i><span style="color:#FF0000;">Condition Name:</span></i> (Content) | |blackBoxWarningBody=<i><span style="color:#FF0000;">Condition Name:</span></i> (Content) | ||
|fdaLIADAdult= | |fdaLIADAdult=* Ocriplasmin® is a proteolytic enzyme indicated for the treatment of symptomatic vitreomacular [[adhesion]]. | ||
=====General Dosing Information===== | |||
Must be diluted before use. For single-use ophthalmic intravitreal injection only. | * Must be diluted before use. For single-use ophthalmic intravitreal [[injection]] only. Ocriplasmin must only be administered by a qualified physician. | ||
=====Dosing===== | |||
* The recommended dose is 0.125 mg (0.1 mL of the diluted solution) administered by intravitreal [[injection]] to the affected [[eye]] once as a single dose. | |||
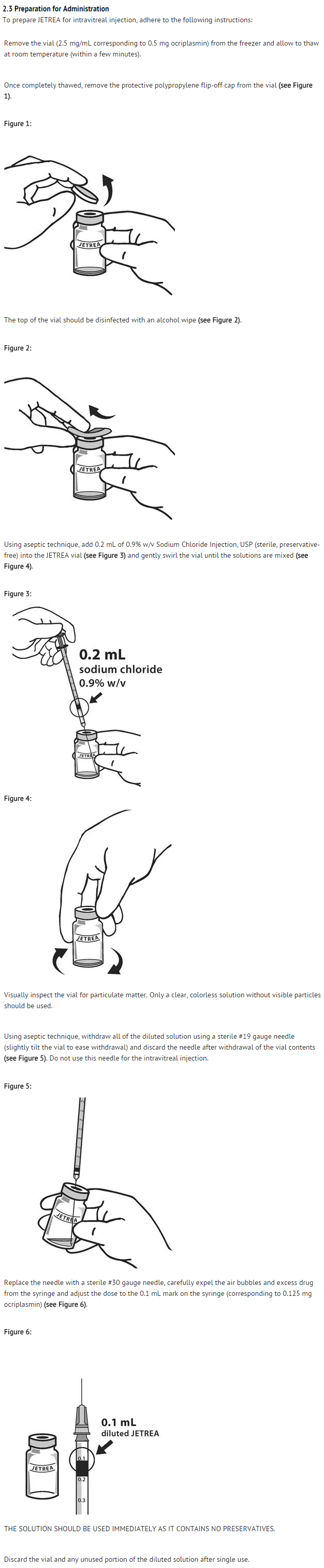
=====Preparation for Administration===== | |||
The recommended dose is 0.125 mg (0.1 mL of the diluted solution) administered by intravitreal injection to the affected eye once as a single dose. | : [[File:Ocri - Dosage 01.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
=====Administration and Monitoring===== | |||
* The intravitreal [[injection]] procedure should be carried out under controlled aseptic conditions, which include the use of sterile gloves, a sterile drape and a sterile [[eyelid]] speculum (or equivalent). Adequate [[anesthesia]] and a broad spectrum microbiocide should be administered according to standard medical practice. | |||
* The injection needle should be inserted 3.5-4.0 mm posterior to the [[limbus]] aiming towards the center of the [[vitreous cavity]], avoiding the horizontal meridian. The injection volume of 0.1 mL is then delivered into the mid-vitreous. | |||
* Immediately following the intravitreal [[injection]], patients should be monitored for elevation in [[intraocular pressure]]. Appropriate monitoring may consist of a check for perfusion of the optic nerve head or [[tonometry]]. If required, a sterile [[paracentesis]] needle should be available. | |||
* Following intravitreal [[injection]], patients should be instructed to report any symptoms suggestive of [[endophthalmitis]] or [[retinal detachment]] (e.g., eye pain, redness of the [[eye]], [[photophobia]], blurred or decreased vision) without delay. | |||
* Each vial should only be used to provide a single injection for the treatment of a single [[eye]]. If the contralateral [[eye]] requires treatment, a new vial should be used and the sterile field, syringe, gloves, drapes, [[eyelid]] speculum, and injection needles should be changed before Ocriplasmin is administered to the other [[eye]], however, treatment with Ocriplasmin in the other eye is not recommended within 7 days of the initial injection in order to monitor the post-injection course including the potential for decreased vision in the injected [[eye]]. | |||
: [[File: | |||
The intravitreal injection procedure should be carried out under controlled aseptic conditions, which include the use of sterile gloves, a sterile drape and a sterile eyelid speculum (or equivalent). Adequate anesthesia and a broad spectrum microbiocide should be administered according to standard medical practice. | |||
The injection needle should be inserted 3.5-4.0 mm posterior to the limbus aiming towards the center of the vitreous cavity, avoiding the horizontal meridian. The injection volume of 0.1 mL is then delivered into the mid-vitreous. | |||
Immediately following the intravitreal injection, patients should be monitored for elevation in intraocular pressure. Appropriate monitoring may consist of a check for perfusion of the optic nerve head or tonometry. If required, a sterile paracentesis needle should be available. | |||
Following intravitreal injection, patients should be instructed to report any symptoms suggestive of endophthalmitis or retinal detachment (e.g., eye pain, redness of the eye, photophobia, blurred or decreased vision) without delay | |||
Each vial should only be used to provide a single injection for the treatment of a single eye. If the contralateral eye requires treatment, a new vial should be used and the sterile field, syringe, gloves, drapes, eyelid speculum, and injection needles should be changed before | |||
|offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Ocriplasmin in adult patients. | |offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Ocriplasmin in adult patients. | ||
|offLabelAdultNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Ocriplasmin in adult patients. | |offLabelAdultNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Ocriplasmin in adult patients. | ||
| Line 40: | Line 27: | ||
|offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Ocriplasmin in pediatric patients. | |offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Ocriplasmin in pediatric patients. | ||
|contraindications=None | |contraindications=None | ||
|warnings= | |warnings======Decreased Vision===== | ||
A decrease of ≥ 3 line of best corrected visual acuity (BCVA) was experienced by 5.6% of patients treated with | * A decrease of ≥ 3 line of best corrected visual acuity (BCVA) was experienced by 5.6% of patients treated with Ocriplasmin and 3.2% of patients treated with vehicle in the controlled trials. | ||
* The majority of these decreases in vision were due to progression of the condition with traction and many required surgical intervention. Patients should be monitored appropriately. | |||
=====Intravitreal Injection Procedure Associated Effects===== | |||
* Intravitreal injections are associated with intraocular inflammation / infection, [[intraocular hemorrhage]] and increased [[intraocular pressure]] (IOP). In the controlled trials, intraocular inflammation occurred in 7.1% of patients injected with Ocriplasmin vs. 3.7% of patients injected with vehicle. Most of the post-injection intraocular inflammation events were mild and transient. Intraocular [[hemorrhage]] occurred in 2.4% vs. 3.7% of patients injected with Ocriplasmin vs. vehicle, respectively. Increased [[intraocular pressure]] occurred in 4.1% vs. 5.3% of patients injected with Ocriplasmin vs. vehicle, respectively. | |||
=====Potential for Lens Subluxation===== | |||
* One case of [[lens]] subluxation was reported in a premature infant who received an [[intravitreal injection]] of 0.175 mg (1.4 times higher than the recommended dose). [[Lens subluxation]] was observed in three animal species (monkey, rabbit, minipig) following a single [[intravitreal injection]] that achieved vitreous concentrations of ocriplasmin 1.4 times higher than achieved with the recommended treatment dose. Administration of a second intravitreal dose in monkeys, 28 days apart, produced [[lens subluxation]] in 100% of the treated [[eyes]]. | |||
=====Retinal Breaks===== | |||
* In the controlled trials, the incidence of [[retinal detachment]] was 0.9% in the Ocriplasmin group and 1.6% in the vehicle group, while the incidence of retinal tear (without detachment) was 1.1% in the Ocriplasmin group and 2.7% in the vehicle group. Most of these events occurred during or after [[vitrectomy]] in both groups. The incidence of retinal detachment that occurred [[pre-vitrectomy]] was 0.4% in the Ocriplasmin group and none in the vehicle group, while the incidence of retinal tear (without detachment) that occurred [[pre-vitrectomy]] was none in the Ocriplasmin group and 0.5% in the vehicle group. | |||
=====Dyschromatopsia===== | |||
* [[Dyschromatopsia]] (generally described as yellowish vision) was reported in 2% of all patients injected with Ocriplasmin. In approximately half of these dyschromatopsia cases there were also electroretinographic (ERG) changes reported (a- and b-wave amplitude decrease). | |||
|clinicalTrials=The following adverse reactions are described below and elsewhere in the labeling: | |||
:* Decreased [[Vision]]. | |||
:* [[Intravitreal Injection]] Procedure Associated Effects. | |||
:* Potential for [[Lens Subluxation]]. | |||
:* Retinal Breaks. | |||
=====Clinical Trials Experience===== | |||
* Because clinical trials are conducted under widely varying conditions, adverse reaction rates in one clinical trial of a drug cannot be directly compared with rates in the clinical trials of the same or another drug and may not reflect the rates observed in practice. | |||
* Approximately 800 patients have been treated with an intravitreal injection of Ocriplasmin. Of these, 465 patients received an intravitreal injection of ocriplasmin 0.125 mg (187 patients received vehicle) in the 2 vehicle-controlled studies (Study 1 and Study 2). | |||
* The most common adverse reactions (incidence 5% - 20% listed in descending order of frequency) in the vehicle-controlled clinical studies were: [[vitreous floaters]], [[conjunctival hemorrhage]], [[eye pain]], [[photopsia]], blurred vision, [[macular hole]], reduced visual acuity, visual impairment, and [[retinal edema]]. | |||
* Less common adverse reactions observed in the studies at a frequency of 2% - < 5% in patients treated with Ocriplasmin included [[macular edema]], increased intraocular pressure, anterior chamber cell, [[photophobia]], vitreous detachment, ocular discomfort, iritis, cataract, dry eye, metamorphopsia, [[conjunctival hyperemia]], and [[retinal degeneration]]. | |||
* [[Dyschromatopsia]] was reported in 2% of patients injected with Ocriplasmin, with the majority of cases reported from two uncontrolled clinical studies. In approximately half of these [[dyschromatopsia]] cases there were also electroretinographic (ERG) changes reported (a- and b-wave amplitude decrease). | |||
=====Immunogenicity===== | |||
* As with all therapeutic proteins, there is potential for [[immunogenicity]]. [[Immunogenicity]] for this product has not been evaluated. | |||
|FDAPregCat=C | |||
|useInPregnancyFDA=* Animal reproduction studies have not been conducted with ocriplasmin. There are no adequate and well-controlled studies of ocriplasmin in [[pregnant]] women. | |||
* It is not known whether ocriplasmin can cause fetal harm when administered to a [[pregnant]] woman or can affect reproduction capacity. The systemic exposure to ocriplasmin is expected to be low after [[intravitreal injection]] of a single 0.125 mg dose. Assuming 100% systemic absorption (and a plasma volume of 2700 mL), the estimated plasma concentration is 46 ng/mL. Ocriplasmin should be given to a [[pregnant]] woman only if clearly needed. | |||
|useInNursing=* It is not known whether ocriplasmin is excreted in human [[milk]]. Because many drugs are excreted in human [[milk]], and because the potential for absorption and harm to infant growth and development exists, caution should be exercised when Ocriplasmin is administered to a nursing woman. | |||
|useInPed=* The use of Ocriplasmin in pediatric patients is not recommended. A single center, randomized, placebo controlled, double masked clinical study to investigate the safety and efficacy of a single intravitreal [[injection]] of 0.175 mg ocriplasmin in pediatric subjects as an adjunct to [[vitrectomy]] was conducted in 24 eyes of 22 patients. There were no statistical or clinical differences between groups for the induction of total [[macular PVD]], any of the secondary endpoints or adverse events. | |||
|useInGeri=* In the clinical studies, 384 and 145 patients were ≥ 65 years and of these 192 and 73 patients were ≥ 75 years in the Ocriplasmin and vehicle groups respectively. No significant differences in efficacy or safety were seen with increasing age in these studies. | |||
|administration=* [[Intravitreal injection]] | |||
|monitoring=* Patients should be monitored and instructed to report any symptoms without delay. | |||
* Immediately following the intravitreal injection, patients should be monitored for elevation in [[intraocular pressure]]. | |||
|overdose=* The clinical data on the effects of Ocriplasmin overdose are limited. One case of accidental overdose of 0.250 mg ocriplasmin (twice the recommended dose) was reported to be associated with inflammation and a decrease in visual acuity. | |||
|drugBox={{Infobox drug | |||
| IUPAC_name = | |||
| image = | |||
| alt = | |||
| caption = | |||
<!-- Clinical data --> | |||
| tradename = JETREA | |||
| Drugs.com = {{Drugs.com|parent|JETREA}} | |||
| MedlinePlus = | |||
| pregnancy_AU = <!-- A / B1 / B2 / B3 / C / D / X --> | |||
| pregnancy_US = C | |||
| pregnancy_category= | |||
| legal_AU = <!-- S2, S3, S4, S5, S6, S7, S8, S9 or Unscheduled--> | |||
| legal_CA = <!-- OTC, Rx-only, Schedule I, II, III, IV, V, VI, VII, VIII --> | |||
| legal_UK = <!-- GSL, P, POM, CD, CD Lic, CD POM, CD No Reg POM, CD (Benz) POM, CD (Anab) POM or CD Inv POM --> | |||
| legal_US = Rx-only | |||
| legal_status = | |||
| routes_of_administration = [[Intravitreal administration|Intravitreal]] | |||
<!-- Pharmacokinetic data --> | |||
| bioavailability = | |||
| protein_bound = | |||
| metabolism = | |||
| elimination_half-life = | |||
| excretion = | |||
<!-- Identifiers --> | |||
| CAS_number = | |||
| ATCvet = | |||
| ATC_prefix = S01 | |||
| ATC_suffix = XA22 | |||
| PubChem = | |||
| DrugBank = DB08888 | |||
| UNII_Ref = {{fdacite|correct|FDA}} | |||
| UNII = 7V6HE3DM5A | |||
| ChemSpiderID = NA | |||
<!-- Chemical data --> | |||
| C=1214 | H=1890 | N=338 | O=348 | S=14 | |||
| molecular_weight = 27.25 [[kDa]] | |||
}} | |||
|mechAction=* Ocriplasmin has proteolytic activity against protein components of the vitreous body and the vitreoretinal interface (VRI) (e.g. [[laminin]], [[fibronectin]] and [[collagen]]), thereby dissolving the protein matrix responsible for the vitreomacular adhesion (VMA). | |||
|structure=* Ocriplasmin is a recombinant truncated form of human [[plasmin]] with a molecular weight of 27.2 kDa produced by recombinant [[DNA]] technology in a Pichia pastoris expression system. | |||
* JETREA is a sterile, clear and colorless solution with no preservatives in a single-use glass vial containing 0.5 mg ocriplasmin in 0.2 mL solution for intravitreal injection after dilution. | |||
* Each vial contains 0.5 mg ocriplasmin (active) and 0.21 mg citric acid, 0.75 mg [[mannitol]], sodium hydroxide (for pH adjustment) and water for injection. The pH of the solution is 3.1. | |||
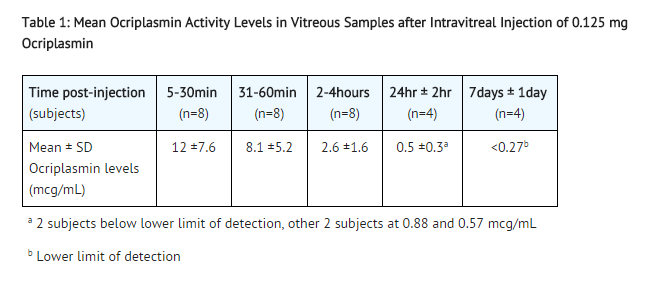
|PK=* The intravitreal pharmacokinetics of ocriplasmin were determined in a clinical study in patients scheduled for vitrectomy where 0.125 mg ocriplasmin (corresponding to an average concentration of 29 mcg ocriplasmin per mL vitreous volume [approximately 4.3 mL/eye]) was administered as a single intravitreal dose at different time points prior to [[vitrectomy]]. The mean ocriplasmin activity levels decreased with time from injection to time of sampling as illustrated in Table 1, according to a second order kinetic process. At 24 hours post injection the levels in the vitreous were below 3% of the theoretical concentration reached immediately after [[injection]]. | |||
* Because of the small dose administered (0.125 mg), detectable levels of ocriplasmin in systemic circulation are not expected after [[intravitreal injection]]. | |||
: [[File:Ocri 02 Pk.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
|nonClinToxic======Carcinogenesis, Mutagenesis, Impairment of Fertility===== | |||
* No carcinogenicity, mutagenicity or reproductive and developmental toxicity studies were conducted with ocriplasmin. | |||
=====Animal Toxicology and/or Pharmacology===== | |||
* The ocular toxicity of ocriplasmin after a single intravitreal dose has been evaluated in rabbits, monkeys and minipigs. Ocriplasmin induced an inflammatory response and transient ERG changes in rabbits and monkeys, which tended to resolve over time. [[Lens subluxation]] was observed in the 3 species at ocriplasmin concentrations in the vitreous at or above 41 mcg/mL, a concentration 1.4-fold above the intended clinical concentration in the vitreous of 29 mcg/mL. Intraocular hemorrhage was observed in rabbits and monkeys. | |||
* A second intravitreal administration of ocriplasmin (28 days apart) in monkeys at doses of 75 mcg/eye (41 mcg/mL vitreous) or 125 mcg/eye (68 mcg/mL vitreous) was associated with [[lens subluxation]] in all ocriplasmin treated eyes. Sustained increases in IOP occurred in two animals with lens subluxation. Microscopic findings in the [[eye]] included [[vitreous liquefaction]], degeneration/disruption of the hyaloideocapsular ligament (with loss of ciliary zonular fibers), lens degeneration, [[mononuclear cell]] infiltration of the vitreous, and vacuolation of the retinal inner nuclear cell layer. These doses are 1.4-fold and 2.3-fold the intended clinical concentration in the vitreous of 29 mcg/mL, respectively. | |||
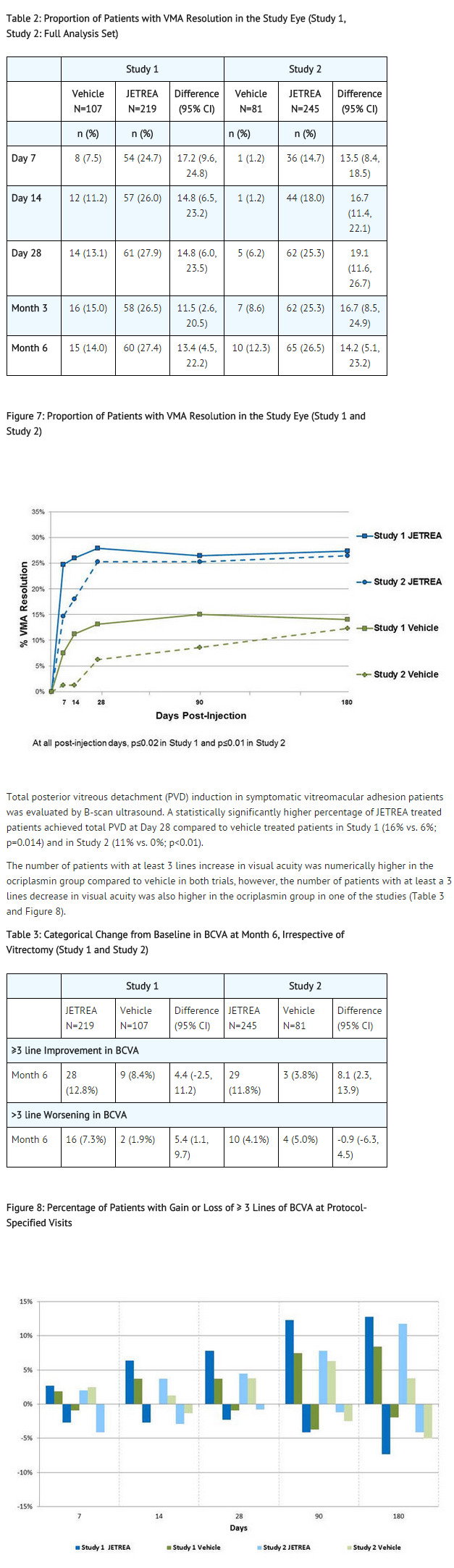
|clinicalStudies=* The efficacy and safety of JETREA was demonstrated in two multicenter, randomized, double masked, vehicle-controlled, 6 month studies in patients with symptomatic vitreomacular adhesion (VMA). A total of 652 patients (JETREA 464, vehicle 188) were randomized in these 2 studies. Randomization was 2:1 (JETREA:vehicle) in Study 1 and 3:1 in Study 2. | |||
* Patients were treated with a single injection of JETREA or vehicle. In both of the studies, the proportion of patients who achieved VMA resolution at Day 28 (i.e., achieved success on the primary endpoint) was significantly higher in the ocriplasmin group compared with the vehicle group through Month 6 (Table 2 and Figure 7). | |||
: [[File:Ocri CLinical 03.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
|howSupplied=* Each vial of JETREA contains 0.5 mg ocriplasmin in 0.2 mL citric-buffered solution (2.5 mg/mL). JETREA is supplied in a 2 mL glass vial with a latex free rubber stopper. Vials are for single use only. | |||
:* NDC 24856-001-00 | |||
|storage=* Store frozen at or below -4°F (-20°C). Protect the vials from light by storing in the original package until time of use. | |||
|packLabel=[[File:Ocri 04.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
[[File:Ocri 05.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
[[File:DailyMed - JETREA- ocriplasmin injection, solution .png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
|fdaPatientInfo=* In the days following JETREA administration, patients are at risk of developing intraocular inflammation/infection. Advise patients to seek immediate care from an ophthalmologist if the eye becomes red, sensitive to light, painful, or develops a change in vision.* Patients may experience temporary visual impairment after receiving an intravitreal injection of JETREA . Advise patients to not drive or operate heavy machinery until this visual impairment has resolved. If visual impairment persists or decreases further, advise patients to seek care from an ophthalmologist. | |||
|alcohol=Alcohol-Ocriplasmin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |||
|brandNames=* JETREA®<ref>{{Cite web | title = JETREA- ocriplasmin injection, solution | url =http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=390682b7-72c4-11e1-b0c4-0800200c9a66#section-2.4 }}</ref> | |||
<!--Look-Alike Drug Names--> | |||
}} | |||
{{LabelImage | |||
|fileName=Ocri 04.jpg | |||
}} | |||
{{LabelImage | |||
|fileName=Ocri 05.jpg | |||
}} | |||
{{LabelImage | |||
|fileName=DailyMed - JETREA- ocriplasmin injection, solution .png | |||
}} | |||
<!--Drug Shortage Status--> | |||
<!--Pill Image--> | |||
<!--Label Display Image--> | |||
<!--Category--> | |||
[[Category:Drug]] | |||
[[Category:Pharmacology]] | |||
Latest revision as of 16:50, 20 August 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Ocriplasmin is a proteolytic enzyme that is FDA approved for the treatment of symptomatic vitreomacular adhesion. Common adverse reactions include blurred vision, conjunctival hemorrhage, macular hole, pain in eye, photopsia, retinal edema, uveitis, visual impairment, vitreous floaters.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- Ocriplasmin® is a proteolytic enzyme indicated for the treatment of symptomatic vitreomacular adhesion.
General Dosing Information
- Must be diluted before use. For single-use ophthalmic intravitreal injection only. Ocriplasmin must only be administered by a qualified physician.
Dosing
- The recommended dose is 0.125 mg (0.1 mL of the diluted solution) administered by intravitreal injection to the affected eye once as a single dose.
Preparation for Administration
Administration and Monitoring
- The intravitreal injection procedure should be carried out under controlled aseptic conditions, which include the use of sterile gloves, a sterile drape and a sterile eyelid speculum (or equivalent). Adequate anesthesia and a broad spectrum microbiocide should be administered according to standard medical practice.
- The injection needle should be inserted 3.5-4.0 mm posterior to the limbus aiming towards the center of the vitreous cavity, avoiding the horizontal meridian. The injection volume of 0.1 mL is then delivered into the mid-vitreous.
- Immediately following the intravitreal injection, patients should be monitored for elevation in intraocular pressure. Appropriate monitoring may consist of a check for perfusion of the optic nerve head or tonometry. If required, a sterile paracentesis needle should be available.
- Following intravitreal injection, patients should be instructed to report any symptoms suggestive of endophthalmitis or retinal detachment (e.g., eye pain, redness of the eye, photophobia, blurred or decreased vision) without delay.
- Each vial should only be used to provide a single injection for the treatment of a single eye. If the contralateral eye requires treatment, a new vial should be used and the sterile field, syringe, gloves, drapes, eyelid speculum, and injection needles should be changed before Ocriplasmin is administered to the other eye, however, treatment with Ocriplasmin in the other eye is not recommended within 7 days of the initial injection in order to monitor the post-injection course including the potential for decreased vision in the injected eye.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Ocriplasmin in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Ocriplasmin in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Ocriplasmin FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Ocriplasmin in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Ocriplasmin in pediatric patients.
Contraindications
None
Warnings
Decreased Vision
- A decrease of ≥ 3 line of best corrected visual acuity (BCVA) was experienced by 5.6% of patients treated with Ocriplasmin and 3.2% of patients treated with vehicle in the controlled trials.
- The majority of these decreases in vision were due to progression of the condition with traction and many required surgical intervention. Patients should be monitored appropriately.
Intravitreal Injection Procedure Associated Effects
- Intravitreal injections are associated with intraocular inflammation / infection, intraocular hemorrhage and increased intraocular pressure (IOP). In the controlled trials, intraocular inflammation occurred in 7.1% of patients injected with Ocriplasmin vs. 3.7% of patients injected with vehicle. Most of the post-injection intraocular inflammation events were mild and transient. Intraocular hemorrhage occurred in 2.4% vs. 3.7% of patients injected with Ocriplasmin vs. vehicle, respectively. Increased intraocular pressure occurred in 4.1% vs. 5.3% of patients injected with Ocriplasmin vs. vehicle, respectively.
Potential for Lens Subluxation
- One case of lens subluxation was reported in a premature infant who received an intravitreal injection of 0.175 mg (1.4 times higher than the recommended dose). Lens subluxation was observed in three animal species (monkey, rabbit, minipig) following a single intravitreal injection that achieved vitreous concentrations of ocriplasmin 1.4 times higher than achieved with the recommended treatment dose. Administration of a second intravitreal dose in monkeys, 28 days apart, produced lens subluxation in 100% of the treated eyes.
Retinal Breaks
- In the controlled trials, the incidence of retinal detachment was 0.9% in the Ocriplasmin group and 1.6% in the vehicle group, while the incidence of retinal tear (without detachment) was 1.1% in the Ocriplasmin group and 2.7% in the vehicle group. Most of these events occurred during or after vitrectomy in both groups. The incidence of retinal detachment that occurred pre-vitrectomy was 0.4% in the Ocriplasmin group and none in the vehicle group, while the incidence of retinal tear (without detachment) that occurred pre-vitrectomy was none in the Ocriplasmin group and 0.5% in the vehicle group.
Dyschromatopsia
- Dyschromatopsia (generally described as yellowish vision) was reported in 2% of all patients injected with Ocriplasmin. In approximately half of these dyschromatopsia cases there were also electroretinographic (ERG) changes reported (a- and b-wave amplitude decrease).
Adverse Reactions
Clinical Trials Experience
The following adverse reactions are described below and elsewhere in the labeling:
- Decreased Vision.
- Intravitreal Injection Procedure Associated Effects.
- Potential for Lens Subluxation.
- Retinal Breaks.
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates in one clinical trial of a drug cannot be directly compared with rates in the clinical trials of the same or another drug and may not reflect the rates observed in practice.
- Approximately 800 patients have been treated with an intravitreal injection of Ocriplasmin. Of these, 465 patients received an intravitreal injection of ocriplasmin 0.125 mg (187 patients received vehicle) in the 2 vehicle-controlled studies (Study 1 and Study 2).
- The most common adverse reactions (incidence 5% - 20% listed in descending order of frequency) in the vehicle-controlled clinical studies were: vitreous floaters, conjunctival hemorrhage, eye pain, photopsia, blurred vision, macular hole, reduced visual acuity, visual impairment, and retinal edema.
- Less common adverse reactions observed in the studies at a frequency of 2% - < 5% in patients treated with Ocriplasmin included macular edema, increased intraocular pressure, anterior chamber cell, photophobia, vitreous detachment, ocular discomfort, iritis, cataract, dry eye, metamorphopsia, conjunctival hyperemia, and retinal degeneration.
- Dyschromatopsia was reported in 2% of patients injected with Ocriplasmin, with the majority of cases reported from two uncontrolled clinical studies. In approximately half of these dyschromatopsia cases there were also electroretinographic (ERG) changes reported (a- and b-wave amplitude decrease).
Immunogenicity
- As with all therapeutic proteins, there is potential for immunogenicity. Immunogenicity for this product has not been evaluated.
Postmarketing Experience
There is limited information regarding Ocriplasmin Postmarketing Experience in the drug label.
Drug Interactions
There is limited information regarding Ocriplasmin Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
- Animal reproduction studies have not been conducted with ocriplasmin. There are no adequate and well-controlled studies of ocriplasmin in pregnant women.
- It is not known whether ocriplasmin can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. The systemic exposure to ocriplasmin is expected to be low after intravitreal injection of a single 0.125 mg dose. Assuming 100% systemic absorption (and a plasma volume of 2700 mL), the estimated plasma concentration is 46 ng/mL. Ocriplasmin should be given to a pregnant woman only if clearly needed.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Ocriplasmin in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Ocriplasmin during labor and delivery.
Nursing Mothers
- It is not known whether ocriplasmin is excreted in human milk. Because many drugs are excreted in human milk, and because the potential for absorption and harm to infant growth and development exists, caution should be exercised when Ocriplasmin is administered to a nursing woman.
Pediatric Use
- The use of Ocriplasmin in pediatric patients is not recommended. A single center, randomized, placebo controlled, double masked clinical study to investigate the safety and efficacy of a single intravitreal injection of 0.175 mg ocriplasmin in pediatric subjects as an adjunct to vitrectomy was conducted in 24 eyes of 22 patients. There were no statistical or clinical differences between groups for the induction of total macular PVD, any of the secondary endpoints or adverse events.
Geriatic Use
- In the clinical studies, 384 and 145 patients were ≥ 65 years and of these 192 and 73 patients were ≥ 75 years in the Ocriplasmin and vehicle groups respectively. No significant differences in efficacy or safety were seen with increasing age in these studies.
Gender
There is no FDA guidance on the use of Ocriplasmin with respect to specific gender populations.
Race
There is no FDA guidance on the use of Ocriplasmin with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Ocriplasmin in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Ocriplasmin in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Ocriplasmin in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Ocriplasmin in patients who are immunocompromised.
Administration and Monitoring
Administration
Monitoring
- Patients should be monitored and instructed to report any symptoms without delay.
- Immediately following the intravitreal injection, patients should be monitored for elevation in intraocular pressure.
IV Compatibility
There is limited information regarding the compatibility of Ocriplasmin and IV administrations.
Overdosage
- The clinical data on the effects of Ocriplasmin overdose are limited. One case of accidental overdose of 0.250 mg ocriplasmin (twice the recommended dose) was reported to be associated with inflammation and a decrease in visual acuity.
Pharmacology
| Clinical data | |
|---|---|
| Trade names | JETREA |
| AHFS/Drugs.com | JETREA |
| Pregnancy category |
|
| Routes of administration | Intravitreal |
| ATC code | |
| Legal status | |
| Legal status |
|
| Identifiers | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C1214H1890N338O348S14 |
| Molar mass | 27.25 kDa |
Mechanism of Action
- Ocriplasmin has proteolytic activity against protein components of the vitreous body and the vitreoretinal interface (VRI) (e.g. laminin, fibronectin and collagen), thereby dissolving the protein matrix responsible for the vitreomacular adhesion (VMA).
Structure
- Ocriplasmin is a recombinant truncated form of human plasmin with a molecular weight of 27.2 kDa produced by recombinant DNA technology in a Pichia pastoris expression system.
- JETREA is a sterile, clear and colorless solution with no preservatives in a single-use glass vial containing 0.5 mg ocriplasmin in 0.2 mL solution for intravitreal injection after dilution.
- Each vial contains 0.5 mg ocriplasmin (active) and 0.21 mg citric acid, 0.75 mg mannitol, sodium hydroxide (for pH adjustment) and water for injection. The pH of the solution is 3.1.
Pharmacodynamics
There is limited information regarding Ocriplasmin Pharmacodynamics in the drug label.
Pharmacokinetics
- The intravitreal pharmacokinetics of ocriplasmin were determined in a clinical study in patients scheduled for vitrectomy where 0.125 mg ocriplasmin (corresponding to an average concentration of 29 mcg ocriplasmin per mL vitreous volume [approximately 4.3 mL/eye]) was administered as a single intravitreal dose at different time points prior to vitrectomy. The mean ocriplasmin activity levels decreased with time from injection to time of sampling as illustrated in Table 1, according to a second order kinetic process. At 24 hours post injection the levels in the vitreous were below 3% of the theoretical concentration reached immediately after injection.
- Because of the small dose administered (0.125 mg), detectable levels of ocriplasmin in systemic circulation are not expected after intravitreal injection.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- No carcinogenicity, mutagenicity or reproductive and developmental toxicity studies were conducted with ocriplasmin.
Animal Toxicology and/or Pharmacology
- The ocular toxicity of ocriplasmin after a single intravitreal dose has been evaluated in rabbits, monkeys and minipigs. Ocriplasmin induced an inflammatory response and transient ERG changes in rabbits and monkeys, which tended to resolve over time. Lens subluxation was observed in the 3 species at ocriplasmin concentrations in the vitreous at or above 41 mcg/mL, a concentration 1.4-fold above the intended clinical concentration in the vitreous of 29 mcg/mL. Intraocular hemorrhage was observed in rabbits and monkeys.
- A second intravitreal administration of ocriplasmin (28 days apart) in monkeys at doses of 75 mcg/eye (41 mcg/mL vitreous) or 125 mcg/eye (68 mcg/mL vitreous) was associated with lens subluxation in all ocriplasmin treated eyes. Sustained increases in IOP occurred in two animals with lens subluxation. Microscopic findings in the eye included vitreous liquefaction, degeneration/disruption of the hyaloideocapsular ligament (with loss of ciliary zonular fibers), lens degeneration, mononuclear cell infiltration of the vitreous, and vacuolation of the retinal inner nuclear cell layer. These doses are 1.4-fold and 2.3-fold the intended clinical concentration in the vitreous of 29 mcg/mL, respectively.
Clinical Studies
- The efficacy and safety of JETREA was demonstrated in two multicenter, randomized, double masked, vehicle-controlled, 6 month studies in patients with symptomatic vitreomacular adhesion (VMA). A total of 652 patients (JETREA 464, vehicle 188) were randomized in these 2 studies. Randomization was 2:1 (JETREA:vehicle) in Study 1 and 3:1 in Study 2.
- Patients were treated with a single injection of JETREA or vehicle. In both of the studies, the proportion of patients who achieved VMA resolution at Day 28 (i.e., achieved success on the primary endpoint) was significantly higher in the ocriplasmin group compared with the vehicle group through Month 6 (Table 2 and Figure 7).
How Supplied
- Each vial of JETREA contains 0.5 mg ocriplasmin in 0.2 mL citric-buffered solution (2.5 mg/mL). JETREA is supplied in a 2 mL glass vial with a latex free rubber stopper. Vials are for single use only.
- NDC 24856-001-00
Storage
- Store frozen at or below -4°F (-20°C). Protect the vials from light by storing in the original package until time of use.
Images
Drug Images
{{#ask: Page Name::Ocriplasmin |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
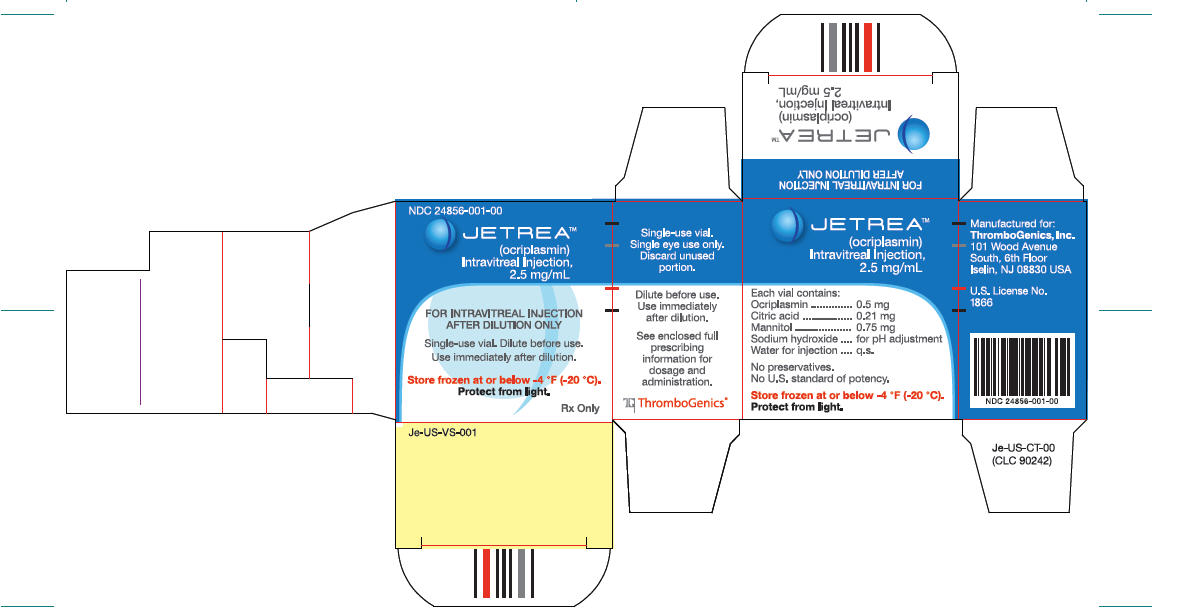
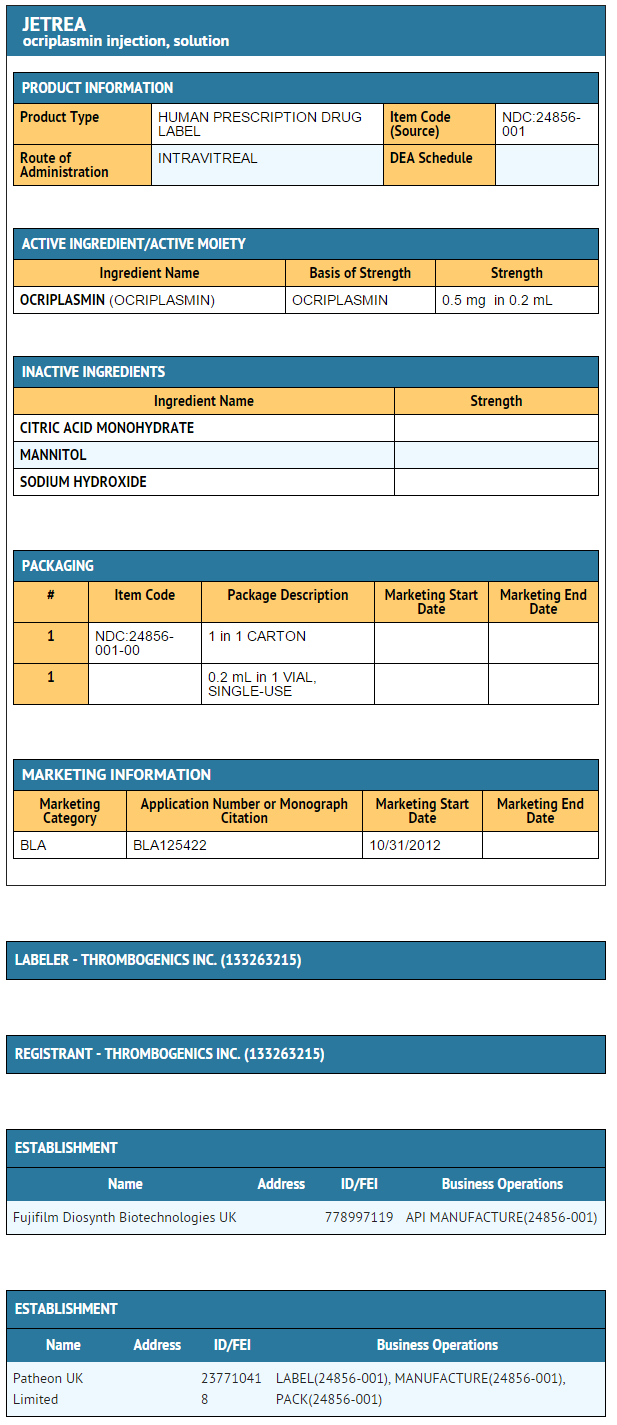
{{#ask: Label Page::Ocriplasmin |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- In the days following JETREA administration, patients are at risk of developing intraocular inflammation/infection. Advise patients to seek immediate care from an ophthalmologist if the eye becomes red, sensitive to light, painful, or develops a change in vision.* Patients may experience temporary visual impairment after receiving an intravitreal injection of JETREA . Advise patients to not drive or operate heavy machinery until this visual impairment has resolved. If visual impairment persists or decreases further, advise patients to seek care from an ophthalmologist.
Precautions with Alcohol
Alcohol-Ocriplasmin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- JETREA®[1]
Look-Alike Drug Names
There is limited information regarding Ocriplasmin Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Ocriplasmin |Label Name=Ocri 04.jpg
}}
{{#subobject:
|Label Page=Ocriplasmin |Label Name=Ocri 05.jpg
}}
{{#subobject:
|Label Page=Ocriplasmin |Label Name=DailyMed - JETREA- ocriplasmin injection, solution .png
}}
- Pages with script errors
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Infobox drug articles without a structure image
- Chemical articles without CAS registry number
- Articles without EBI source
- Articles without KEGG source
- Articles without InChI source
- Articles containing unverified chemical infoboxes
- Infobox drug tracked parameters
- Drug
- Pharmacology