Mitral valve prolapse echocardiography
|
Mitral valve prolapse Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Mitral valve prolapse echocardiography On the Web |
|
American Roentgen Ray Society Images of Mitral valve prolapse echocardiography |
|
Risk calculators and risk factors for Mitral valve prolapse echocardiography |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Two- and three-dimensional echocardiography are valuable in the diagnosis of MVP as they allow visualization of the mitral leaflets relative to the mitral annulus. This allows measurement of the leaflet thickness and their displacement relative to the annulus. Thickening of the mitral leaflets >5 mm and leaflet displacement >2 mm indicates classic mitral valve prolapse.
Echocardiography
2D Echo features
The leaflets and chordae are thick and reduntant. Reduced tensile strength leads to progressive elongation or rupture of chordae. Ruptured chordae appear as flail segments.
To diagnose mitral valve prolapse, the following criteria should be fulfilled - Movement of any part of either leaflet more than 2mm behind the annular plane in parasternal long axis view and movement of point of co-aptation behind the annular plane in apical 4 chamber view. Mitral regurgitation can result in enlarged LA size.
Doppler
Colour flow mapping and CW doppler shows predominantly late systolic mitral regurgitation.
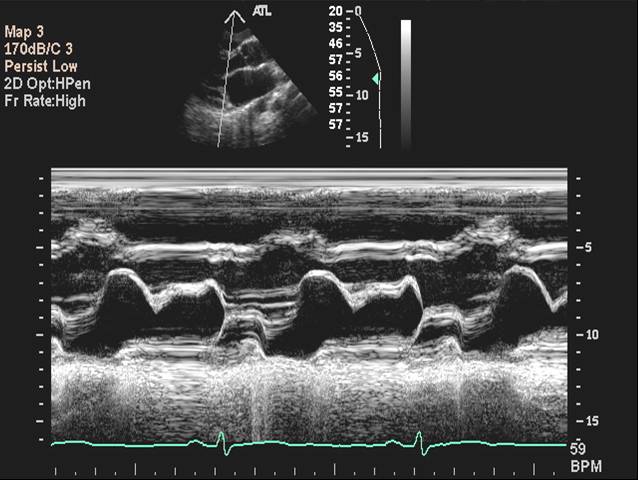
M Mode Echocardiography
 |
2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) [1]
Asymptomatic Patients (DO NOT EDIT) [1]
| Class I |
| "1. Echocardiography is indicated for the diagnosis of MVP and assessment of MR, leaflet morphology, and ventricular compensation in asymptomatic patients with physical signs of MVP. (Level of Evidence: B)" |
| Class III |
| "1. Echocardiography is not indicated to exclude MVP in asymptomatic patients with ill-defined symptoms in the absence of a constellation of clinical symptoms or physical findings suggestive of MVP or a positive family history. (Level of Evidence: B)" |
| "2. Routine repetition of echocardiography is not indicated for the asymptomatic patient who has MVP and no MR or MVP and mild MR with no changes in clinical signs or symptoms. (Level of Evidence: C)" |
| Class IIa |
| "1. Echocardiography can effectively exclude MVP in asymptomatic patients who have been diagnosed without clinical evidence to support the diagnosis. (Level of Evidence: C)" |
| "2. Echocardiography can be effective for risk stratification in asymptomatic patients with physical signs of MVP or known MVP. (Level of Evidence: C)" |
Sources
- 2008 Focused Update Incorporated Into the ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease [1]
References
- ↑ 1.0 1.1 1.2 Bonow RO, Carabello BA, Chatterjee K; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172. Unknown parameter
|month=ignored (help)