Mexiletine
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Gerald Chi
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNINGS
See full prescribing information for complete Boxed Warning.
Mortality:
Acute Liver Injury:
|
Overview
Mexiletine is an antiarrhythmic that is FDA approved for the {{{indicationType}}} of ventricular arrhythmias, such as sustained ventricular tachycardia. There is a Black Box Warning for this drug as shown here. Common adverse reactions include heartburn, nausea, vomiting, coordination problem, dizziness, lightheadedness, tremor, blurred vision, visual disturbance, and anxiety.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- Loading Dose
- When rapid control of ventricular arrhythmia is essential, an initial loading dose of 400 mg of mexiletine hydrochloride may be administered, followed by a 200 mg dose in eight hours. Onset of therapeutic effect is usually observed within 30 minutes to two hours.
- Q12H Dosage Schedule
- Some patients responding to mexiletine may be transferred to a 12 hour dosage schedule to improve convenience and compliance. If adequate suppression is achieved on a mexiletine hydrochloride dose of 300 mg or less every eight hours, the same total daily dose may be given in divided doses every 12 hours while carefully monitoring the degree of suppression of ventricular ectopy. This dose may be adjusted up to a maximum of 450 mg every 12 hours to achieve the desired response.
- Transferring to Mexiletine Hydrochloride
- The following dosage schedule, based on theoretical considerations rather than experimental data, is suggested for transferring patients from other Class I oral antiarrhythmic agents to mexiletine: mexiletine hydrochloride treatment may be initiated with a 200 mg dose, and titrated to response as described above, 6 to 12 hours after the last dose of quinidine sulfate, 3 to 6 hours after the last dose of procainamide, 6 to 12 hours after the last dose of disopryramide or 8 to 12 hours after the last dose of tocainide.
- In patients in whom withdrawal of the previous antiarrhythmic agent is likely to produce life-threatening arrhythmias, hospitalization of the patient is recommended.
- When transferring from lidocaine to mexiletine, the lidocaine infusion should be stopped when the first oral dose of mexiletine hydrochloride is administered. The infusion line should be left open until suppression of the arrhythmia appears to be satisfactorily maintained. Consideration should be given to the similarity of the adverse effects of lidocaine and mexiletine and the possibility that they may be additive.
Ventricular Arrhythmia
- Dosing Information
- The dosage of mexiletine hydrochloride must be individualized on the basis of response and tolerance, both of which are dose-related. Administration with food or antacid is recommended. Initiate mexiletine therapy with 200 mg every eight hours when rapid control of arrhythmia is not essential. A minimum of two to three days between dose adjustments is recommended. Dose may be adjusted in 50 or 100 mg increments up or down.
- As with any antiarrhythmic drug, clinical and electrocardiographic evaluation (including Holter monitoring if necessary for evaluation) are needed to determine whether the desired antiarrhythmic effect has been obtained and to guide titration and dose adjustment.
- Satisfactory control can be achieved in most patients by 200 to 300 mg given every eight hours with food or antacid. If satisfactory response has not been achieved at 300 mg q8h, and the patient tolerates mexiletine well, a dose of 400 mg q8h may be tried. As the severity of CNS side effects increases with total daily dose, the dose should not exceed 1200 mg/day.
- In general, patients with renal failure will require the usual doses of mexiletine hydrochloride. Patients with severe liver disease, however, may require lower doses and must be monitored closely. Similarly, marked right-sided congestive heart failure can reduce hepatic metabolism and reduce the needed dose. Plasma level may also be affected by certain concomitant drugs
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Mexiletine in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Mexiletine in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
- Safety and effectiveness in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Mexiletine in pediatric patients.
Non–Guideline-Supported Use
Premature Ventricular Contractions, Ventricular Couplets, or Ventricular Tachycardia Associated with Congenital Heart Disease
- Dosing Information
- 1.4 to 5 mg/kg (mean 3.3 mg/kg) every 8 hours[1]
Contraindications
- Mexiletine hydrochloride capsules are contraindicated in the presence of cardiogenic shock or pre-existing second-or third-degree AV block (if no pacemaker is present).
Warnings
|
WARNINGS
See full prescribing information for complete Boxed Warning.
Mortality:
Acute Liver Injury:
|
Precautions
- General
- If a ventricular pacemaker is operative, patients with second or third degree heart block may be treated with mexiletine hydrochloride if continuously monitored. A limited number of patients (45 of 475 in controlled clinical trials) with pre-existing first degree AV block were treated with mexiletine; none of these patients developed second or third degree AV block. Caution should be exercised when it is used in such patients or in patients with pre-existing sinus node dysfunction or intraventricular conduction abnormalities.
- Like other antiarrhythmics mexiletine hydrochloride can cause worsening of arrhythmias. This has been uncommon in patients with less serious arrhythmias (frequent premature beats or nonsustained ventricular tachycardia: see ADVERSE REACTIONS), but is of greater concern in patients with life-threatening arrhythmias such as sustained ventricular tachycardia. In patients with such arrhythmias subjected to programmed electrical stimulation or to exercise provocation, 10 to 15% of patients had exacerbation of the arrhythmia, a rate not greater than that of other agents.
- Mexiletine should be used with caution in patients with hypotension and severe congestive heart failure because of the potential for aggravating these conditions.
- Since mexiletine is metabolized in the liver, and hepatic impairment has been reported to prolong the elimination half-life of mexiletine, patients with liver disease should be followed carefully while receiving mexiletine. The same caution should be observed in patients with hepatic dysfunction secondary to congestive heart failure.
- Concurrent drug therapy or dietary regimens which may markedly alter urinary pH should be avoided during mexiletine hydrochloride therapy. The minor fluctuations in urinary pH associated with normal diet do not affect the excretion of mexiletine.
- SGOT Elevation and Liver Injury
- In three month controlled trials, elevations of SGOT greater than three times the upper limit of normal occurred in about 1% of both mexiletine-treated and control patients. Approximately 2% of patients in the mexiletine compassionate use program had elevations of SGOT greater than or equal to three times the upper limit of normal. These elevations frequently occurred in association with identifiable clinical events and therapeutic measures such as congestive heart failure, acute myocardial infarction, blood transfusions and other medications. These elevations were often asymptomatic and transient, usually not associated with elevated bilirubin levels and usually did not require discontinuation of therapy. Marked elevations of SGOT (> 1000 U/L) were seen before death in four patients with end-stage cardiac disease (severe congestive heart failure, cardiogenic shock).
- Rare instances of severe liver injury, including hepatic necrosis, have been reported in association with mexiletine treatment. It is recommended that patients in whom an abnormal liver test has occurred, or who have signs of symptoms suggesting liver dysfunction, be carefully evaluated. If persistent or worsening elevation of hepatic enzymes is detected, consideration should be given to discontinuing therapy.
- Blood Dyscrasias
- Among 10,867 patients treated with mexiletine in the compassionate use program, marked leukopenia (neutrophils less than 1000/mm3) or agranulocytosis were seen in 0.06% and milder depressions of leukocytes were seen in 0.08%, and thrombocytopenia was observed in 0.16%. Many of these patients were seriously ill and receiving concomitant medications with known hematologic adverse effects. Rechallenge with mexiletine in several cases was negative. Marked leukopenia or agranulocytosis did not occur in any patient receiving mexiletine alone; five of the six cases of agranulocytosis were associated with procainamide (sustained release preparations in four) and one with vinblastine. If significant hematologic changes are observed, the patient should be carefully evaluated, and, if warranted, mexiletine should be discontinued. Blood counts usually return to normal within a month of discontinuation (see ADVERSE REACTIONS).
- Convulsions (seizures) did not occur in mexiletine controlled clinical trials. In the compassionate use program, convulsions were reported in about 2 of 1000 patients. Twenty-eight percent of these patients discontinued therapy. Convulsions were reported in patients with and without a prior history of seizures. Mexiletine should be used with caution in patients with known seizure disorder.
Adverse Reactions
Clinical Trials Experience
- Mexiletine hydrochloride commonly produces reversible gastrointestinal and nervous system adverse reactions but is otherwise well tolerated. Mexiletine has been evaluated in 483 patients in one month and three month controlled studies and in over 10,000 patients in a large compassionate use program. Dosages in the controlled studies ranged from 600 to 1200 mg/day; some patients (8%) in the compassionate use program were treated with higher daily doses (1600 to 3200 mg/day). In the three month controlled trials comparing mexiletine to quinidine, procainamide and disopyramide, the most frequent adverse reactions were upper gastrointestinal distress (41%), lightheadedness (10.5%), tremor (12.6%) and coordination difficulties (10.2%). Similar frequency and incidence were observed in the one month placebo-controlled trial. Although these reactions were generally not serious, and were dose-related and reversible with a reduction in dosage, by taking the drug with food or antacid or by therapy discontinuation, they led to therapy discontinuation in 40% of patients in the controlled trials. Table 1 presents the adverse events reported in the one-month placebo-controlled trial.
- Table 2 presents the adverse reactions occurring in one percent or more of patients in the three month controlled studies.
- Less than 1%: Syncope, edema, hot flashes, hypertension, short-term memory loss, loss of consciousness, other psychological changes, diaphoresis, urinary hesitancy/retention, malaise, impotence/decreased libido, pharyngitis, congestive heart failure.
- An additional group of over 10,000 patients has been treated in a program allowing administration of mexiletine hydrochloride under compassionate use circumstances. These patients were seriously ill with the large majority on multiple drug therapy. Twenty-four percent of the patients continued in the program for one year or longer. Adverse reactions leading to therapy discontinuation occurred in 15 percent of patients (usually upper gastrointestinal system or nervous system effects). In general, the more common adverse reactions were similar to those in the controlled trials. Less common adverse events possibly related to mexiletine use include:
Cardiovascular
Syncope and hypotension, each about 6 in 1000; bradycardia, about 4 in 1000; angina/angina-like pain, about 3 in 1000; edema, atrioventricular block/conduction disturbances and hot flashes, each about 2 in 1000; atrial arrhythmias, hypertension and cardiogenic shock, each about 1 in 1000.
Digestive
Dysphagia, about 2 in 1000; peptic ulcer, about 8 in 10,000; upper gastrointestinal bleeding, about 7 in 10,000; esophageal ulceration, about 1 in 10,000. Rare cases of severe hepatitis/acute hepatic necrosis.
Hematologic and Lymphatic
Blood dyscrasias were not seen in the controlled trials but did occur among 10,867 patients treated with mexiletine in the compassionate use program.
Myelofibrosis was reported in two patients in the compassionate use program; one was receiving long-term thiotepa therapy and the other had pretreatment myeloid abnormalities.
In postmarketing experience, there have been isolated, spontaneous reports of pulmonary changes including pulmonary infiltration and pulmonary fibrosis during mexiletine therapy with or without other drugs or diseases that are known to produce pulmonary toxicity. A causal relationship to mexiletine therapy has not been established. In addition, there have been isolated reports of drowsiness, nystagmus, ataxia, dyspepsia, hypersensitivity reaction, and exacerbation of congestive heart failure in patients with pre-existing compromised ventricular function. There have been rare reports of pancreatitis associated with mexiletine treatment.
Neurologic
Short-term memory loss, about 9 in 1000 patients; hallucinations and other psychological changes, each about 3 in 1000; psychosis and convulsions/seizures, each about 2 in 1000; loss of consciousness, about 6 in 10,000.
Skin and Hypersensitivy Reactions
Rare cases of exfoliative dermatitis and Stevens-Johnson syndrome with mexiletine treatment have been reported.
Laboratory
Abnormal liver function tests, about 5 in 1000; positive ANA and thrombocytopenia, each about 2 in 1000; leukopenia (including neutropenia and agranulocytosis), about 1 in 1000; myelofibrosis, about 2 in 10,000 patients.
Miscellaneous
Diaphoresis, about 6 in 1000; altered taste, about 5 in 1000; salivary changes, hair loss and impotence/decreased libido, each about 4 in 1000; malaise, about 3 in 1000; urinary hesitancy/retention, each about 2 in 1000; hiccups, dry skin, laryngeal and pharyngeal changes and changes in oral mucous membranes, each about 1 in 1000; SLE syndrome, about 4 in 10,000.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Mexiletine in the drug label.
Drug Interactions
- Drug
- Description
Use in Specific Populations
Pregnancy
- Pregnancy Category
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Mexiletine in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Mexiletine during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Mexiletine with respect to nursing mothers.
Pediatric Use
There is no FDA guidance on the use of Mexiletine with respect to pediatric patients.
Geriatic Use
There is no FDA guidance on the use of Mexiletine with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Mexiletine with respect to specific gender populations.
Race
There is no FDA guidance on the use of Mexiletine with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Mexiletine in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Mexiletine in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Mexiletine in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Mexiletine in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
- Intravenous
Monitoring
There is limited information regarding Monitoring of Mexiletine in the drug label.
Condition1
- Description
IV Compatibility
There is limited information regarding IV Compatibility of Mexiletine in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- Clinical findings associated with mexiletine overdosage have included drowsiness, confusion, nausea, hypotension, sinus bradycardia, paresthesia, seizures, bundle branch block, AV heart block, asystole, ventricular tachyarrythmia, including ventricular fibrillation, cardiovascular collapse and coma. The lowest known dose in a fatality case was 4.4 g with postmortem serum mexiletine level of 34 to 37 mcg/mL (Jequier P. et. al., Lancet 1976: 1 (7956): 429). Patients have recovered from ingestion of 4 g to 18 g of mexiletine (Frank S. E. et. al., Am J Emerg Med 1991: 9:43-48).
Management
- In postmarketing experience, there have been isolated, spontaneous reports of pulmonary changes including pulmonary infiltration and pulmonary fibrosis during mexiletine therapy with or without other drugs or diseases that are known to produce pulmonary toxicity. A causal relationship to mexiletine therapy has not been established. In addition, there have been isolated reports of drowsiness, nystagmus, ataxia, dyspepsia, hypersensitivity reaction, and exacerbation of congestive heart failure in patients with pre-existing compromised ventricular function. There have been rare reports of pancreatitis associated with mexiletine treatment.
Chronic Overdose
There is limited information regarding Chronic Overdose of Mexiletine in the drug label.
Pharmacology
| |
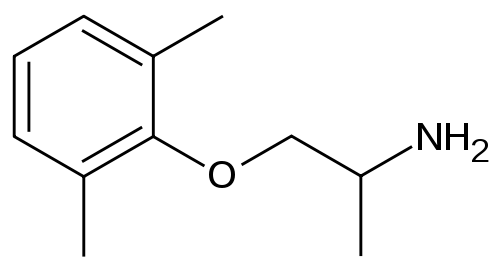
1 : 1 mixture (racemate)Mexiletine
| |
| Systematic (IUPAC) name | |
| (RS)-1-(2,6-dimethylphenoxy)propan-2-amine OR 2-(2-aminopropoxy)-1,3-dimethylbenzene | |
| Identifiers | |
| CAS number | |
| ATC code | C01 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 179.259 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | 90% |
| Protein binding | 50-60% |
| Metabolism | Hepatic (CYP2D6 and 1A2- mediated) |
| Half life | 10-12 hours |
| Excretion | Renal (10%) |
| Therapeutic considerations | |
| Pregnancy cat. | |
| Legal status | |
| Routes | Oral, IV |
Mechanism of Action
Structure
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Mexiletine in the drug label.
Pharmacokinetics
There is limited information regarding Pharmacokinetics of Mexiletine in the drug label.
Nonclinical Toxicology
There is limited information regarding Nonclinical Toxicology of Mexiletine in the drug label.
Clinical Studies
There is limited information regarding Clinical Studies of Mexiletine in the drug label.
Condition1
- Description
How Supplied
Storage
There is limited information regarding Mexiletine Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Mexiletine |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Mexiletine |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Mexiletine in the drug label.
Precautions with Alcohol
- Alcohol-Mexiletine interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Mexitil®[2]
Look-Alike Drug Names
- A® — B®[3]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Moak, J. P. (1987-10). "Mexiletine: an effective antiarrhythmic drug for treatment of ventricular arrhythmias in congenital heart disease". Journal of the American College of Cardiology. 10 (4): 824–829. ISSN 0735-1097. PMID 3655149. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ "MEXILETINE HYDROCHLORIDE (mexiletine hydrochloride) capsule".
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Mexiletine |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Mexiletine |Label Name=Mexiletine11.png
}}
{{#subobject:
|Label Page=Mexiletine |Label Name=Mexiletine11.png
}}


