Medullary thyroid cancer staging: Difference between revisions
No edit summary |
|||
| Line 185: | Line 185: | ||
===Medullary Thyroid Cancer=== | ===Medullary Thyroid Cancer=== | ||
====Stage | * Several staging systems have been employed to correlate extent of disease with long-term survival in medullary thyroid cancer. The clinical staging system of the AJCC correlates survival to size of the primary tumor, presence or absence of lymph node metastases, and presence or absence of distance metastasis. Patients with the best prognosis are those who are diagnosed by provocative screening, prior to the appearance of palpable disease.[3] | ||
* Stage I | ====Stage 0 medullary thyroid cancer==== | ||
====Stage II | * Clinically occult disease detected by provocative biochemical screening. | ||
* | ====Stage I medullary thyroid cancer==== | ||
====Stage III | * Tumor smaller than 2 cm. | ||
* | ====Stage II medullary thyroid cancer==== | ||
====Stage IV | * Tumor larger than 2 cm but 4 cm or smaller with no metastases or larger than 4 cm with minimal extrathyroid extension. | ||
* Stage IV is | ====Stage III medullary thyroid cancer==== | ||
* Tumor of any size with metastases limited to the pretracheal, paratracheal, or prelaryngeal/Delphian lymph nodes. | |||
====Stage IV medullary thyroid cancer==== | |||
* Stage IV medullary thyroid cancer is divided into the following categories: | |||
:* Stage IVA (moderately advanced with or without lymph node metastases [for T4a] but without distant metastases). | |||
:* Stage IVB (very advanced with or without lymph node metastases but no distant metastases). | |||
:* Stage IVC (distant metastases). | |||
* Medullary carcinoma usually presents as a hard mass and is often accompanied by blood vessel invasion. Medullary thyroid cancer occurs in two forms, sporadic and familial. In the sporadic form, the tumor is usually unilateral. In the familial form, the tumor is almost always bilateral. In addition, the familial form may be associated with benign or malignant tumors of other endocrine organs, commonly referred to as the multiple endocrine neoplasia syndromes (MEN 2A or MEN 2B). | |||
* In these syndromes, there is an association with pheochromocytoma of the adrenal gland and parathyroid hyperplasia. Medullary carcinoma usually secretes calcitonin, a hormonal marker for the tumor, and may be detectable in blood even when the tumor is clinically occult. Metastases to regional lymph nodes are found in about 50% of cases. Prognosis depends on extent of disease at presentation, presence or absence of regional lymph node metastases, and completeness of the surgical resection.[4] | |||
* Family members should be screened for calcitonin elevation to identify individuals who are at risk of developing familial medullary thyroid cancer. MEN 2A gene carrier status can be more accurately determined by analysis of mutations in the RET gene. Whereas modest el mutation is the optimal approach in evaluating MEN 2A. All patients with medullary carcinoma of the thyroid (whether familial or sporadic) should be tested for RET mutations, and, if they are positive, family members should also be tested. Family members who are gene carriers should undergo prophylactic thyroidectomy at an early age.[5-7] | |||
<gallery> | <gallery> | ||
File:Stage M1 Thyroid cancer.png|Stage M1 thyroid cancer | File:Stage M1 Thyroid cancer.png|Stage M1 thyroid cancer | ||
| Line 203: | Line 213: | ||
File:Diagram showing stage T4b thyroid cancer CRUK 273.png|Stage T4b thyroid cancer | File:Diagram showing stage T4b thyroid cancer CRUK 273.png|Stage T4b thyroid cancer | ||
</gallery> | </gallery> | ||
==Reference== | |||
{{Reflist|2}} | |||
==Reference== | ==Reference== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
Revision as of 15:27, 11 November 2015
|
Medullary thyroid cancer Microchapters |
|
Differentiating Medullary thyroid cancer from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Medullary thyroid cancer staging On the Web |
|
American Roentgen Ray Society Images of Medullary thyroid cancer staging |
|
Risk calculators and risk factors for Medullary thyroid cancer staging |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Overview
According to the American Joint Committee on Cancer (AJCC)[1] there are 4 stages of medullary thyroid cancer based on the clinical features and findings on imaging. Each stage is assigned a letter and a number that designate the tumor size, number of involved lymph node regions, and metastasis.
Staging
| Stage | Description |
|---|---|
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
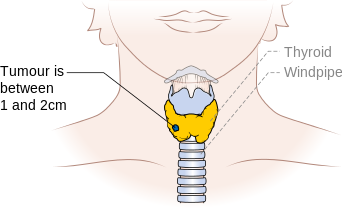
| T1 | Tumor ≤2 cm in greatest dimension limited to the thyroid |
| T1a | Tumor ≤1 cm, limited to the thyroid |
| T1b | Tumor >1 cm but ≤2 cm in greatest dimension, limited to the thyroid |
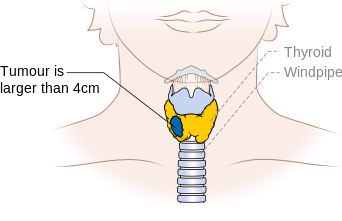
| T2 | Tumor >2 cm but ≤4 cm in greatest dimension, limited to the thyroid |
| T3 | Tumor >4 cm in greatest dimension limited to the thyroid or any tumor with minimal extrathyroid extension (e.g., extension to sternothyroid muscle or perithyroid soft tissues) |
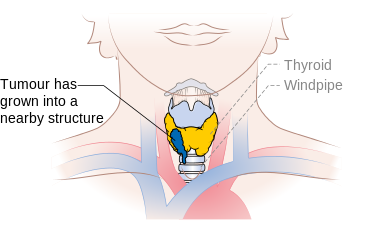
| T4a | Moderately advanced disease |
| Tumor of any size extending beyond the thyroid capsule to invade subcutaneous soft tissues, larynx, trachea, esophagus, or recurrent laryngeal nerve | |
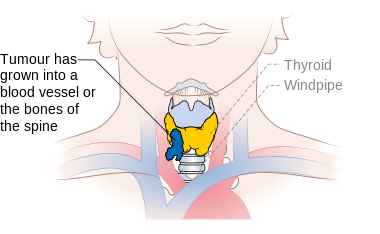
| T4b | Very advanced disease |
| Tumor invades prevertebral fascia or encases carotid artery or mediastinal vessel |
| Stage | Description |
|---|---|
| NX | Regional lymph node cannot be assessed |
| N0 | No regional lymph node metastasis]] |
| N1 | Regional lymph node metastasis |
| N1a | Metastases to Level VI (pretracheal, paratracheal, and prelaryngeal/Delphian lymph nodes) |
| N1b | Metastases to unilateral, bilateral, or contralateral cervical (Levels I, II, III, IV, or V) or retropharyngeal or superior mediastinal lymph nodes (Level VII) |
| Stage | Description |
|---|---|
| M0 | No distant metastasis |
| M1 | Distant metastasis |
| Stage | T | N | M |
|---|---|---|---|
| Medullary carcinoma (all age groups) | |||
| I | T1 | N0 | M0 |
| II | T2 | N0 | M0 |
| T3 | N0 | M0 | |
| III | T1 | N1a | M0 |
| T2 | N1a | M0 | |
| T3 | N1a | M0 | |
| IVa | T4a | N0 | M0 |
| T4a | N1a | M0 | |
| T1 | N1b | M0 | |
| T2 | N1b | M0 | |
| T3 | N1b | M0 | |
| T4a | N1b | M0 | |
| Stage IVb | T4b | Any N | |
| IVB | T4b | Any N | M0 |
| IVC | Any T | Any N | M1 |
Medullary Thyroid Cancer
- Several staging systems have been employed to correlate extent of disease with long-term survival in medullary thyroid cancer. The clinical staging system of the AJCC correlates survival to size of the primary tumor, presence or absence of lymph node metastases, and presence or absence of distance metastasis. Patients with the best prognosis are those who are diagnosed by provocative screening, prior to the appearance of palpable disease.[3]
Stage 0 medullary thyroid cancer
- Clinically occult disease detected by provocative biochemical screening.
Stage I medullary thyroid cancer
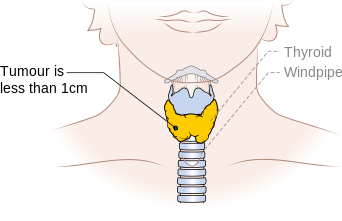
- Tumor smaller than 2 cm.
Stage II medullary thyroid cancer
- Tumor larger than 2 cm but 4 cm or smaller with no metastases or larger than 4 cm with minimal extrathyroid extension.
Stage III medullary thyroid cancer
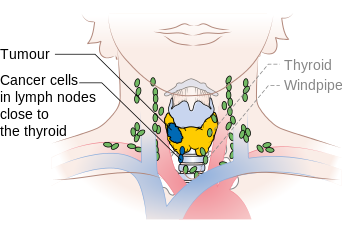
- Tumor of any size with metastases limited to the pretracheal, paratracheal, or prelaryngeal/Delphian lymph nodes.
Stage IV medullary thyroid cancer
- Stage IV medullary thyroid cancer is divided into the following categories:
- Stage IVA (moderately advanced with or without lymph node metastases [for T4a] but without distant metastases).
- Stage IVB (very advanced with or without lymph node metastases but no distant metastases).
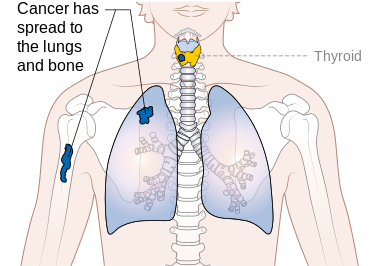
- Stage IVC (distant metastases).
- Medullary carcinoma usually presents as a hard mass and is often accompanied by blood vessel invasion. Medullary thyroid cancer occurs in two forms, sporadic and familial. In the sporadic form, the tumor is usually unilateral. In the familial form, the tumor is almost always bilateral. In addition, the familial form may be associated with benign or malignant tumors of other endocrine organs, commonly referred to as the multiple endocrine neoplasia syndromes (MEN 2A or MEN 2B).
- In these syndromes, there is an association with pheochromocytoma of the adrenal gland and parathyroid hyperplasia. Medullary carcinoma usually secretes calcitonin, a hormonal marker for the tumor, and may be detectable in blood even when the tumor is clinically occult. Metastases to regional lymph nodes are found in about 50% of cases. Prognosis depends on extent of disease at presentation, presence or absence of regional lymph node metastases, and completeness of the surgical resection.[4]
- Family members should be screened for calcitonin elevation to identify individuals who are at risk of developing familial medullary thyroid cancer. MEN 2A gene carrier status can be more accurately determined by analysis of mutations in the RET gene. Whereas modest el mutation is the optimal approach in evaluating MEN 2A. All patients with medullary carcinoma of the thyroid (whether familial or sporadic) should be tested for RET mutations, and, if they are positive, family members should also be tested. Family members who are gene carriers should undergo prophylactic thyroidectomy at an early age.[5-7]
-
Stage M1 thyroid cancer
-
Stage N1a thyroid cancer
-
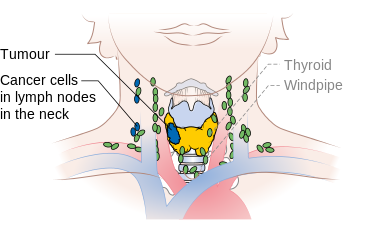
Stage N1b thyroid cancer
-
Stage T1a thyroid cancer
-
Stage T1b thyroid cancer
-
Stage T3 thyroid cancer
-
Stage T4a thyroid cancer
-
Stage T4b thyroid cancer
Reference
- ↑ Stage Information for Thyroid Cancer Cancer.gov (2015). http://www.cancer.gov/types/thyroid/hp/thyroid-treatment-pdq#link/stoc_h2_2- Accessed on October, 29 2015