Hemolytic anemia laboratory findings
|
Hemolytic anemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hemolytic anemia laboratory findings On the Web |
|
American Roentgen Ray Society Images of Hemolytic anemia laboratory findings |
|
Risk calculators and risk factors for Hemolytic anemia laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Shyam Patel [2]
Overview
Laboratory evaluation begins with examination of the peripheral blood smear. Serum tests include LDH, haptoglobin, bilirubin, and reticulocyte count. A combination of all of these tests can give insight into whether or note hemolytic anemia is present and, if present, the degree of hemolysis. The osmotic fragility test is less commonly used but can also be used to assess for predisposition to hemolysis.
Approach to diagnosis of hemolytic anemia
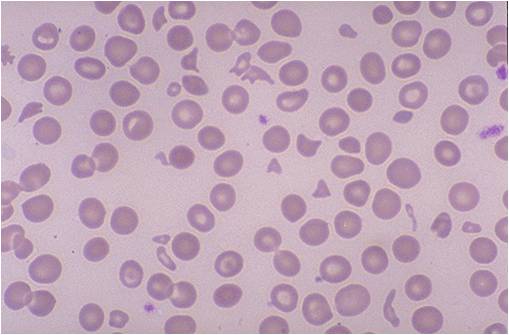
The most important initial diagnostic tests is the peripheral blood smear. This allows for direct visualization of the red blood cells and any other morphologic abnormalities. The results of the peripheral blood smear can frequently guide additional testing.[1] The cost of a peripheral blood smear is low, and thus it is the test of choice for initial workup of hemolytic anemia. A peripheral blood smear is prepared by placing a small about of whole blood onto a glass slide, then using a second glass slide to smear the blood on the first slide. Stains are done to help visualize cells.
Peripheral blood smear
- Schistocytes: These are fragments of red blood cells. They are also known as helmet cells. Presence of schistocytes is not specific for hemolysis but is specific for a microangiopathic process, which can be associated with hemolysis.
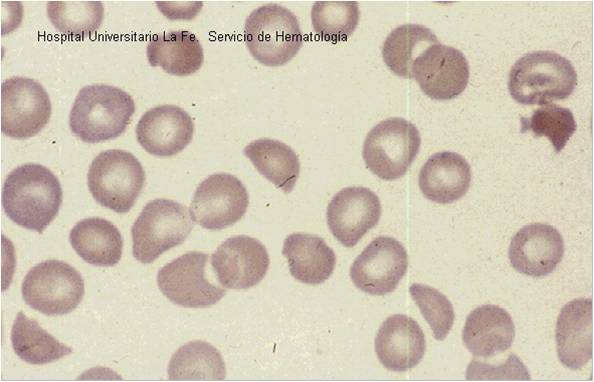
- Spherocytes: These are red blood cells that contain a high volume to surface area ratio. These cells have a relative lack of membrane and thus appear as spheres rather than the typical biconcave shape of normal red blood cells. They appear smaller and rounder than normal red blood cells.
- Bite cells: These are also known as Heinz bodies. They are typically seen in patients with hemolysis from G6PD deficiency. Heinz bodies comprise denatured hemoglobin.
- Target cells: These are also known as codocytes. They are not specific for hemolysis, as they can be found in liver disease, thalassemia, hemoglobin E, and hemoglobin C. Electrophoresis helps to differentiate between thalassemia and liver diseases (elevated liver enzymes), and other hemoglobinopathies.
- Reticulocytes: These are primitive or immature red blood cells. They contain residual ribosomes and RNA. The presence of RNA allows a visible blue stain to bind or, in the case of fluorescent dye, result in a different brightness. This is known as polychromasia.[1] When reticulocytes are present in elevated numbers, this suggests an adequate bone marrow response to anemia. The reticulocytes response act as an important indicator for the severity of the hemolytic anemia. The normal reticulocyte count is 0.5-1.5%. In the case of hemolysis, the reticulocyte count can increase to beyond 10%. The different methods used to assess the appropriate response are:
- Absolute reticulocyte count: This is measured in number of cells per microliter. The normal range for absolute reticulocyte count is 25,000 to 75,000 per microliter.
- Corrected reticulocyte count: This is calculated as absolute reticulocyte count divided by reticulocyte maturation time (in days).
- Reticulocyte production index: This is calculated as reticulocytes % x (hematocrit / 45) x (1 / reticulocyte maturation time). The reticulocyte index (RI) should be between 1.0 and 2.0 for a healthy patient.
- RI < 2 with anemia indicates decreased production of reticulocytes and therefore red blood cells.
- RI > 2 with anemia indicates loss of red blood cells (destruction, bleeding, etc) leading to increased compensatory production of reticulocytes to replace the lost red blood cells.
Laboratory Findings
- Elevated total bilirubin: Elevated bilirubin, or hyperbilirubinemia, is a hallmark of hemolytic anemia. Bilirubin is typically unconjugated (indirect).
- Elevated LDH: This is an enzyme present in red blood cells. When hemolysis occurs, the intracellular contents of the cells are released, and LDH levels rise.
- Low haptoglobin: Haptoglobin is produced in the liver and bind free hemoglobin. During hemolysis, haptoglobin decreases as it is consumed at a faster rate compared to the rate of production by the liver.
- Elevated reticulocyte count: Reticulocytes are primitive red blood cells and are elevated in hemolysis. Please see above for detailed explanation of reticulocytosis.
- Direct antiglobulin test (DAT) (Coomb's test)[1]: This measures the presence of antibodies on patient's red blood cells. This is an important diagnostic test to help differentiate immune-mediated hemolysis from non-immune-mediated hemolysis. A positive Coomb's test suggests immune-mediated hemolysis. The DAT can detect either IgG or complement protein C3 on the surface of red blood cells. Presence of IgG (or IgG plus C3) is characteristic of warm autoimmune hemolytic anemia, whereas presence of C3 is more characteristic of cold agglutinin disease or paroxysmal cold hemoglobinuria.[1]
- Indirect antiglobulin test (indirect Coombs' test)[1]: This measures the presence of antibodies in a patient's serum but not coating their red cells. This is another test that helps differentiate immune-mediated hemolysis from non-immune-mediated hemolysis. A positive indirect Coomb's test can suggest alloantibodies from prior transfusion.
- Osmotic fragility test: This test determines the fragility of red blood cells to hypotonic lysis. Patients with hereditary spherocytosis usually have red blood cells with high degrees of osmotic fragility.[2]
Specific findings for intravascular hemolysis
- Elevated urine hemosiderin
- Elevated urine hemoglobin
- Microangiopathic blood smear
Specific findings for extravascular hemolysis
- Spherocytic red cell morphology
- Negative urine hemosiderin
- Negative urine hemoglobin
(Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey, and Hospital Universitario La Fe Servicio Hematologia)
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Packman CH (2015). "The Clinical Pictures of Autoimmune Hemolytic Anemia". Transfus Med Hemother. 42 (5): 317–24. doi:10.1159/000440656. PMC 4678314. PMID 26696800.
- ↑ Jung HL (2013). "A new paradigm in the diagnosis of hereditary hemolytic anemia". Blood Res. 48 (4): 237–9. doi:10.5045/br.2013.48.4.237. PMC 3894378. PMID 24466544.