Heart murmur pathophysiology
|
Heart murmur Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Heart murmur pathophysiology On the Web |
|
American Roentgen Ray Society Images of Heart murmur pathophysiology |
|
Risk calculators and risk factors for Heart murmur pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Associate Editor(s)-in-Chief: Nuha Al-Howthi, MD[2]
Overview
Turbulent flow is responsible for most murmurs. Turbulent flow occurs when the velocity of blood flow becomes critically high because of a high volume of flow, the flow goes through an irregular or narrow area, the flow empties into a dilated vessel or chamber, or if the flow goes backward through an incompetent valve, septal defect, or patent ductus arteriosus. Frequently, a combination of these factors is operative. The sounds most commonly originate from the abnormal movement of blood across valves and between cardiac chambers. When this occurs, turbulence results, which produces vibrations in the chambers of the heart or outflow vessels that are detected as Murmurs.
summery of pathophysiology
| pathophysiology | |
|---|---|
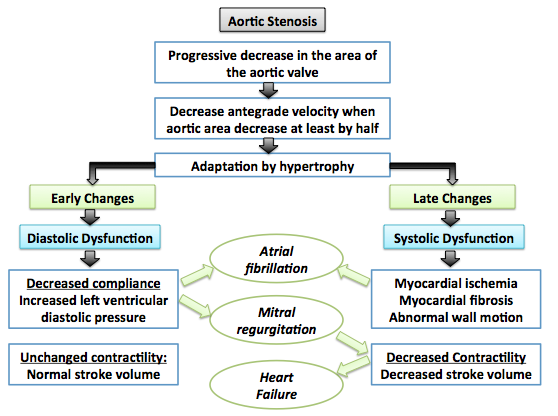
| aortic stenosis |
 |
| aortic regurgitation |
|
| mitral stenosis |
|
| mitral regurgitation |
|
References
- ↑ Galli D, Manuguerra R, Monaco R, Manotti L, Goldoni M, Becchi G; et al. (2016). "Understanding the structural features of symptomatic calcific aortic valve stenosis: A broad-spectrum clinicopathologic study in 236 consecutive surgical cases". Int J Cardiol. 228: 364–374. doi:10.1016/j.ijcard.2016.11.180. PMID 27866029.
- ↑ Joseph J, Naqvi SY, Giri J, Goldberg S (2016). "Aortic stenosis: pathophysiology, diagnosis and therapy". Am J Med. doi:10.1016/j.amjmed.2016.10.005. PMID 27810479.
- ↑ Otto CM, Prendergast B (2014). "Aortic-valve stenosis--from patients at risk to severe valve obstruction". N Engl J Med. 371 (8): 744–56. doi:10.1056/NEJMra1313875. PMID 25140960.
- ↑ 4.0 4.1 Dweck MR, Boon NA, Newby DE (2012). "Calcific aortic stenosis: a disease of the valve and the myocardium". J Am Coll Cardiol. 60 (19): 1854–63. doi:10.1016/j.jacc.2012.02.093. PMID 23062541.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". J Thorac Cardiovasc Surg. 148 (1): e1–e132. doi:10.1016/j.jtcvs.2014.05.014. PMID 24939033.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". J Am Coll Cardiol. 63 (22): e57–185. doi:10.1016/j.jacc.2014.02.536. PMID 24603191.
- ↑ Stout KK, Verrier ED (2009). "Acute valvular regurgitation". Circulation. 119 (25): 3232–41. doi:10.1161/CIRCULATIONAHA.108.782292. PMID 19564568.
- ↑ Mokadam NA, Stout KK, Verrier ED (2011). "Management of acute regurgitation in left-sided cardiac valves". Tex Heart Inst J. 38 (1): 9–19. PMC 3060740. PMID 21423463.
- ↑ Enriquez-Sarano M, Tajik AJ (2004). "Clinical practice. Aortic regurgitation". N Engl J Med. 351 (15): 1539–46. doi:10.1056/NEJMcp030912. PMID 15470217.
- ↑ Devlin WH, Petrusha J, Briesmiester K, Montgomery D, Starling MR (1999). "Impact of vascular adaptation to chronic aortic regurgitation on left ventricular performance". Circulation. 99 (8): 1027–33. PMID 10051296.
- ↑ Nishimura, RA. (2002). "Cardiology patient pages. Aortic valve disease". Circulation. 106 (7): 770–2. PMID 12176943. Unknown parameter
|month=ignored (help) - ↑ BLAND EF, DUCKETT JONES T (1951). "Rheumatic fever and rheumatic heart disease; a twenty year report on 1000 patients followed since childhood". Circulation. 4 (6): 836–43. PMID 14879491.
- ↑ Gordon SP, Douglas PS, Come PC, Manning WJ (1992). "Two-dimensional and Doppler echocardiographic determinants of the natural history of mitral valve narrowing in patients with rheumatic mitral stenosis: implications for follow-up". J Am Coll Cardiol. 19 (5): 968–73. PMID 1552121.
- ↑ Sagie A, Freitas N, Padial LR, Leavitt M, Morris E, Weyman AE; et al. (1996). "Doppler echocardiographic assessment of long-term progression of mitral stenosis in 103 patients: valve area and right heart disease". J Am Coll Cardiol. 28 (2): 472–9. doi:10.1016/0735-1097(96)00153-2. PMID 8800128.
- ↑ Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016
- ↑ Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016
- ↑ Marcus RH, Sareli P, Pocock WA, Barlow JB (1994). "The spectrum of severe rheumatic mitral valve disease in a developing country. Correlations among clinical presentation, surgical pathologic findings, and hemodynamic sequelae". Ann Intern Med. 120 (3): 177–83. PMID 8043061.
- ↑ Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016
- ↑ Kusiak V, Brest AN (1986). "Acute mitral regurgitation: pathophysiology and management". Cardiovasc Clin. 16 (2): 257–80. PMID 3742524.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". J Am Coll Cardiol. 63 (22): 2438–88. doi:10.1016/j.jacc.2014.02.537. PMID 24603192.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". J Am Coll Cardiol. 63 (22): 2438–88. doi:10.1016/j.jacc.2014.02.537. PMID 24603192.