Fragile X syndrome: Difference between revisions
m (Bot: Automated text replacement (-{{SIB}} + & -{{EJ}} + & -{{EH}} + & -{{Editor Join}} + & -{{Editor Help}} +)) |
No edit summary |
||
| Line 14: | Line 14: | ||
MeshID = D005600 | | MeshID = D005600 | | ||
}} | }} | ||
{{ | {{Fragile X syndrome}} | ||
{{CMG}} | {{CMG}} | ||
Revision as of 13:42, 27 August 2012
For patient information click here
| Fragile X syndrome | |
 | |
|---|---|
| Location of FMR1 gene | |
| ICD-10 | Q99.2 |
| ICD-9 | 759.83 |
| OMIM | 309550 |
| DiseasesDB | 4973 |
| MeSH | D005600 |
|
Fragile X syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Fragile X syndrome On the Web |
|
American Roentgen Ray Society Images of Fragile X syndrome |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Fragile X syndrome is a syndrome of X-linked mental retardation. Boys with the syndrome may have large testicles (macroorchidism), prognathism, hypotonia and autism, and a characteristic but variable face with large ears, long face, high-arched palate, gynecomastia, and malocclusion. Additional abnormalities may include lordosis, heart defect, pectus excavatum, flat feet, shortening of the tubular bones of the hands, and joint laxity. Females who have one fragile chromosome and one normal X chromosome may range from normal to mild manifestations of the fragile X syndrome. The fragile X syndrome has an estimated incidence of 1 in 3600 males and 1 in 4,000–6,000 females. [1]
Background
Martin and Bell in 1943, described a pedigree of X-linked mental disability, without considering the macroorchidism.[2] In 1969 Chris and Weesam first sighted an unusual "marker X chromosome" in association with mental disability.[3] In 1970 Frederick Hecht coined the term "fragile site" (Renpenning's syndrome is not synonymous with the Martin-Bell (fragile X) syndrome). In Renpennig's syndrome there is no fragile site on the X chromosome. Renpenning’s cases had short stature, moderate microcephaly, and neurological disorders.
Escalante's syndrome is synonymous with the fragile X syndrome. This term has been used in Brazil and other South American countries.
Etiology
The fragile X syndrome is a genetic disorder caused by mutation of the FMR1 gene on the X chromosome. Mutation at that site is found in 1 out of about every 2000 males and 1 out of about every 259 females. (Incidence of the disease itself is about 1 in every 4000 females.)
FMR1 is divided into four allelic classes based on the number of CGG repeats present in the 5' untranslated region (5'UTR): 1.) Common alleles with 40 or less repeats 2.) Intermediate alleles with 41-54 repeats 3.) Premutation alleles with 55-200 repeats 4.) Full mutation alleles with greater than 200 repeats. Common, intermediate, and premutation alleles are normally unmethylated in the 5'UTR and FMR1 is transcriptionally active. Premutation alleles often have increased transcriptional activity. Full mutation alleles are usually hypermethylated in the 5'UTR and transcriptionally inactive.[4]
This methylation of the FMR1 locus in chromosome band Xq27.3 is believed to result in constriction of the X chromosome which appears 'fragile' under the microscope at that point, a phenomenon that gave the syndrome its name.
Mutation of the FMR1 gene leads to the transcriptional silencing of the fragile X-mental retardation protein, FMRP. FMRP serves as a counterbalance to protein synthesis induced by group 1 metabotropic glutamate receptor (mGluR) activation. The mGluR1 and mGluR5 proteins participate in cell signaling pathways that upregulate the expression of proteins involved in diverse neuronal functions such as dendritic spine elongation, fear memory (possibly correlated to autism), and long-term potentiation of the corticostriatal synapse (possibly correlated to obsessive-compulsive behavior).[5] mGluR signaling in FMRP deficient cells is associated with increased alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid receptor (AMPAR) uptake. The trafficking of AMPAR to and from synaptic membranes is thought to be essential to the synaptic processes involved in memory and learning. Unbalanced AMPAR trafficking may underlie the abnormal cognition seen in FXS patients and patients with other cognitive disorders, such as Alzheimer’s disease and schizophrenia.[6]
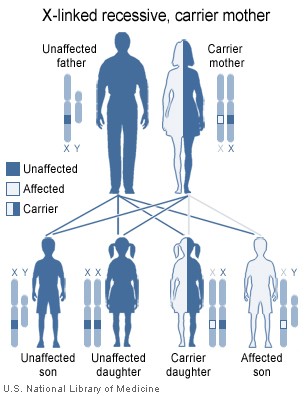
Transmission of the Fragile X
The diagram (right) of X-linked recessive inheritance is not entirely inappropriate but it markedly oversimplifies the situation and does not provide a sufficient foundation for genetic counseling about the fragile X syndrome. Technically, fragile X syndrome is an X-linked dominant condition with reduced penetrance.
Because males normally have only one copy of the X chromosome, those males with significant trinucleotide expansion at the FMR1 locus are symptomatic. They are intellectually disabled and may show various physical features of the fragile X syndrome.
Females have two X chromosomes and thus have double the chance of having a working FMR1 allele. Females carrying one X chromosome with an expanded FMR1 gene can have some signs and symptoms of the disorder or be normal. Although the extra X chromosome can serve as a backup, only one X chromosome is active at a time due to X-inactivation.
Males with the fragile X cannot transmit it to any of their sons (since males contribute a Y chromosome, not an X, to their male offspring), but will transmit it to all of their daughters, as males contribute their X to all of their daughters.
Females carrying one copy of the fragile X can transmit it to their sons or daughters; in this case each child has a 50% chance of inheriting the fragile X. Sons who receive the fragile X are at high risk of intellectual disability. Daughters who receive the fragile X may appear normal or they may be intellectually disabled, usually to a lesser degree than boys with the syndrome. The transmission of fragile X often increases with each passing generation. This seemingly anomalous pattern of inheritance is referred to as the Sherman paradox.
Symptoms
File:Fragile x syndrom.png Aside from intellectual disability, prominent characteristics of the syndrome include an elongated face, large or protruding ears, flat feet, larger testicles in men (macroorchidism), and low muscle tone. Speech may include cluttered speech or nervous speech[7]. Behavioral characteristics may include stereotypic movements (e.g., hand-flapping) and atypical social development, particularly shyness and limited eye contact. Some individuals with the fragile X syndrome also meet the diagnostic criteria for autism. Most females experience symptoms to a lesser degree because of their second X-chromosome, however they can develop just as severe symptoms. While full mutation males tend to present with severe intellectual disability, the symptoms of full mutation females runs the gamut of minimally affected to severe intellectual disability, which may explain why females are underdiagnosed relative to males.
Diagnosis
Fragile X syndrome was originally diagnosed by culturing cells in a folate deficient medium and then assessing the cultures for X-chromosome breakage by cytogenetic analysis of the long arm of the X chromosome. This technique proved unreliable for both diagnosis and carrier testing.
The fragile X abnormality is now directly determined by analysis of the number of CGG repeats and their methylation status using restriction endonuclease digestion and Southern blot analysis.
Treatment and current research
Recent studies have focused on a number of critical areas. The role of FMRP's RNA partners, many of which have now been validated through in vitro assays, is of primary importance. Also being examined is the function the various domains of FMRP, an RNA-binding protein, which is still relatively unknown. One hypothesis is that many symptoms are caused by unchecked activation of mGluR5, a metabotropic glutamate receptor, which was found in a 2007 study to contribute significantly to the pathogenesis of the disease;[8] this suggests that mGluR5 blockers could be used to treat fragile X syndrome.[9]
While there is no current cure for the syndrome, there is hope that further understanding of its underlying causes would lead to new therapies. Currently, the syndrome can be treated through behavioral therapy, special education, medication, and when necessary, treatment of physical abnormalities. Persons with the fragile X syndrome in their family histories are advised to seek genetic counseling to assess the likelihood of having children who are affected, and how severe any impairments may be in affected descendants.
Researchers at the Picower Institute for Learning and Memory at MIT have reversed symptoms of mental retardation and autism in mice.[10]
References
- ↑ Crawford, D.C.; Acuna, J.M. & Sherman, S.L. (2001) "FMR1 and the Fragile X syndrome: Human genome epidemiology review". Genet Med 3: 359-371
- ↑ Martin, J. P. & Bell, J. "A pedigree of mental defect showing sex-linkage". Journal of neurology, neurosurgery, and psychiatry (J. Neurol. Psychiat.). BMJ Publishing Group, London 6.1943, 154-157. Template:ISSN
- ↑ Lubs, H. (1969) "A marker X chromosome". Am Hum Genet 21: 231.
- ↑ Garber KB, Visootsak J, and Warren ST (2008) "Fragile X Syndrome". European Journal of Human Genetics 16: 666-672.
- ↑ GBear MF, Huber KM, Warren ST (2004) "The mGluR theory of fragile X mental retardation". Trends in Neurosciences 27: 370-377.
- ↑ Nakamoto M, Nalavadi V, Epstein MP, Narayanan U, Bassell GJ, Warren ST (2007) "Fragile X mental retardation protein deficiency leads to excessive mGluR5-dependent internalization of AMPA receptors". Neuroscience 104: 15537-15542.
- ↑ http://www.wrongdiagnosis.com/f/fragile_x_syndrome/signs.htm
- ↑ Dölen G, Osterweil E, Rao BS; et al. (2007). "Correction of fragile X syndrome in mice". Neuron. 56 (6): 955–62. doi:10.1016/j.neuron.2007.12.001. PMID 18093519.
- ↑ Highfield R (2007-12-19). "Fragile X study offers hope for autism treatment". Daily Telegraph. Retrieved 2007-12-22.
- ↑ MIT researchers reverse symptoms in mice of leading inherited cause of mental retardation
External links
Template:Pervasive developmental disorders Template:Chromosomal abnormalities