Follicular lymphoma pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
==Pathophysiology== | ==Pathophysiology== | ||
===Genetics=== | ===Genetics=== | ||
A [[Chromosomal translocation|translocation]] between [[chromosome]] 14 and 18 results in the overexpression of the ''[[BCL-2]]'' gene | A [[Chromosomal translocation|translocation]] between [[chromosome]] 14 and 18 results in the overexpression of the ''[[BCL-2]]'' gene<ref name="pmid12529293">{{cite journal |author=Bosga-Bouwer AG, van Imhoff GW, Boonstra R, ''et al.'' |title=Follicular lymphoma grade 3B includes 3 cytogenetically defined subgroups with primary t(14;18), 3q27, or other translocations: t(14;18) and 3q27 are mutually exclusive |journal=Blood |volume=101 |issue=3 |pages=1149–54 |date=February 2003 |pmid=12529293 |doi=10.1182/blood.V101.3.1149 |url=http://www.bloodjournal.org/cgi/pmidlookup?view=long&pmid=12529293}}</ref>. As the bcl-2 protein is normally involved in preventing [[apoptosis]], cells with an overexpression of this protein are basically immortal. The ''[[BCL-2]]'' gene is normally found on chromosome 18, and the translocation moves the gene near to the site of the immunoglobulin heavy chain enhancer element on chromosome 14. | ||
Translocations of ''BCL6'' at 3q27 can also be involved | Translocations of ''BCL6'' at 3q27 can also be involved<ref name="pmid16075463">{{cite journal |author=Bosga-Bouwer AG, Haralambieva E, Booman M, ''et al.'' |title=BCL6 alternative translocation breakpoint cluster region associated with follicular lymphoma grade 3B |journal=Genes Chromosomes Cancer |volume=44 |issue=3 |pages=301–4 |date=November 2005 |pmid=16075463 |doi=10.1002/gcc.20246}}</ref>. | ||
It is positive for the B-cell markers | It is positive for the B-cell markers [[CD10]], [[CD19]], [[CD22]], and usually [[CD20]]<ref>[http://pleiad.umdnj.edu/hemepath/follicular/follicular.html Overview] at [[University of Medicine and Dentistry of New Jersey|UMDNJ]]</ref> but almost always negative for [[CD5]]<ref name="pmid11419985">{{cite journal |author=Barekman CL, Aguilera NS, Abbondanzo SL |title=Low-grade B-cell lymphoma with coexpression of both CD5 and CD10. A report of 3 cases |journal=Arch. Pathol. Lab. Med. |volume=125 |issue=7 |pages=951–3 |date=July 2001 |pmid=11419985 |doi= 10.1043/0003-9985(2001)125<0951:LGBCLW>2.0.CO;2|url=http://journals.allenpress.com/jrnlserv/?request=get-abstract&issn=0003-9985&volume=125&page=951}}</ref>. | ||
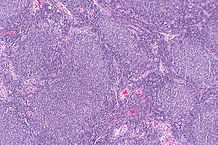
[[Image:192px-Lymphoma macro.jpg|thumb|right|top|350px|Follicular lymphoma replacing a lymph node.]] | [[Image:192px-Lymphoma macro.jpg|thumb|right|top|350px|Follicular lymphoma replacing a lymph node.]] | ||
Revision as of 15:02, 28 August 2015
|
Follicular lymphoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Follicular lymphoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Follicular lymphoma pathophysiology |
|
Risk calculators and risk factors for Follicular lymphoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sowminya Arikapudi, M.B,B.S. [2]
Overview
Follicular lymphoma is defined as a lymphoma of follicle center B-cells (centrocytes and centroblasts), which has at least a partially follicular pattern. Genes involved in the pathogenesis of follicular lymphoma include BCL-2, and BCL-6. The progression to follicular lymphoma involves the microRNAs (miRNAs). On microscopic histopathological analysis, centrocytes, and centroblasts are characteristic findings of follicular lymphoma.
Pathophysiology
Genetics
A translocation between chromosome 14 and 18 results in the overexpression of the BCL-2 gene[1]. As the bcl-2 protein is normally involved in preventing apoptosis, cells with an overexpression of this protein are basically immortal. The BCL-2 gene is normally found on chromosome 18, and the translocation moves the gene near to the site of the immunoglobulin heavy chain enhancer element on chromosome 14. Translocations of BCL6 at 3q27 can also be involved[2]. It is positive for the B-cell markers CD10, CD19, CD22, and usually CD20[3] but almost always negative for CD5[4].

MicroRNA expression
Recently, it was described that short non-coding RNAs named microRNAs (miRNAs) have important functions in lymphoma biology, including follicular lymphoma. In malignant B cells miRNAs participate in pathways fundamental to B cell development like
- B cell receptor (BCR) signalling
- B cell migration/adhesion, cell-cell interactions in immune niches
- The production and class-switching of immunoglobulins.[5]
MiRNAs influence B cell maturation, generation of pre-, marginal zone, follicular, B1, plasma and memory B cells.[5]
 |
Microscopic Pathology
The tumor is composed of follicles containing a mixture of
- Centrocytes (Kiel nomenclature adopted by WHO experts) or cleaved follicle center cells (older American nomenclature), small cells.
- Centroblasts (Kiel nomenclature adopted by WHO experts) or large noncleaved follicle center cells (older American nomenclature), "large cells.
- These follicles are surrounded by non-malignant cells, mostly T-cells.
In the follicles, centrocytes typically predominate; centroblasts are usually in minority.
 |
Grading
According to the WHO criteria, the disease is morphologically graded into:[6]
- grade 1 (<5 centroblasts per high-power field (hpf))
- grade 2 (6–15 centroblasts/hpf)
- grade 3 (>15 centroblasts/hpf)
- grade 3A (centrocytes still present)
- grade 3B (the follicles consist almost entirely of centroblasts)
The WHO 2008 update classifies
- Grades 1 and 2 now as low grade follicular lymphoma
- Grade 3A as high grade follicular lymphoma
- Grade 3B as diffuse large B Cell Lymphoma
References
- ↑ Bosga-Bouwer AG, van Imhoff GW, Boonstra R; et al. (February 2003). "Follicular lymphoma grade 3B includes 3 cytogenetically defined subgroups with primary t(14;18), 3q27, or other translocations: t(14;18) and 3q27 are mutually exclusive". Blood. 101 (3): 1149–54. doi:10.1182/blood.V101.3.1149. PMID 12529293.
- ↑ Bosga-Bouwer AG, Haralambieva E, Booman M; et al. (November 2005). "BCL6 alternative translocation breakpoint cluster region associated with follicular lymphoma grade 3B". Genes Chromosomes Cancer. 44 (3): 301–4. doi:10.1002/gcc.20246. PMID 16075463.
- ↑ Overview at UMDNJ
- ↑ Barekman CL, Aguilera NS, Abbondanzo SL (July 2001). "Low-grade B-cell lymphoma with coexpression of both CD5 and CD10. A report of 3 cases". Arch. Pathol. Lab. Med. 125 (7): 951–3. doi:10.1043/0003-9985(2001)125<0951:LGBCLW>2.0.CO;2. PMID 11419985.
- ↑ 5.0 5.1 Musilova, K; Mraz, M (2014). "MicroRNAs in B cell lymphomas: How a complex biology gets more complex". Leukemia. doi:10.1038/leu.2014.351. PMID 25541152.
- ↑ "Follicular Lymphomas". Retrieved 2008-07-26.