Dextromethorphan: Difference between revisions
Gerald Chi (talk | contribs) m (Changed protection level for "Dextromethorphan" ([Edit=Allow only autoconfirmed users] (expires 18:55, 25 February 2014 (UTC)) [Move=Allow only autoconfirmed users] (expires 18:55, 25 February 2014 (UTC)))) |
No edit summary |
||
| Line 21: | Line 21: | ||
| routes_of_administration = Oral | | routes_of_administration = Oral | ||
}} | }} | ||
{{CMG}} | {{CMG}}<br> | ||
<small>'''''Street Names/Slangs:CCC, DXM, Orange crush, Red devils, Robo, Robo-trippin, skittles, Triple C, Tussin'''''</small> | |||
Latest revision as of 19:27, 11 February 2014
 | |
 | |
| Clinical data | |
|---|---|
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 11%[1] |
| Metabolism | Hepatic (liver) enzymes: major CYP2D6, minor CYP3A4, and minor CYP3A5 |
| Elimination half-life | 1.4–3.9 hours |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
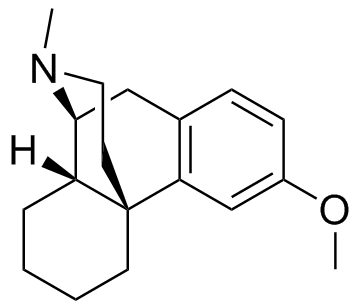
| Formula | C18H25NO |
| Molar mass | 271.4 g/mol |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Street Names/Slangs:CCC, DXM, Orange crush, Red devils, Robo, Robo-trippin, skittles, Triple C, Tussin
Dextromethorphan (DXM or DM) is an antitussive (cough-suppressant) drug found in many over-the-counter cold and cough medicines. Dextromethorphan has also found other uses in medicine, ranging from pain relief to psychological applications. Pure dextromethorphan occurs as a powder made up of white crystals, but it is generally administered via syrups, tablets, or lozenges manufactured under several different brand names and generic labels.
When taken at doses higher than are medically recommended, dextromethorphan acts as a dissociative hallucinogen[2]. It exhibits neurotoxic and hallucinogenic effects similar to those of the controlled substance ketamine and phencyclidine (PCP), which afford it a high potential for abuse.
Chemistry
Dextromethorphan hydrobromide monohydrate is a salt of the methyl ether dextrorotatory isomer of levorphanol, a narcotic analgesic. It is chemically named as 3-methoxy-17-methyl-9(alpha), 13(alpha), 14(alpha)-morphinan hydrobromide monohydrate. DXM occurs as white crystals, is sparingly soluble in water, and freely soluble in alcohol. The drug is dextrorotatory in water (at 20 degrees Celsius, Sodium D-line) with a specific rotation of +27.6 degrees.
Indications
The primary use of dextromethorphan is as a cough suppressant, for the temporary relief of cough caused by minor throat and bronchial irritation; as commonly accompanies the common cold, as well as other causes such as inhaled irritants.
A combination of dextromethorphan and quinidine has been shown to alleviate symptoms of easy laughing and crying (pseudobulbar affect) in patients with amyotrophic lateral sclerosis and multiple sclerosis.[3]
Dextromethorphan is being investigated as a possible treatment for pain associated with fibromyalgia, a chronic rheumatological organic fatigue disorder.[4]
Dextromethorphan is also useful in breaking addictions to narcotics and other habit-forming drugs (including nicotine), since it is an inhibitor of many of the brain receptors involved in narcotic action on the brain. For this purpose, DXM is more effective when combined with an oxidase inhibitor such as quinidine.[5]
Pharmacokinetics
At therapeutic doses, the drug acts centrally to elevate the threshold for coughing, without inhibiting ciliary activity. Dextromethorphan is rapidly absorbed from the gastrointestinal tract and metabolizes within 15–60 minutes of ingestion. The duration of action after oral administration is approximately three to eight hours for dextromethorphan-hydrobromide and 10 to 12 hours for dextromethorphan-polistirex. Because administration of DXM can trigger a histamine release (an allergic reaction), its use in atopic children is very limited.
The average dosage necessary for effective antitussive therapy is between 10 mg and 30 mg. The time to re-dose depends on the specific preparation being used.
Side-effects
Side-effects of dextromethorphan use can include body rash/itching, disassociation, nausea as well as other gastrointestinal disturbances, drowsiness, dizziness, excitation, vomiting, blurred vision, dilated pupils, sweating, fever, hypertension, shallow respiration, diarrhea, urinary retention, and increases in heart rate, blood pressure, and body temperature.[6]
Dextromethorphan can also produce psychological dependence due to its potential for recreational use, but does not produce physical addiction, according to the WHO Committee on Drug Dependence.
Dextromethorphan, when combined with guaifenesin, an expectorant used in many preparations, is likely to cause nausea and vomiting when the combination is taken at high doses.[6]
Olney's Lesions
Like other NMDA receptor antagonists, it is postulated that high doses of dextromethorphan can cause a type of brain damage known as Olney's lesions.[7][8] Studies conducted on rats have shown that high doses of the NMDA receptor antagonist MK-801 caused vacuoles to form in certain regions of test rats' brains that developed into irreversible lesions, and experts say that it is possible that similar brain damage can occur in humans.[9]
It may be important to note that injected dextromethorphan has been shown to cause the vacuolization, [10] whereas oral administration of dextromethorphan in rat studies does not appear to cause the same effect.[11]
Drug interactions
Dextromethorphan should not be taken with any of the following:
- monoamine oxidase inhibitors (MAOIs)[6]
- selective serotonin reuptake inhibitors (SSRIs)[6]
- CNS depressant drugs and substances, including alcohol, antihistamines, and psychotropics, will have a cumulative CNS depressant effect if taken with dextromethorphan.[6]
- CYP2D6 inhibitors can increase the effects of dextromethorphan. Examples of these include chlorpromazine, delavirdine, fluoxetine, miconazole, paroxetine, pergolide, quinidine, quinine, ritonavir, and ropinirole.[12]
DXM taken with any of these can cause Serotonin syndrome, a potentially life-threatening adverse drug reaction that results from intentional self-poisoning, therapeutic drug use, or inadvertent interactions between drugs which cause an excess of serotonergic activity at central nervous system (CNS) and peripheral serotonin receptors.
Contraindications
- Atopic children should be administered dextromethorphan only under the strict supervision of a health care professional.[6]
Clinical pharmacology
Following oral administration, dextromethorphan is rapidly absorbed from the gastrointestinal tract, where it enters the bloodstream and crosses the blood-brain barrier. The first-pass through the hepatic portal vein results in some of the drug being metabolized into an active metabolite of dextromethorphan, dextrorphan, the 3-hydroxy derivative of dextromethorphan. The therapeutic activity of dextromethorphan is believed to be caused by both the drug and this metabolite. Dextromethorphan is metabolized by various liver enzymes and subsequently undergoes O-demethylation (producing dextrorphan), N-demethylation, and partial conjugation with glucuronic acid and sulfate ions. Hours after dextromethorphan therapy, (in humans) the metabolites (+)-3-hydroxy-N-methylmorphinan, (+)-3-morphinan, and traces of the unchanged drug are detectable in the urine.[6]
A major metabolic catalyst involved is the cytochrome P450 enzyme known as 2D6, or CYP2D6. A significant portion of the population has a functional deficiency in this enzyme and are known as poor CYP2D6 metabolizers. As CYP2D6 is a major metabolic pathway in the inactivation of dextromethorphan, the duration of action and effects of dextromethorphan can be increased by as much as three times in such poor metabolizers.[13]
A large number of medications (including antidepressants) are potent inhibitors of CYP2D6. There exists, therefore, the potential of interactions between dextromethorphan and concomitant medications. There have been reports of fatal consequences arising from such interactions.[14]
Dextromethorphan crosses the blood-brain barrier, and the following pharmacological actions have been reported:
- NMDA glutamatergic receptor antagonist
- σ1 and σ2 receptor agonist.[15]
- α3β4 nicotinic receptor antagonist[16]
- Serotonin reuptake inhibitor[17]
- Dopamine reuptake inhibitor (disputed)[6][18]
History
Dextromethorphan was first patented with U.S. Patent 2,676,177. The FDA approved dextromethorphan for over-the-counter sale as a cough suppressant in 1958. This filled the need for a cough suppressant lacking the sedative side-effects, stronger potential for abuse, and physically addictive properties of codeine phosphate, the most widely-used cough medication at the time (now prescription-only in the United States).[19] As with most cough suppressants, studies show that dextromethorphan's effectiveness is highly debatable,[20] especially in children.[21]
During the 1960s and 1970s, DXM became available in an over-the-counter tablet form by the brand name Romilar. It was put on the shelves in hopes of cutting down on codeine cough remedies. In 1973, Romilar was taken off the shelves after a burst in sales due to common recreational use, and was replaced by cough syrup in an attempt to cut down on recreational use.[19]
More recently (around 2000) gel capsule forms began reappearing in the form of Robitussin CoughGels as well as several generic forms of that preparation.
Recreational use
Since their introduction, over-the-counter preparations containing the drug dextromethorphan have been used in a manner inconsistent with their labeling, often as a recreational drug, to induce intoxication.[19] Dextromethorphan has little to no psychological effect in the doses used medically; however, alteration of consciousness generally occurs following ingestion of approximately 7 to 50 times the therapeutic dose over a relatively short period of time.[19]
Slang terms for DXM often correlate to the brands of cough medicine used, such as "tussin," "robo," "dex," "triple C's," and "skittles." Recreational use of DXM is frequently referred to in verb form as "dexing," "tussing," "roboing," and "robotripping." Due to abuse and theft concerns, many retailers in the US have moved DXM-containing products behind the counter so that one must ask a pharmacist to receive them or be 18 years (19 in NJ) or older to purchase them.
DXM is often found in "fake" ecstasy pills instead of MDMA because it is easier to come by than the chemical precursors of MDMA, is cheaper, and requires less knowledge of chemistry to extract than synthesizing MDMA. Sites such as TranceSafe.com [22] can help you identify which pills may contain DXM and may be harmful to your health.
Classification
At high doses, dextromethorphan is classified as a dissociative hallucinogenic drug, like ketamine and phencyclidine (PCP).[23][24] It generally does not produce withdrawal symptoms characteristic of physically addictive substances, but cases of psychological addiction have been reported.
Legality
Antitussive preparations containing DXM are legal to purchase from most pharmacies worldwide. Since DXM's use as a recreational drug usually involves only the ingestion of large quantities of an over-the-counter medication, no legal distinction currently exists between medical and recreational use, sale, or purchase.
The sale of DXM in its pure powder form may incur penalties in the United States, although no explicit law exists prohibiting its sale. There have been cases of individuals incurring time in prison and other penalties for selling pure DXM in this form, due to the incidental breaking of related drug laws — such as resale of a medication without proper warning labels.[23]
DXM was excluded from the Controlled Substances Act (CSA) of 1970 and was specifically excluded from the Single Convention on Narcotic Drugs. DXM is still excluded from the CSA (as of 2007), however officials have warned that it could still be added if increased recreational use warrants its scheduling.[19]
DXM appears to be available over the counter in most countries, with one exception being Hong Kong. [25]
Effects
DXM, when consumed in low recreational doses (usually under 200 mg), is described as having a euphoric effect. With higher doses (about 400 mg), intense euphoria (or dysphoria), vivid imagination, and closed-eye hallucinations may occur. With very high doses (600 mg and over), profound alterations in consciousness have been noted, and users often report out-of-body experiences or temporary psychosis.[26][27] Frequent and long-term usage at very high doses can lead to toxic psychosis and other permanent psychological problems.[19] Most users find such high doses to be extremely uncomfortable and are unwilling to repeat them. Flanging (speeding up or slowing down) of sensory input is characteristic at any recreational dosing level.
In 1981, a paper by Gosselin estimated the lethal dose to be between 50 and 500 mg/kg. It is generally accepted that the antidote to DXM overdose is naloxone, administered intravenously.[28]
Many negative reports of recreational use have come from individuals who inadvertently overdosed on a multi-symptom cold medication, rather than using a cough suppressant whose sole active ingredient is dextromethorphan. Combination products would certainly produce a negative experience and are highly unsafe. Multi-symptom cold medicines contain other active ingredients, such as guaifenesin, acetaminophen, and chlorphenamine, any of which can cause permanent bodily damage, or even death, if taken on the generally-accepted recreational dosing scale of DXM.[29][30]
Duration
The effects of recreational dosing generally last as long as medical dosing of the same DXM preparation. In other words, taking a recreational dose of an eight-hour DXM-containing cough suppressant will generally produce recreational effects lasting eight hours. The time until wear-off depends on the tolerance of the individual user, as well as on the type of dextromethorphan taken. Dextromethorphan-polistirex is contained in extended-release cough suppressants (generally lasting up to 12 hours) and therefore will produce a longer-lasting recreational effect than the more common and shorter-acting form, dextromethorphan-hydrobromide. Dosage itself has relatively little impact on the length of time the effects last — meaning that taking more DXM is much more likely to heighten its effects rather than lengthen them.
It is possible that DXM also causes an "afterglow," for as long as one to 14 hours after the actual dose wears off.
Psychopharmacology
Biochemically, DXM's psychological effects can be attributed largely to dextrorphan (DXO), a chemical by-product (or metabolite) that is produced when DXM metabolizes within the body. Both DXO and DXM are NMDA receptor antagonists,[31] just like the dissociative hallucinogenic drugs ketamine and phencyclidine (PCP); however for that purpose, DXO is more potent than DXM.[32]
Just like all NMDA receptor antagonists, DXO/DXM inhibit neurotransmitters (specifically glutamate) from activating neurotransmitter receptors in the brain. This can effectively slow or even shut down certain neural pathways, preventing the brain from "communicating with itself," so to speak, which leaves the user feeling dissociated, "disconnected," or "outside" one's own body.[33][34]
DXM's euphoric effects have sometimes been attributed to it triggering an increase in dopamine levels, since such an increase generally correlates to a pleasurable response to a drug in humans and animals, as is observed with antidepressant drugs. However the effect of DXO and DXM on dopamine levels is a disputed subject. Some studies show that NMDA receptor antagonists in general (ketamine and PCP, for example) will raise dopamine levels.[35][18] However, there is also evidence that DXO and DXM don't affect dopamine levels at all — a property exhibited by dizocilpine, another NMDA receptor antagonist. Some findings even suggest that DXM actually counters the dopamine increase caused by morphine.[6][36][37][38] Due to these conflicting results, the actual effect of DXM on dopamine levels is yet to be fully determined.
Recreational effects are generally temporary, however chronic high-dose usage of DXM can lead to toxic psychosis or other psychological problems.[19] In addition, inadvertent overdose of accompanying active ingredients in multi-symptom cold medications can cause permanent physiological damage.
References
- ↑ "Plasma profile and pharmacokinetics of dextromethorphan after intravenous and oral administration". Journal of Veterinary Pharmacology and Therapeutics.
- ↑ http://www.drugabuse.gov/InfoFacts/PainMed.html
- ↑ Brooks B, Thisted R, Appel S, Bradley W, Olney R, Berg J, Pope L, Smith R (2004). "Treatment of pseudobulbar affect in ALS with dextromethorphan/quinidine: a randomized trial". Neurology. 63 (8): 1364–70. PMID 15505150.
- ↑ "Cough Drug May Help Fibromyalgia Pain". WebMD.
- ↑ "Patent application". FreePatentsOnline.com.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 "Dextromethorphan". NHTSA.
- ↑ Olney J, Labruyere J, Price M (1989). "Pathological changes induced in cerebrocortical neurons by phencyclidine and related drugs". Science. 244 (4910): 1360–2. PMID 2660263.
- ↑ Hargreaves R, Hill R, Iversen L. "Neuroprotective NMDA antagonists: the controversy over their potential for adverse effects on cortical neuronal morphology". Acta Neurochir Suppl (Wien). 60: 15–9. PMID 7976530.
- ↑ http://www.erowid.org/chemicals/dxm/dxm_health2.shtml
- ↑ Hashimoto, K; Tomitaka, S; Narita, N; Minabe, Y; Iyo, M; Fukui, S (1996). "Induction of heat shock protein HSP-70 in rat retrosplenial cortex following administration of dextromethorphan". Environmental Toxicology and Pharmacology. 1 (4): 235–239.
- ↑ Carliss RD, Radovsky A, Chengelis CP, O'neill TP, Shuey DL (2007). "Oral administration of dextromethorphan does not produce neuronal vacuolation in the rat brain". doi:10.1016/j.neuro.2007.03.009. PMID 17573115.
- ↑ http://www.healthanddna.com/drugchart.htm
- ↑ "Clinical Pharmacology & Therapeutics - Abstract of article: The influence of CYP2D6 polymorphism and quinidine on the disposition and antitussive effect of dextromethorphan in humans[ast]". Retrieved 2007-07-16.
- ↑ Jones K, Taranto M (2006). "Illicit Drug Manual: Dextromethorphan ("Robo-tripping")". collegehealth-e. 1 (4): 13–17.
- ↑ "British Journal of Pharmacology - The dextromethorphan analog dimemorfan attenuates kainate-induced seizures via [sigma]1 receptor activation: comparison with the effects of dextromethorphan". Retrieved 2007-07-16.
- ↑ Hernandez SC, Bertolino M, Xiao Y, Pringle KE, Caruso FS, Kellar KJ (2000). "Dextromethorphan and its metabolite dextrorphan block alpha3beta4 neuronal nicotinic receptors". J. Pharmacol. Exp. Ther. 293 (3): 962–7. PMID 10869398.
- ↑ Kamei J, Mori T, Igarashi H, Kasuya Y (1992). "Serotonin release in nucleus of the solitary tract and its modulation by antitussive drugs". Res. Commun. Chem. Pathol. Pharmacol. 76 (3): 371–4. PMID 1636059.
- ↑ 18.0 18.1 Verma A, Moghaddam B (1996). "NMDA receptor antagonists impair prefrontal cortex function as assessed via spatial delayed alternation performance in rats: modulation by dopamine". Journal of Neuroscience. 1: 373–9. Unknown parameter
|month=ignored (help); Unknown parameter|day=ignored (help) - ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 http://www.cesar.umd.edu/cesar/drugs/dxm.asp
- ↑ Cough medicines "have no benefit" BBC News: Health, Tuesday, July 6, 2004. Accessed July 28 2007.
- ↑ [1] "Kids' cough medicine no better than placebo" San Francisco Chronicle, July 8, 2004
- ↑ http://www.TranceSafe.com
- ↑ 23.0 23.1 http://www.erowid.org/psychoactives/research_chems/research_chems_law3.pdf
- ↑ http://www.erowid.org/chemicals/dxm/dxm_effects.shtml
- ↑ http://www.erowid.org/chemicals/dxm/dxm_law.shtml
- ↑ Bornstein, S; Czermak, M; Postel, J., (1968). "Apropos of a case of voluntary medicinal intoxication with dextromethorphan hydrobromide". Annales Medico-Psychologiques. 1 (3): 447–451.
- ↑ Dodds A, Revai E (1967). "Toxic psychosis due to dextromethorphan". Med J Aust. 2: 231.
- ↑ Schneider SM, Michelson EA; et al. (1991). "Dextromethorphan poisoning reversed by naloxone". Am. J. Emerg. Med. 9: 237–238.
- ↑ Kirages T, Sulé H, Mycyk M (2003). "Severe manifestations of coricidin intoxication". Am J Emerg Med. 21 (6): 473–5. PMID 14574654.
- ↑ Kintz, P. and Mangin, P. (1992). "Toxicological findings in a death involving dextromethorphan and terfenadine". Am J Forensic Med Pathol. 13 (4): 351–352. Unknown parameter
|month=ignored (help) - ↑ http://cat.inist.fr/?aModele=afficheN&cpsidt=914417
- ↑ http://jpet.aspetjournals.org/cgi/content/full/309/2/515?ijkey=73c6efcf7713b02798c855b5ce4d50f1aa22d299&keytype2=tf_ipsecsha#ABS
- ↑ Muir, KW (1995). "Clinical experience with excitatory amino acid antagonist drugs". Stroke. 26 (3): 503–513. Retrieved 2007-01-17. Unknown parameter
|coauthors=ignored (help) - ↑ Kristensen, JD (1992). "The NMDA-receptor antagonist CPP abolishes neurogenic 'wind-up pain' after intrathecal administration in humans". Pain. 51 (2): 249–253. PMID 1484720. Unknown parameter
|coauthors=ignored (help);|access-date=requires|url=(help) - ↑ http://www.nature.com/mp/journal/v7/n8/full/4001093a.html
- ↑ Steinmiller, CL (2003). "Effects of dextromethorphan on dopamine release in the nucleus accumbens: Interactions with morphine". Pharmacol Biochem Behav. Center for Neuropharmacology and Neuroscience (MC-136). 74 (4): 803–10. PMID 12667894. Unknown parameter
|coauthors=ignored (help);|access-date=requires|url=(help) - ↑ Carrozza, DP (1992). "In vivo modulation of excitatory amino acid receptors: microdialysis studies on N-methyl-D-aspartate-evoked striatal dopamine release and effects of antagonists". Brain Res. 74 (4): 803–10. PMID 1353403. Unknown parameter
|coauthors=ignored (help);|access-date=requires|url=(help) - ↑ Huang, EY (2003). "Co-administration of dextromethorphan with morphine attenuates morphine rewarding effect and related dopamine releases at the nucleus accumbens". Brain Res. 368 (5): 386–92. PMID 14564449. Unknown parameter
|coauthors=ignored (help);|access-date=requires|url=(help)
See also
External links
- Dextroverse
- Dextromethorphan FAQ at third-plateau.org
- Erowid
- Dextromethorphan User Forums at Fourth-plateau.org
Template:Dissociative psychedelics Template:Cough and cold preparations
de:Dextromethorphan et:Dekstrometorfaan hu:Dextromethorphan nl:Dextromethorfan fi:Dekstrometorfaani sv:Dextrometorfan
- Pages with script errors
- CS1 maint: Multiple names: authors list
- Pages with citations using unsupported parameters
- CS1 maint: Explicit use of et al.
- Pages using citations with accessdate and no URL
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Articles containing unverified chemical infoboxes
- Antitussives
- Dissociatives
- Dopamine reuptake inhibitors
- Morphinans
- NMDA receptor antagonists
- Sigma agonists