Antibiotic resistant gonorrhea
|
Gonorrhea Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Antibiotic resistant gonorrhea On the Web |
|
American Roentgen Ray Society Images of Antibiotic resistant gonorrhea |
|
Risk calculators and risk factors for Antibiotic resistant gonorrhea |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mehrsefat, M.D. [2]
Overview
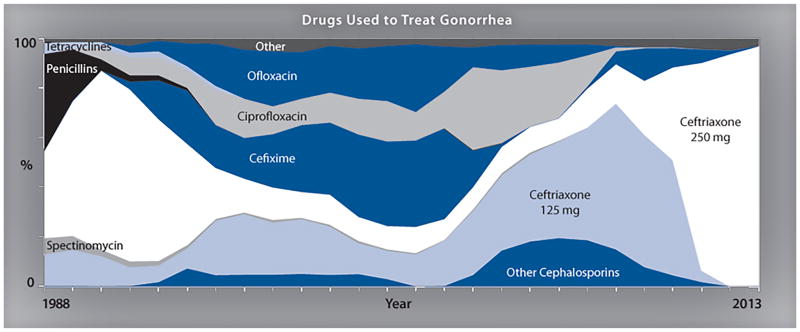
Gonorrhea treatment is complicated by the ability of Neisseria gonorrhoeae to develop resistance to antimicrobials. High-level resistance to expanded-spectrum cephalosporins and [Azithromycin]] is now reported, and it seems developing another effective treatment has become unaffordable. Although new combination antibiotic treatments are being evaluated. There are no affordable alternative therapeutic options currently available for the treatment of gonococcal disease. and it seems even newly developed antibiotics will be short solution and may be developed resistance as well.[1]
Antibiotic Resistant
- Gonorrhea treatment is complicated by the ability of Neisseria gonorrhoeae to develop resistance to antimicrobials, therefore a combination therapy with Azithromycin and a Cephalosporin is used to improve treatment efficacy and potentially slow the emergence and spread of resistance.
- High-level resistance to these expanded-spectrum cephalosporins is now reported, and it seems developing another effective treatment has become unaffordable.
- Although new combination antibiotic treatments are being evaluated. There are no affordable alternative therapeutic options currently available for the treatment of gonococcal disease. and it seems even newly developed antibiotics will be short solution and may be developed resistance as well.[1]
- In 2006, CDC had five recommended treatment options for gonorrhea—now the U.S. has only one option remaining.
The drug resistance may be developed by following mechanisms:
- Chromosomal mutations
- Acquisition of R factors (plasmids)
Gonococcal Isolate Surveillance Project
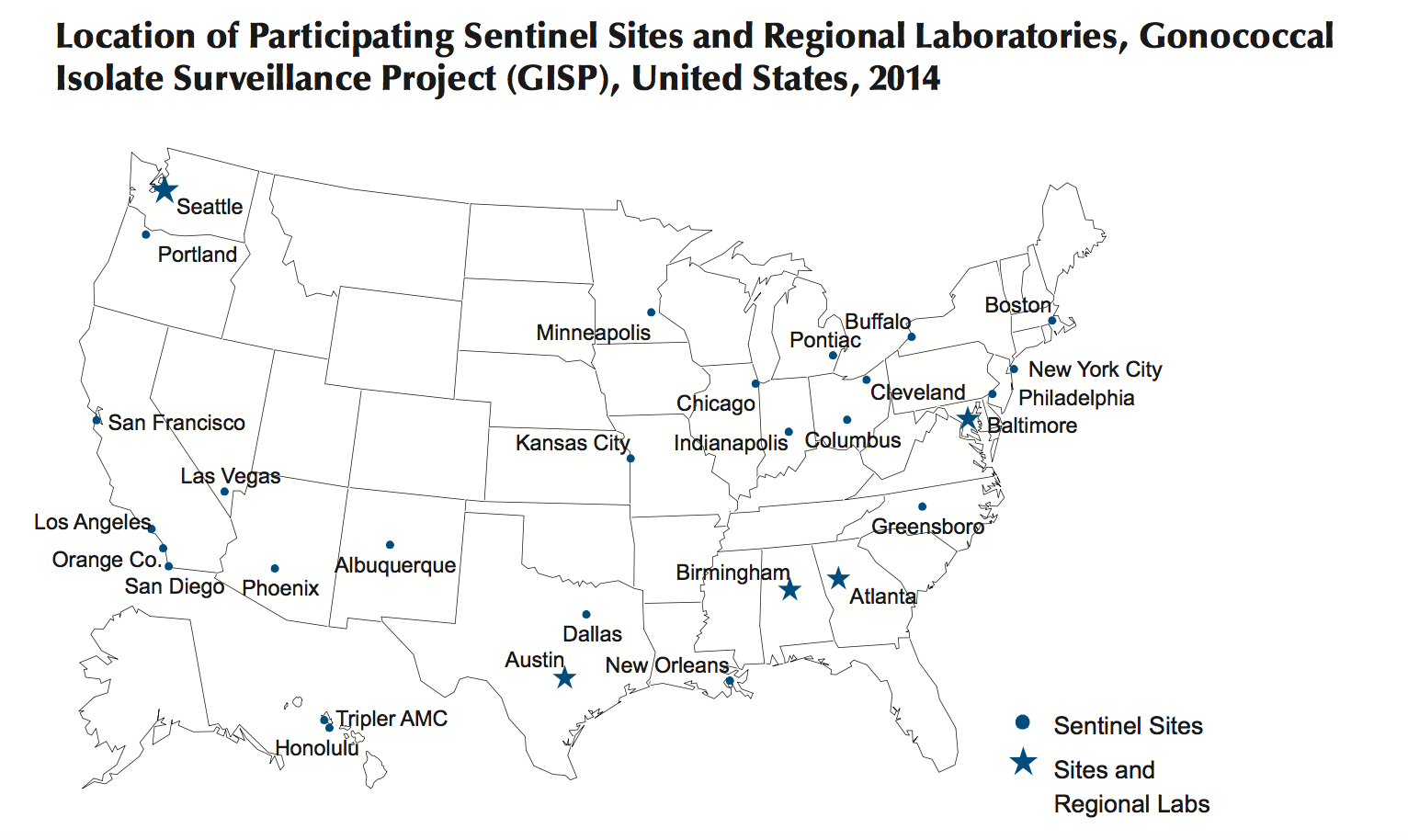
Antimicrobial resistance remains an important consideration in the treatment of gonorrhea.[2]
- In 1986, the CDC established the Gonococcal Isolate Surveillance Project (GISP)
- Data are collected from selected STD clinic sentinel sites and from regional laboratories in order to: [3]
- Monitor antimicrobial susceptibility trends in the United States
- Characterize male patients with gonococcal infection
- Phenotypically characterize antimicrobial-resistant isolates of Niesseira gonorrhea
Penicillin Susceptibility
Penicillin has not been a first-line treatment option for gonorrhea for a number of decades. However, it has been tested for surveillance purposes.
- In 2012, Almost 13.1% of Neisseria gonorrhoeae from the GISP survey were resistant to penicillin mainly with two mechanisms:
- Chromosomal penicillin resistance (82.3%)
- Penicillinase production (17.7%)
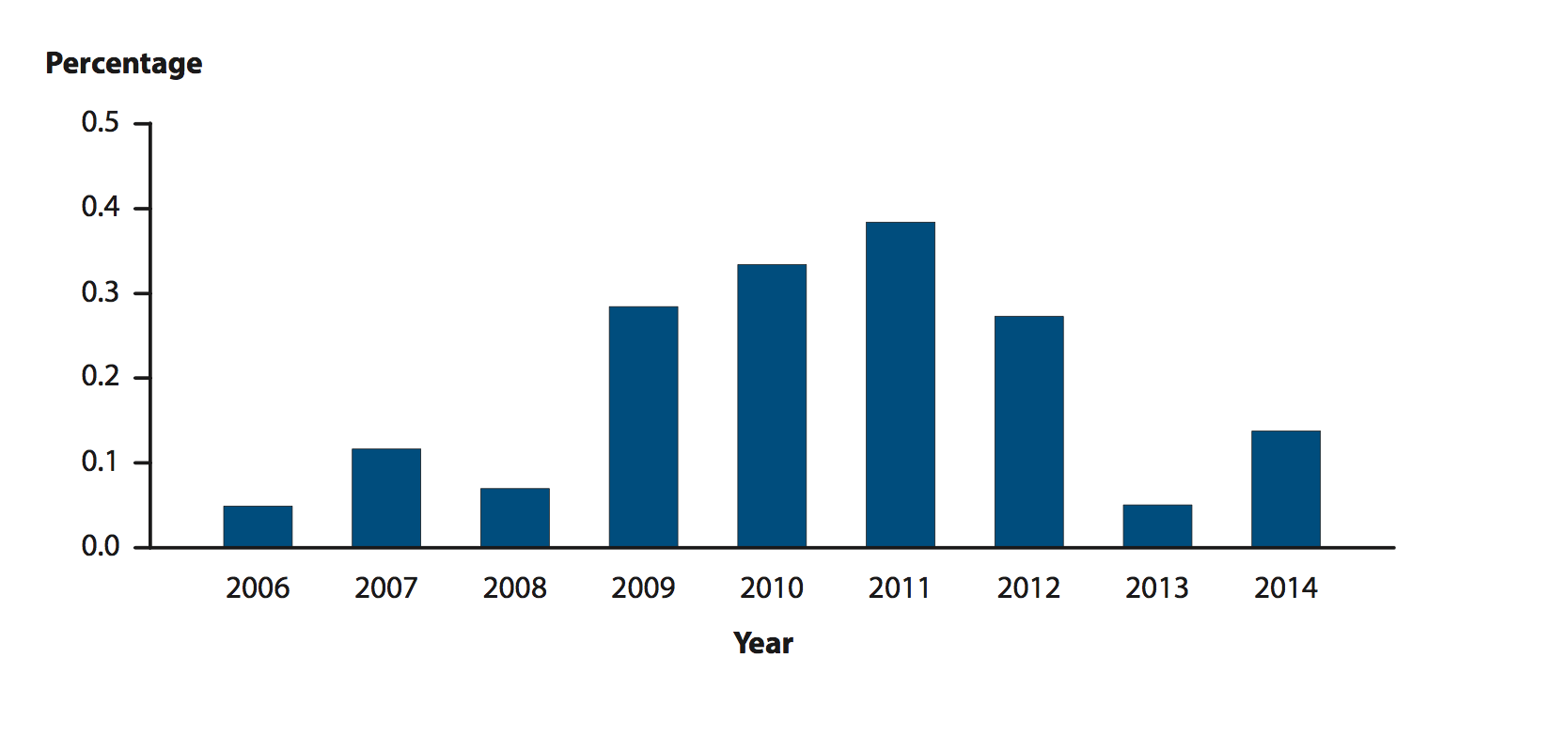
Ceftriaxone Susceptibility
- In 1987, susceptibility testing for ceftriaxone began and continues to date.
- From 2008 to 2011, ceftriaxone Minimum inhibitory concentrations MICs increased from 0.1% to 0.4%.
- Five isolates with decreased ceftriaxone susceptibility (MIC 0.5 lg/ml) include:
- San Diego, California (1987)
- Cincinnati, Ohio (1992 and 1993)
- Philadelphia, Pennsylvania (1997)
- Oklahoma City, Oklahoma (2012)
- From 2006–2012, the prevalence of elevated Ceftriaxone (MICs) was higher in isolates from Men Who have Sex With Men (MSM) than from Men Who have Sex With women (MSW)
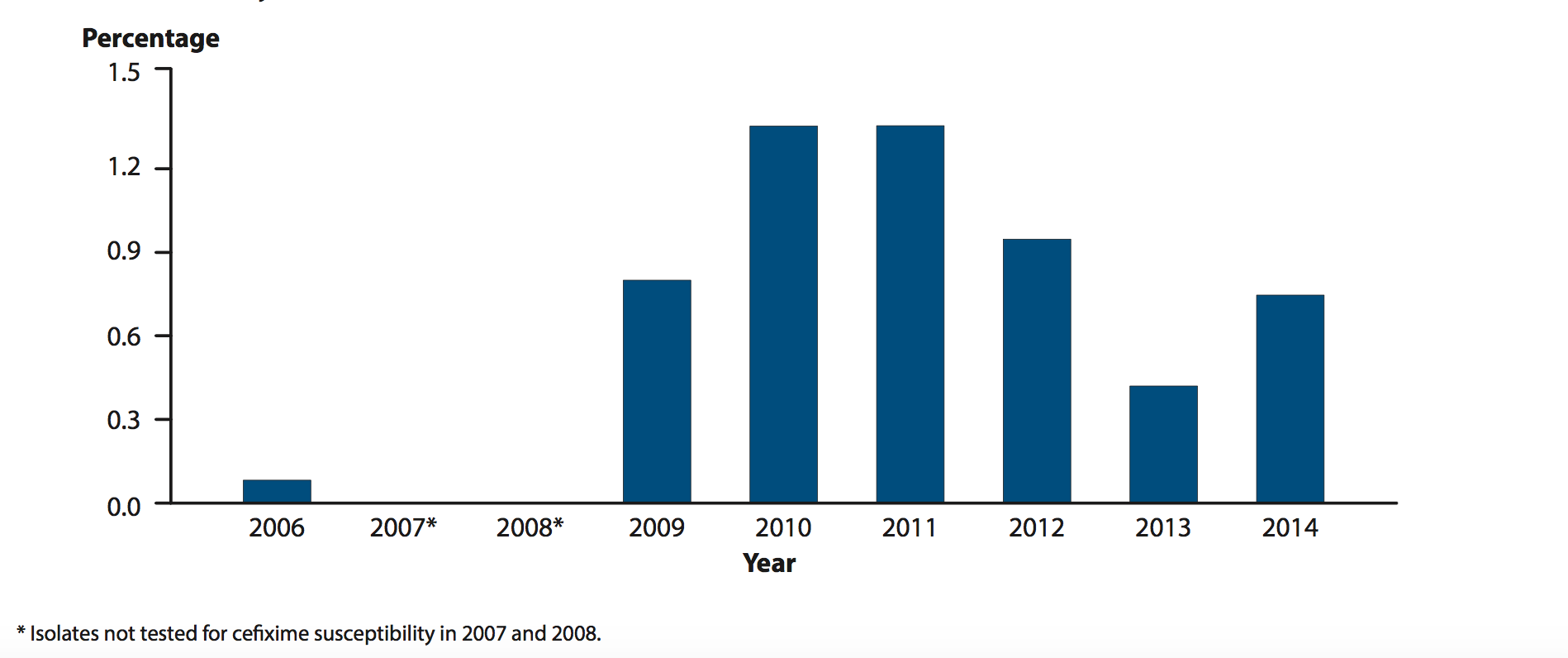
Cefixime Susceptibility
- In 1992, cefixime susceptibility testing began and was discontinued in 2007
- In 2009, cefixime susceptibility testing was restarted due to lack of drug supply in the United States
- From 2006 to 2010, ceftixim Minimum inhibitory concentrations (MICs) increased from 0.1 to 1.4
- from 2006–2012, the prevalence of elevated cefixime (MICs) was higher in isolates from Men Who have Sex With Men (MSM) than from Men Who have Sex With women (MSW)
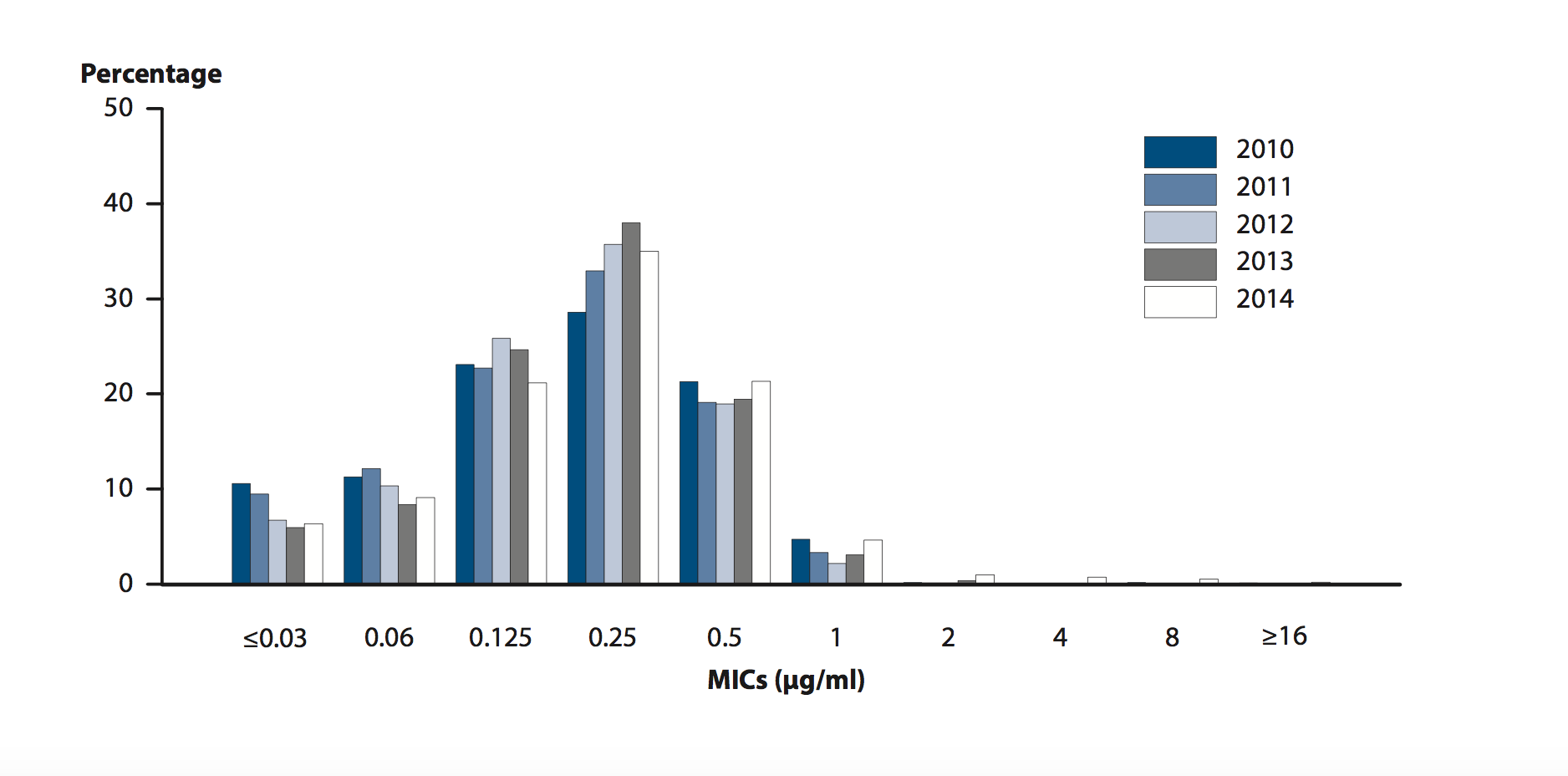
Azithromycin Susceptibility
- In 1992, susceptibility testing for azithromycin began in the United States
- From 2010 to 2013, the percentage of isolates with reduced azithromycin susceptibility (MICs ≥ 2 μg/ml) ranged from 0.3% to 0.6%
- Between 2013 and 2014, the percentage increased from 0.6% to 2.5%
Susceptibility to Other Antimicrobials
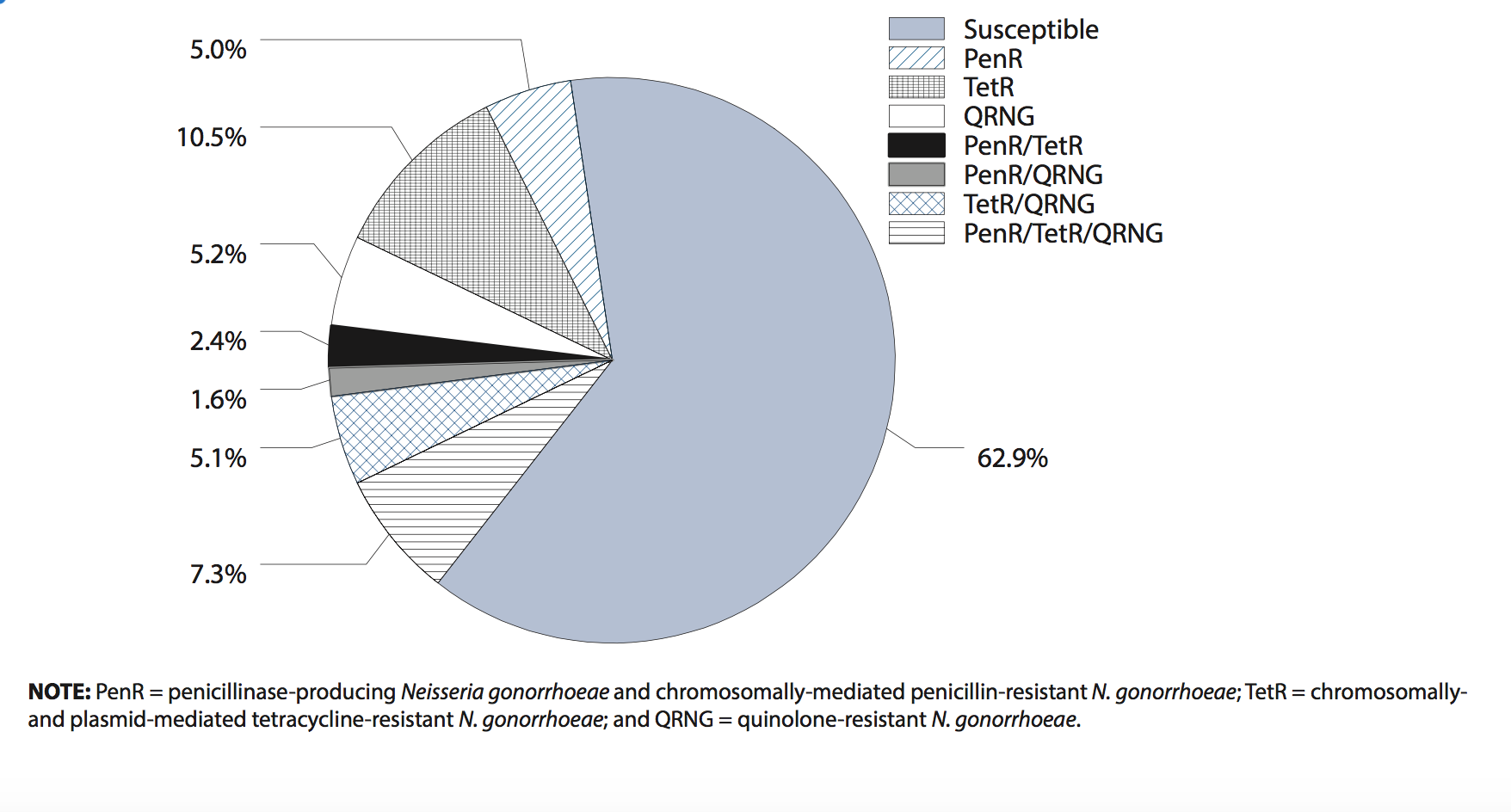
- In 2014, 37.0% of isolates collected from GISP sites were resistant to penicillin, tetracycline, ciprofloxacin, or some combination of those antimicrobials.
References
- ↑ 1.0 1.1 Centers for Disease Control and Prevention. Combating the Threat of Antibiotic-Resistant Gonorrhea. (2016) http://www.cdc.gov/std/gonorrhea/arg/carb.htm Accessed on September 25, 2016
- ↑ GISP, Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2012; gonococcal isolates surveillance project (GISP) supplement and profiles. Atlanta, GA: U.S. Department of Health and Human Services, 2014.https://www.cdc.gov/std/gisp2012/gisp_2012_text_figures_tables_web.pdf
- ↑ Schwarcz SK, Zenilman JM, Schnell D, et al. National surveillance of antimicrobial resistance in Neisseria gonorrhoeae. JAMA 1990;264:1413–7.