22q11.2 deletion syndrome: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 123: | Line 123: | ||
[[Category:Syndromes]] | [[Category:Syndromes]] | ||
[[Category:Immune system disorders]] | [[Category:Immune system disorders]] | ||
[[Category:Needs patient information]] | |||
[[Category:Mature chapter]] | [[Category:Mature chapter]] | ||
Revision as of 22:07, 31 July 2011
| 22q11.2 deletion syndrome | |
| ICD-10 | D82.1 |
|---|---|
| ICD-9 | 279.11, 758.32 |
| OMIM | 188400 |
| DiseasesDB | 3631 |
| MeSH | D004062 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
22q11.2 deletion syndrome, also known as Velocardiofacial Syndrome, Di George Syndrome and Strong Syndrome is a disorder caused by the deletion of a small piece of chromosome 22. The deletion occurs near the middle of the chromosome at a location designated q11.2. It has a prevalence estimated at 1:4000.[1]
Nomenclature
Because the signs and symptoms of 22q11.2 deletion syndrome are so varied, different groupings of features were once described as separate conditions. These included the velo-cardio-facial syndrome (also called Shprintzen's syndrome), DiGeorge syndrome, hearing loss with craniofacial syndromes and conotruncal anomaly face syndrome, thymic hypoplasia, cleft palate, psychiatric disorders, and hypocalcaemia. The acronym CATCH-22 (C = cardiac defects, A = abnormal facies, T = thymic hypoplasia, C = cleft palate, H = hypocalcemia from parathyroid aplasia, 22 = microdeletions in chromosome 22) is sometimes used, although it is widely rejected because of the negative connotations with Catch-22 meaning a 'no-win' situation.
In addition, some children with the 22q11.2 deletion were diagnosed with Opitz G/BBB syndrome and Cayler cardiofacial syndrome. Once the genetic basis for these disorders was identified, doctors determined that they were all part of a single syndrome with many possible signs and symptoms. To avoid confusion, this condition is usually called 22q11.2 deletion syndrome, a description based on its underlying genetic cause.
Etiology
The syndrome is caused by genetic deletions (loss of a small part of the genetic material) found on the long arm of the 22nd chromosome. Some patients with similar clinical features may have deletions on the short arm of chromosome 10.
DiGeorge syndrome causes migration defects of neural crest-derived tissues, particularly affecting development of the third and fourth Branchial pouches (pharyngeal pouches). Also affected is the thymus gland; a mediastinal organ largely responsible for differentiation and induction of tolerance in T-cells. Impaired immune function results principally from this aetiology.
Genetics
Most people with 22q11.2 deletion syndrome are missing about 3 million base pairs (the building blocks of DNA) on one copy of chromosome 22 in each cell. This region contains about 30 genes, but many of these genes have not been well characterized. A small percentage of affected individuals have shorter deletions in the same region. This condition is often described as a contiguous gene deletion syndrome because a deletion in chromosome 22 leads to the loss of many genes.
Researchers have not yet identified all of the genes that contribute to the features of 22q11.2 deletion syndrome. They have determined that the loss of one particular gene on chromosome 22, TBX1, is probably responsible for many of the syndrome's characteristic signs (such as heart defects, a cleft palate, distinctive facial features, and low calcium levels). A loss of this gene does not appear to cause learning disabilities, however. Additional genes in the deleted region are likely to contribute to the signs and symptoms of 22q11.2 deletion syndrome.
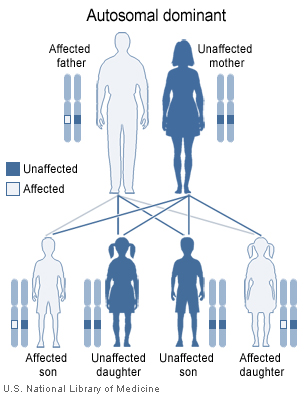
The 22q11.2 deletion syndrome can be inherited in an autosomal dominant manner. Almost all (about 93%) of cases have a de novo (new to the family) deletion of 22q11.2 but about 7% inherit the 22q11.2 deletion from a parent. Children of an individual with deletion 22q11.2 have a 50% chance of inheriting the 22q11.2 deletion. Prenatal testing, such as amniocentesis, is available for pregnancies determined to be at risk. Also pregnancies who have findings of congenital heart disease and/or cleft palate detected by ultrasound examination may be offered prenatal testing. Genetic counseling may be helpful for families who may have DiGeorge syndrome. Because most of the signs of this cluster of defects can also be inherited as autosomal recessive or x-linked traits, only genetic testing of both parents can determine with any certainty the likelihood these anomalies occurring in any subsequent children.
Epidemiology
22q11.2 deletion syndrome affects an estimated 1 in 4000 live births [1]. The condition may be more common, however, because some people with the deletion have few signs and symptoms and may not have been diagnosed.
Presentation
The features of this syndrome vary widely, even among members of the same family, and affect many parts of the body. Characteristic signs and symptoms include heart defects that are often present from birth, an opening in the roof of the mouth (a cleft palate or other defect in the palate), autism, other learning disabilities, mild differences in facial features, and recurrent viral or fungal infections are common due to problems with the immune system's T-cell mediated response. DiGeorge syndrome is often first spotted when the affected newborn begins convulsing from hypocalcemia due to an absence of parathyroid and parathyroid hormone. Affected individuals may also have kidney abnormalities, significant feeding difficulties, autoimmune disorders such as rheumatoid arthritis, and an increased risk of developing mental illnesses.[2] Microdeletions in chromosomal region 22q11 are associated with a roughly 30-fold increased risk of schizophrenia, [3] and are frequently detected in schizophrenic patients. Different studies provide different occurrence rates, ranging from 0.5 to 3%, compared with the overall 0.025% risk of the 22q11 deletion syndrome in the general population.[4]
- ↑ 1.0 1.1 Oskarsdóttir S, Vujic M, Fasth A (2004). "Incidence and prevalence of the 22q11 deletion syndrome: a population-based study in Western Sweden". Arch. Dis. Child. 89 (2): 148–51. PMID 14736631.
- ↑ Debbané M, Glaser B, David MK, Feinstein C, Eliez S (2006). "Psychotic symptoms in children and adolescents with 22q11.2 deletion syndrome: Neuropsychological and behavioral implications". Schizophr. Res. 84 (2–3): 187–93. doi:10.1016/j.schres.2006.01.019. PMID 16545541.
- ↑ Bassett AS, Chow EW, AbdelMalik P, Gheorghiu M, Husted J, Weksberg R (2003). "The schizophrenia phenotype in 22q11 deletion syndrome". Am J Psychiatry. 160 (9): 1580–6. PMID 12944331.
- ↑ Horowitz A, Shifman S, Rivlin N, Pisanté A, Darvasi A (2005). "A survey of the 22q11 microdeletion in a large cohort of schizophrenia patients". Schizophr. Res. 73 (2–3): 263–7. doi:10.1016/j.schres.2004.02.008. PMID 15653270.