Tension pneumothorax resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohamed Moubarak, M.D. [2]; Twinkle Singh, M.B.B.S. [3]
Synonyms and keywords: Collapsed lung; air around the lung; air outside the lung
| Tension Pneumothorax Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Overview
Tension pneumothorax is a medical emergency resulting from the accumulation of air in the pleural cavity. Air enters the intrapleural space as a result of disruption in the parietal pleura, visceral pleura or tracheobronchial tree. This disruption results in the formation of a one way valve which allows the air to enter in the pleural cavity (during inspiration) but prevents its escape (during expiration). Subsequently, pressure inside the pleural cavity rises above the atmospheric pressure and results in respiratory and cardiovascular failure. Tension pneumothorax can occur as a result of trauma, ventilation, resuscitation and preexisting lung disease.[1] Commonly, the patient presents with severe dyspnea and chest pain. It should be managed immediately with emergency needle decompression.
Causes
Life Threatening Causes
Tension pneumothorax is a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
- Asthma
- Central venous catheter
- Cardiopulmonary resuscitation
- Chronic obstructive pulmonary disease
- Emphysema
- Mechanical ventilation
- Trauma
Diagnosis
First Initial Rapid Evaluation of Suspected Tension Pneumothorax
Shown below is an algorithm for the First Initial Rapid Evaluation (FIRE) of suspected tension pneumothorax.[1]
Identify cardinal signs and symptoms that increase the pretest probability of tension pneumothorax | |||||||||||||||||||||||||||||||||||||||||
Identify any alarming signs or symptoms ❑ Jugular venous distension ❑ Tachycardia ❑ Hypotension ❑ Severe dyspnea | |||||||||||||||||||||||||||||||||||||||||
Unstable patient | ❑ Stable patient | ||||||||||||||||||||||||||||||||||||||||
❑ Assess airway, breathing, and circulation | |||||||||||||||||||||||||||||||||||||||||
Proceed with immediate needle decompression in the 2nd intercostal space, midclavicular line of affected hemithorax | |||||||||||||||||||||||||||||||||||||||||
❑ Insert chest drain immediately after needle decompression | |||||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach in Patients with Tension Pneumothorax
Shown below is an algorithm depicting the diagnostic approach of tension pneumothorax based on the British Thoracic Society Pleural Disease Guideline 2010.[1]
Tension pneumothorax requires immediate intervention. It should be diagnosed based on the history and physical examination findings.
Abberviations: DVT: Deep venous thrombosis; CT: Computed tomography
Characterize the symptoms: ❑ Dyspnea | |||||||||||||||||||||||||||
Identify the precipitating factors: ❑ Recent invasive procedures
❑ Mechanical ventilation | |||||||||||||||||||||||||||
Examine the patient: Appearance of the patient Vital signs ❑ Pulse
Skin ❑ Cyanosis Neck ❑ Jugular venous distension (absent in severe hypotension) Respiratory examination: Inspection Additional findings in ventilated patients: ❑ Decreased oxygen saturation | |||||||||||||||||||||||||||
Consider alternative diagnosis:
| |||||||||||||||||||||||||||
| Hemodynamically unstable | Hemodynamically stable | ||||||||||||||||||||||||||
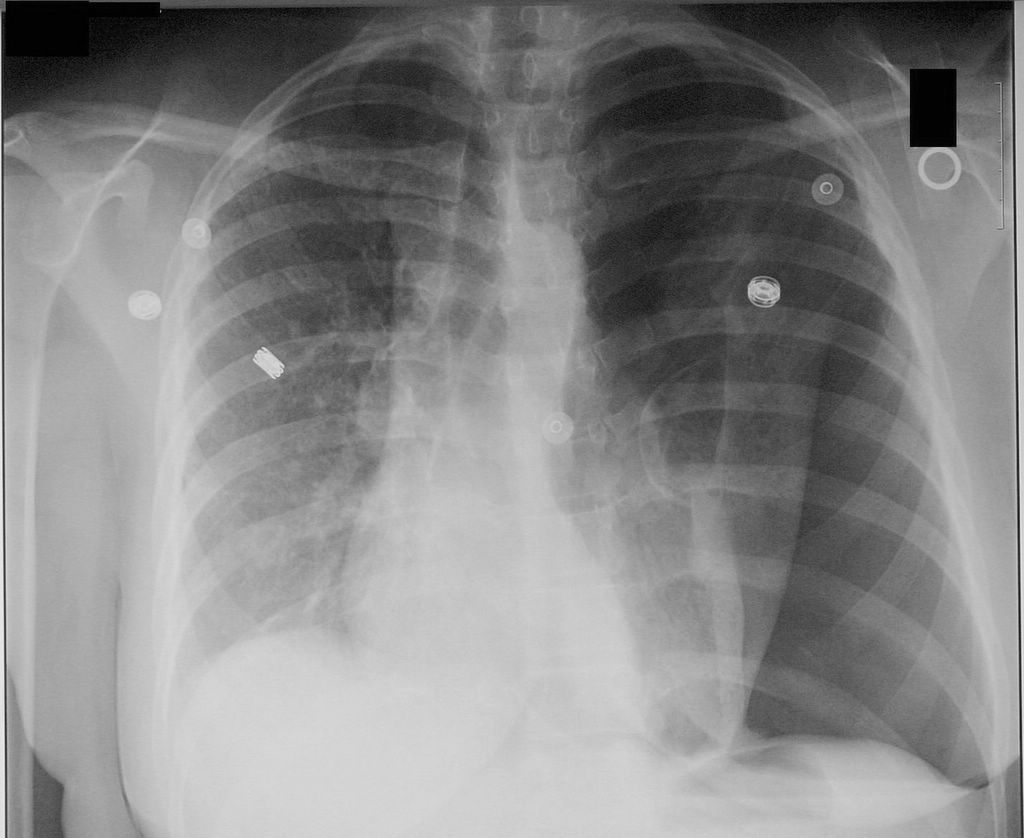
| Proceed with immediate needle decompression | Proceed with imaging studies to confirm the diagnosis in patients who are stable and not in advanced stages of tension
| ||||||||||||||||||||||||||
Treatment
Shown below is an algorithm depicting the treatment approach to tension pneumothorax based on the British Thoracic Society Pleural Disease Guideline 2010.[1]
Perform emergency needle decompression
❑ Ensure aseptic preparation
❑ Use 14-16 gauge intravenous cannula
Don't repeat needle aspiration unless there were technical difficulties. | |||||||||||||||||||||||||||||||||||||
Insert chest drain immediately after needle decompression ❑ Obtain the informed consent
❑ Use a recent chest X-ray to guide the drain insertion
❑ Insert the chest drain | |||||||||||||||||||||||||||||||||||||
Follow up ❑ All patients should be followed up by a chest physician | |||||||||||||||||||||||||||||||||||||
Do's
- Suspect tension pneumothorax with blunt and penetrating trauma to the chest.
- Suspect tension pneumothorax in patients on mechanical ventilation who develop a rapid onset of hemodynamic instability or cardiac arrest and require an increase in the peak inspiratory pressure.
- Order serial chest radiographs every 6 hrs on the first day following chest trauma to rule out pneumothorax.[2]
- Administer adequate analgesia to patients before chest tube insertion, as the procedure is extremely painful.
- Refer the patient to a respiratory specialist within 24 hours of admission.
- Order a chest X-ray before chest tube removal to confirm reexpansion of the affected lung.
Don'ts
- Don't remove the needle from the 2nd intercostal space unless the patient is stable.
- Don't use large bore chest drains.[1]
- Don't leave the chest drain more than 7 days, as it will increase the risk of infection.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group (2010). "Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010". Thorax. 65 Suppl 2: ii18–31. doi:10.1136/thx.2010.136986. PMID 20696690.
- ↑ 2.0 2.1 2.2 Sharma A, Jindal P (2008). "Principles of diagnosis and management of traumatic pneumothorax". J Emerg Trauma Shock. 1 (1): 34–41. doi:10.4103/0974-2700.41789. PMC 2700561. PMID 19561940.