Diabetes mellitus type 1 pathophysiology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Priyamvada Singh, M.B.B.S. [2]; Cafer Zorkun, M.D., Ph.D. [3]
Overview
Pathophysiology
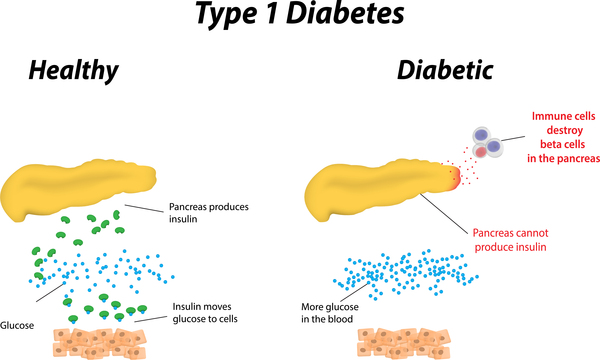
Type 1 diabetes is a disorder characterized by abnormally high blood sugar levels. In this form of diabetes, specialized cells in the pancreas called beta cells stop producing insulin. Insulin controls how much glucose (a type of sugar) is passed from the blood into cells for conversion to energy. Lack of insulin results in the inability to use glucose for energy or to control the amount of sugar in the blood.
Pathogenesis
- Type 1 DM is the result of interactions of genetic, environmental, and immunologic factors that ultimately lead to the destruction of the pancreatic beta cells and insulin deficiency
- Concordance of type 1 DM in identical twins ranges between 40 and 60%, indicating the presence of additional modifying factors.
Genetics
Genes associated with Diabetes mellitus include the following:
- Currently, 58 genomic regions are found to be associated with Type 1 DM.
- Major susceptibility gene for type 1 DM is located on HLA region of chromosome 6. It accounts for 40-50% of the genetic risk for type 1 DM. This region encodes for class II major histocompatibility complex (MHC) molecules. Class II major histocompatibility complex (MHC) molecules play an important role in presenting antigen to helper T cells and initiating immune response.
- Other major susceptibility genes which were associated with Type 1 DM include polymorphisms in the promoter region of the insulin gene, the CTLA-4 gene, interleukin 2 receptor, CTLA4, and PTPN22 etc
- Presence of certain genes confer protection against the development of the disease. Haplotype DQA1*0102, DQB1*0602 is extremely rare in individuals with type 1 DM (<1%) and appears to provide protection from type 1 DM.
Environment
Environmental factors through various pathways were found to influence type 1 DM. Some were found to confer protection against type 1 DM, while others associated with progression and promotion of Type 1 DM, these include :
| Triggers | Protective factors | |
|---|---|---|
| Prenatal triggers |
|
|
| Postnatal triggers |
|
|
| Promoters of progression |
|
Immunological
Several studies have found that abnormalities in the humoral and cellular arm of the immune system, were identified to be associated with Type 1 DM, these include:
- Islet cell autoantibodies
- Activated lymphocytes in the islets, peripancreatic lymph nodes, and systemic circulation
- T lymphocytes that proliferate when stimulated with islet proteins
- Release of cytokines within the insulitis
References
Template:WH Template:WS Template:WH Template:WS