Diabetic foot: Difference between revisions
(→Trauma) |
|||
| Line 36: | Line 36: | ||
Trauma is frequently the trigger of foot [[ulcer]] as repetitive trauma and pressure to the area prevent healing. Excessive plantar pressure is related to limited joint mobility and to foot deformities (Charcot foot, hammer toe). Limited joint mobility and abnormal foot biomechanisms have been associated with an increased risk of ulceration. It could also be the result of poor vision and sensory neuropathy so that the patients does not feel the pain, nor do they see the ulcer. Loss of balance can also make patients more susceptible to falls. <ref name="pmid22529027">{{cite journal| author=Alexiadou K, Doupis J| title=Management of diabetic foot ulcers. | journal=Diabetes Ther | year= 2012 | volume= 3 | issue= 1 | pages= 4 | pmid=22529027 | doi=10.1007/s13300-012-0004-9 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22529027 }} </ref>. | Trauma is frequently the trigger of foot [[ulcer]] as repetitive trauma and pressure to the area prevent healing. Excessive plantar pressure is related to limited joint mobility and to foot deformities (Charcot foot, hammer toe). Limited joint mobility and abnormal foot biomechanisms have been associated with an increased risk of ulceration. It could also be the result of poor vision and sensory neuropathy so that the patients does not feel the pain, nor do they see the ulcer. Loss of balance can also make patients more susceptible to falls. <ref name="pmid22529027">{{cite journal| author=Alexiadou K, Doupis J| title=Management of diabetic foot ulcers. | journal=Diabetes Ther | year= 2012 | volume= 3 | issue= 1 | pages= 4 | pmid=22529027 | doi=10.1007/s13300-012-0004-9 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22529027 }} </ref>. | ||
==Epidemiology and Demographics== | |||
===Incidence=== | |||
It has been reported that annually, about 1 to 4 percent of those with diabetes develop a foot ulcer; 10 to 15 percent of those with diabetes will have at least one foot ulcer during their lifetime<ref name="pmid17280936">{{cite journal| author=Frykberg RG, Zgonis T, Armstrong DG, Driver VR, Giurini JM, Kravitz SR et al.| title=Diabetic foot disorders. A clinical practice guideline (2006 revision). | journal=J Foot Ankle Surg | year= 2006 | volume= 45 | issue= 5 Suppl | pages= S1-66 | pmid=17280936 | doi=10.1016/S1067-2516(07)60001-5 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17280936 }} </ref> | |||
===Gender=== | |||
In 1987, Borch-Johnsen et al. described a male preponderance for the development of severe microvascular complications <ref name="pmid2956021">{{cite journal| author=Borch-Johnsen K, Nissen H, Salling N, Henriksen E, Kreiner S, Deckert T et al.| title=The natural history of insulin-dependent diabetes in Denmark: 2. Long-term survival--who and why. | journal=Diabet Med | year= 1987 | volume= 4 | issue= 3 | pages= 211-6 | pmid=2956021 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2956021 }} </ref>. Diabetic foot disease is not an exception to this rule. For unknown reasons , men have a higher risk of diabetic foot disease compared to women. Some possible explanations are a higher bioavailability of [[nitric oxide]] (NO) bioavailability and NO responsiveness and the protective role of [[estrogen]] in women <ref name="pmid12538427">{{cite journal| author=Gladwin MT, Schechter AN, Ognibene FP, Coles WA, Reiter CD, Schenke WH et al.| title=Divergent nitric oxide bioavailability in men and women with sickle cell disease. | journal=Circulation | year= 2003 | volume= 107 | issue= 2 | pages= 271-8 | pmid=12538427 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12538427 }} </ref>. However the beneficial effect of these factors are reversed by [[diabetes]], irrespective of menopausal status.Nevertheless men still have a higher risk for having diabetic foot disease . | |||
==Diabetic Foot Physical Examination== | ==Diabetic Foot Physical Examination== | ||
Revision as of 20:16, 22 February 2013
|
Diabetes mellitus Main page |
|
Patient Information |
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Priyamvada Singh, M.B.B.S. [2]; Cafer Zorkun, M.D., Ph.D. [3]
Overview
Type 2 diabetes and its complications are now considered as a growing health threat. It is the leading cause of blindness, end stage renal disease, coronary heart disease and foot ulceration which leads to amputations. In general, the incidence of nontraumatic lower extremity amputations has been reported to be at least 15 times greater in those with diabetes than with any other medical illness. Among patients with diabetes, the lifetime risk of having foot ulcer is 15%. Diabetic foot ulcers dramatically worsen the physical, psychological and social quality of life [1]. 1 in every 4 patients with diabetes develops complications. The pathogenesis of diabetics foot is due to two causes i.e. neuropathy and vasculopathy. Due to neuropathy the patient loses sensation whereas, vasculopathy causes poor blood supply to the foot region. Due to both these contributing factors, even a small trauma to the feet can give rise to ulcer or gangrene and may even require amputation. Thus, foot examination by a podiatrist or a doctor is recommended every year.
Pathophysiology
Diabetic foot is an umbrella term for foot problems in patients with diabetes mellitus. Due to arterial abnormalities and diabetic neuropathy and delayed wound healing, infection or gangrene of the foot is relatively common. The key components of diabetic foot are neuropathy, angiopathy and trauma [1].
Neuropathy
The most important cause of diabetic foot is neuropathy. This is present to some extent in more than half of the patients with diabetes older than 60 years old. Peripheral neuropathy usually is profound at the point where it leads to the formation of a foot ulcer. What causes neuropathy and why it occurs is not fully known. It is most likely caused by a combination of factors such as; high blood glucose, reactive oxygen species, vasculopathy, reduced oxygenation of the nerves, inflammation, autoimmunity in diabetes, genetic factors, mechanical injury, smoking and alcohol abuse.
Generalized symmetric distal polyneuropathy is the most common and widely recognized form of diabetic neuropathy leading to diabetic foot ulcer. It may be either sensory or motor, and involves small fibers, large fibers or both. The clinical manifestations are divided into the three types of sensory, motor and autonomic neuropathy. Motor neuropathy causes wasting of small muscles of the feet with hammer toes and weakness of hands and feet.
Sensory neuropathy causes:
- Impaired vibration perception and position sense
- Depressed tendon reflexes
- Dull, crushing or cramp-like pain in the bones of the feet,
- Sensory ataxia
- Shortening of the achilles tendon
- Abnormal thresholds for warm thermal perception
- Decreased neurovascular function
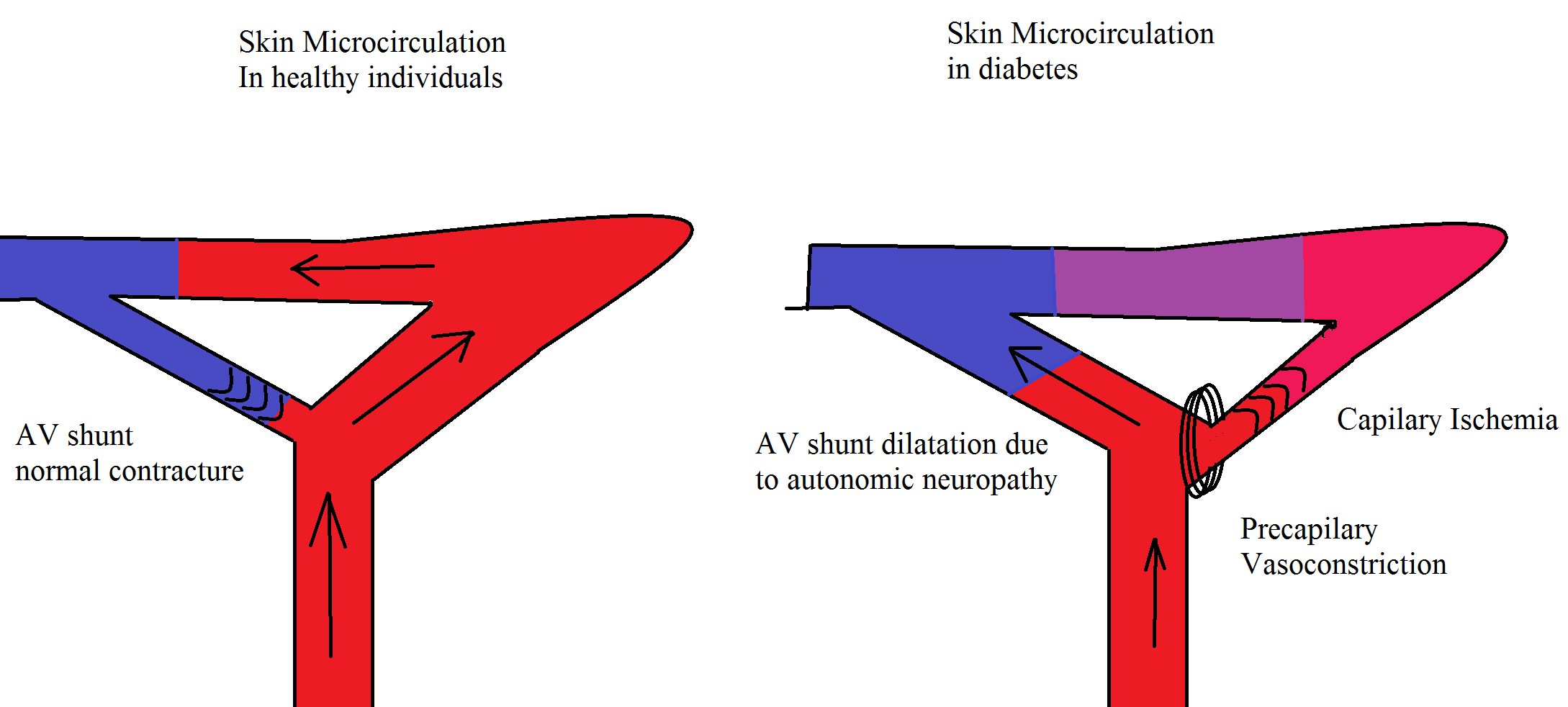
Autonomic neuropathy is the increased or decreased blood flow to the foot (hot foot) with an increased risk of charcot neuroarthropathy, decreased sweating, dry skin, impaired vasomotion and blood flow. These lead to cold feet which ultimately result into the loss of skin integrity, providing a vulnerable site for infection [2].
Angiopathy
Micro and macrovascular complications are the leading cause of diabetic complications. Atherosclerosis occurs due to inflammation, which leads to the accumulation of foam cells. The vascular changes which are responsible for foot problems include stiff arteries due to calcification of the smooth muscle cells in the arterial wall (mediasclerosis). It is usually discovered by an impaired ankle brachial index (ABI). The resting ABI is the ratio of the blood pressure in the lower legs to the blood pressure in the arms. The ABI is calculated by dividing the systolic blood pressure at the ankle by the systolic blood pressures in the arm. It is a non-invasive method to assess the lower extremity arterial system and to detect the presence of arterial occlusion disease. In severe cases, it leads to ischemic foot problems, which the only treatment is vascular surgery. Even in neuropathic foot ulcers, the non healing wounds are the result of impaired blood supply to the tissue. Decreasing the central blood pressure by antihypertensive drugs may be deleterious for these patients[2]. Microvascular complications cause skin damage, infection and impaired wound healing. Once a foot ulcer develops, peripheral vascular disease is the most important factor which may contribute to adverse outcomes.Vascular complications are like a positive feedback which worsen the skin and nerve damage in diabetes [3]
Trauma
Trauma is frequently the trigger of foot ulcer as repetitive trauma and pressure to the area prevent healing. Excessive plantar pressure is related to limited joint mobility and to foot deformities (Charcot foot, hammer toe). Limited joint mobility and abnormal foot biomechanisms have been associated with an increased risk of ulceration. It could also be the result of poor vision and sensory neuropathy so that the patients does not feel the pain, nor do they see the ulcer. Loss of balance can also make patients more susceptible to falls. [2].
Epidemiology and Demographics
Incidence
It has been reported that annually, about 1 to 4 percent of those with diabetes develop a foot ulcer; 10 to 15 percent of those with diabetes will have at least one foot ulcer during their lifetime[4]
Gender
In 1987, Borch-Johnsen et al. described a male preponderance for the development of severe microvascular complications [5]. Diabetic foot disease is not an exception to this rule. For unknown reasons , men have a higher risk of diabetic foot disease compared to women. Some possible explanations are a higher bioavailability of nitric oxide (NO) bioavailability and NO responsiveness and the protective role of estrogen in women [6]. However the beneficial effect of these factors are reversed by diabetes, irrespective of menopausal status.Nevertheless men still have a higher risk for having diabetic foot disease .
Diabetic Foot Physical Examination
Inspection
- Dilated veins
- Scar, Sinuses
- Shiny skin
- Hair distribution
- Areas of Pigmentation
- Areas of discolouration
- Varicose vein
- Ulcers
- Brittle or broken nail
- Fungal infection
Palpation
- Temperature (increase temperature- deep vein thrombosis, decrease temperature-ischemia)
- Tenderness (squeeze calf muscle and achilles tendon for tenderness)
- Pulsation- Dorsalis pedis
- Capillary filling time
- Ulcers in pressure areas like ball of great toe, base of fifth metatarsal, posterior aspect of heel
Motor Examination
- Nutrition/Bulk
- Tone
- Power
- Reflexes
Sensory
- Vibration
- Joint position sense
Video: Physical Examination Diabetes
{{#ev:youtube|715j6zRZHaA}}
Video: Diabetic Foot Care
{{#ev:youtube|DASvmFJeYX8}}
Image: Diabetic Foot Ulcer

References
- ↑ 1.0 1.1 Assal JP, Mehnert H, Tritschler HJ, Sidorenko A, Keen H, Hellmut Mehnert Award Workshop Participants (2002). "On your feet! Workshop on the diabetic foot". J Diabetes Complications. 16 (2): 183–94. PMID 12039404.
- ↑ 2.0 2.1 2.2 Alexiadou K, Doupis J (2012). "Management of diabetic foot ulcers". Diabetes Ther. 3 (1): 4. doi:10.1007/s13300-012-0004-9. PMID 22529027.
- ↑ Venermo M, Vikatmaa P, Terasaki H, Sugano N (2012). "Vascular laboratory for critical limb ischaemia". Scand J Surg. 101 (2): 86–93. PMID 22623440.
- ↑ Frykberg RG, Zgonis T, Armstrong DG, Driver VR, Giurini JM, Kravitz SR; et al. (2006). "Diabetic foot disorders. A clinical practice guideline (2006 revision)". J Foot Ankle Surg. 45 (5 Suppl): S1–66. doi:10.1016/S1067-2516(07)60001-5. PMID 17280936.
- ↑ Borch-Johnsen K, Nissen H, Salling N, Henriksen E, Kreiner S, Deckert T; et al. (1987). "The natural history of insulin-dependent diabetes in Denmark: 2. Long-term survival--who and why". Diabet Med. 4 (3): 211–6. PMID 2956021.
- ↑ Gladwin MT, Schechter AN, Ognibene FP, Coles WA, Reiter CD, Schenke WH; et al. (2003). "Divergent nitric oxide bioavailability in men and women with sickle cell disease". Circulation. 107 (2): 271–8. PMID 12538427.