Osteoid osteoma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
'''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | ||
<br>'''For more information about osteoma that is not associated with osteoid osteoma, see [[osteoma]]''' | <br>'''For more information about osteoma that is not associated with osteoid osteoma, see [[osteoma]]''' | ||
| Line 7: | Line 6: | ||
{{SK}} Osteoma osteoid; OO; Osteoid osteomas | {{SK}} Osteoma osteoid; OO; Osteoid osteomas | ||
==Overview== | ==Overview== | ||
Revision as of 20:34, 18 December 2018
For patient information click here
For more information about osteoma that is not associated with osteoid osteoma, see osteoma
|
WikiDoc Resources for Osteoid osteoma |
|
Articles |
|---|
|
Most recent articles on Osteoid osteoma Most cited articles on Osteoid osteoma |
|
Media |
|
Powerpoint slides on Osteoid osteoma |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Osteoid osteoma at Clinical Trials.gov Trial results on Osteoid osteoma Clinical Trials on Osteoid osteoma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Osteoid osteoma NICE Guidance on Osteoid osteoma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Osteoid osteoma Discussion groups on Osteoid osteoma Patient Handouts on Osteoid osteoma Directions to Hospitals Treating Osteoid osteoma Risk calculators and risk factors for Osteoid osteoma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Osteoid osteoma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rohan A. Bhimani, M.B.B.S., D.N.B., M.Ch.[2]
Synonyms and keywords: Osteoma osteoid; OO; Osteoid osteomas
Overview
Osteoid osteoma is the third most common benign bone tumor. Its incidence is 11% among the benign tumors and 3% among all primary bone tumors. Adolescents and children are most affected by osteoid osteoma. Men are more commonly affected than women, with a 6:4 ratio. Osteoid osteoma is a benign osteoblastic tumor that was first described in 1930 by Bergstrand. Jaffe described it in 1935 and was the first to recognize it as a unique entity. Osteoid osteomas are usually smaller than 1.5-2 cm and characterized by an osteoid-rich nidus in a highly loose, vascular connective tissue. The nidus is well demarcated and may contain a variable amount of calcification. Surrounding the nidus is a zone of sclerotic but otherwise normal bone. Osteoid osteoma can occur anywhere. Osteoid osteoma is usually occur in the cortex of the shafts of long bones more than 50% of the cases. It is seen in the metadiphyseal regions of large bones of the femur, tibia, and humerus. About 20% percent of the lesions involve posterior element of the spine. The hallmark of osteoid osteoma is intense nocturnal limb pain which is relieved by low doses of salicylates and local tenderness. If left untreated, osteoid osteoma progression occurs slow and is then followed by restricted range of motion, possible pathologic fracture, or spontaneous regression. The medical therapy for osteoid osteoma is NSAIDs and the mainstay of treatment is surgery.
The lower extremities are the most common sites of osteoid osteomas. The femur, particularly the intertrochanteric or intracapsular regions of the hip, is affected in two thirds of cases.
Historical Perspective
- In 1930, Dr. Bergstrand, a German physician, first described osteoid osteoma in 1930.[1]
- In 1935, Dr.Henry Jaffe, an American pathologist first described osteoid osteoma as a benign bone tumor.[2]
- In 1953, Dr. Jaffe coined the term nidus, which was described as the “core”, referring to the tumor itself and is composed of bone at various stages of maturity within a highly vascular connective tissue stroma.[3]
- In 1954, Dahlin and Johnson added the term giant osteoid osteomas.[4]
- In 1966, Dr.Edeiken classifed osteoid osteomas into three types.[2]
Classification
- Osteoid Osteoma can be classified based on location and imaging findings.
Anatomical Classification
| Type of osteoid osteoma | Characteristics |
|---|---|
| Intracortical | Dense sclerosis around the nidus |
| Periosteal | Periosteal reaction |
| Cancellous (medullary) | Produces very little reactive bone |
| Subarticular | Simulates arthritis as it produces synovial reactions |
Enneking (MSTS) Staging System
- The Enneking surgical staging system (also known as the MSTS system) for benign musculoskeletal tumors based on radiographic characteristics of the tumor host margin.[7]
- It is widely accepted and routinely used classification.
| Stages | Description |
|---|---|
| 1 | Latent: Well demarcated borders |
| 2 | Active: Indistinct borders |
| 3 | Aggressive: Indistinct borders |
Pathophysiology
- The exact etiology of osteoid osteoma is unknown.[8]
- Osteoid osteoma arises from the osteoblasts.
- Osteoid osteoma consists of radially oriented trabeculae of surrounding reactive bone, indicating an increased pressure in the vascular nidus.
- This arrangement of the bony trabeculae is due to the stresses placed on them.
- This increased pressure is due to vasodilatation and edema is which stimulate intraosseous nerve endings, generating pain.[9]
- In addiition, the pain is also attributed to increased local concentration of prostaglandin E2, COX1 & 2 expression; and increased number and size of unmyelinated nerve fibers within the nidus.
- Osteoid osteomas are usually cortical lesions but they can occur anywhere within the bone including medullary, subperiosteal (most common in talus), and intracapsular area.
- More than 50 percent of osteoid osteomas occur in lower extremity of long bones.[2][10]
- It most commonly affects the metadiaphysis of the femur and tibia.
- About 20 percent of osteoid osteomas occur in the posterior elements of the spine.
Genetics
- The structural chromosomal alterations involving 22q13.1 in osteoid osteoma may affect critical genes involved in the regulation of cell proliferation, such as the YWHAH gene.[11]
- YWHAH gene codes for a 14-3-3 family members of dimeric phosphoserine-binding proteins that participate in signal transduction and checkpoint control pathways.
- Their primary function is to inhibit apoptosis.
- Another gene mapped in this region is PDGFB that codes for a platelet-derived growth factor, a beta polypeptide (simian sarcoma viral [v-sis] oncogene homolog), a potent mitogen for cells of mesenchymal origin and involved in the transformation process.
Causes
- The cause of osteoid osteoma has not been identified.[12]
Differentiating ((Page name)) from Other Diseases
- Osteoid osteoma must be differentiated from other diseases that cause night-pain, soft tissue swelling, and bowing deformity such as other osteogenic tumors, osteoblastoma, bone abscess (Brodie abscess), osteosarcoma, and enostosis.[13][14]
| Differential Diagnosis | Similar Features | Differentiating Features |
|---|---|---|
| Osteoblastoma |
|
|
| Brodie abscess |
|
|
| Osteosarcoma |
|
|
| Enostosis |
|
|
Epidemiology and Demographics
- Osteoid osteoma is the third most common benign bone tumor.[15][16]
- Its incidence is 11% among the benign tumors and 3% among all primary bone tumors.[17]
- Adolescents and children are most affected by osteoid osteoma.
- The age distribution of osteoid osteoma is between 5-22 years.[18]
- The mean age of the patients with osteoid osteoma is 12 years (range, 8-35 years).[18]
- Men are more commonly affected than women, with a 6:4 ratio.[18]
- There is no racial predilection to osteoid osteoma.
Risk Factors
There are no established risk factors for osteoid osteoma.[19]
Screening
- There is insufficient evidence to recommend routine screening for osteoid osteoma.
Natural History, Complications, and Prognosis
- The natural history of untreated osteoid osteoma is toward spontaneous regression, it is taken an average of 6 years.[20]
- During this period, the nidus gradually begins to calcify; afterwards, ossify, and, finally, blends into sclerotic surrounding bone.
- The local pain gradually diminishes over time.
- Common complications of osteoid osteoma includes pathological fracture, stress fracture, and muscle atrophy.
- Prognosis is generally excellent after surgery.
- Local recurrence is rare but may occur 6 months after surgery.
Diagnosis
Diagnostic Study of Choice
- CT scan is the diagnostic study of choice for the diagnosis of osteoid osteoma.
- CT findings include:[21]
- Sharp round lesion which is less than 2 cm in diameter.
- Osteoid osteoma has a homogeneous dense center.
- Sclerotic reactive bone surrounding the nidus is seen.
- A 1.5 mm peripheral radiolucent zone is seen.
- Furthermore, a central sclerotic is noted.
History and Symptoms
- The majority of patients with osteoid osteoma have localized pain that worsens at night.[22]
- The pain is relieved by salicylates.
- Swelling
- Intra-articular lesions present with:
- Limb deformity
- Abnormal gait
- Lesions invloving spine present as back pain.
Physical Examination
- Patients with osteoid osteoma usually appears well.
- Common physical examination findings of osteoblastoma include:[23]
- Palpable bone deformity
- swelling
- Erythema
- Tenderness
- If the lesion is in proximity to a joint, findings include:
- Effusion
- Contracture
- Abnormal gait
- Muscle atrophy
- If the lesion involves spine, findings include:
- Postural scoliosis
- Paravertebral muscle spasm
Laboratory Findings
- There are no diagnostic laboratory findings associated with osteoid osteoma.
 |
Electrocardiogram
- There are no ECG findings associated with osteoid osteoma.
X-ray
- Three views of affected bone or joint are recommended.[24]
- Radiological findings for osteoid osteoma include:
- Intensely reactive bone
- Radiolucent nidus
Echocardiography or Ultrasound
Ultrasound findings associated with osteoid osteoma, include:[25]
- Focal cortical irregularity
- Adjacent hypoechoic synovitis
- Hypoechogenecity with posterior acoustic enhancement
- On Doppler ultrasound, osteoid osteoma may appear as a hypervascular nidus.
CT scan
 |
- CT scan is the study of choice for the diagnosis of osteoid osteoma.
- CT findings include:[26]
- Sharp round lesion which is less than 2 cm in diameter.
- Osteoid osteoma has a homogeneous dense center.
- Sclerotic reactive bone surrounding the nidus is seen.
- A 1.5 mm peripheral radiolucent zone is seen.
- Furthermore, a central sclerotic is noted.
MRI
MRI is usually not recommended as it can mimic aggressive lesions.
Other Imaging Findings
Radionuclide Scanning
- Radionuclide scans are reliable tools when radiographic findings are not diagnostic.[27][28][29]
- Bone scan findings include:
- Intense hot area of focal uptake at the nidus.
- Low uptake in reactive zone known as the double-density sign.
Other Diagnostic Studies
 |
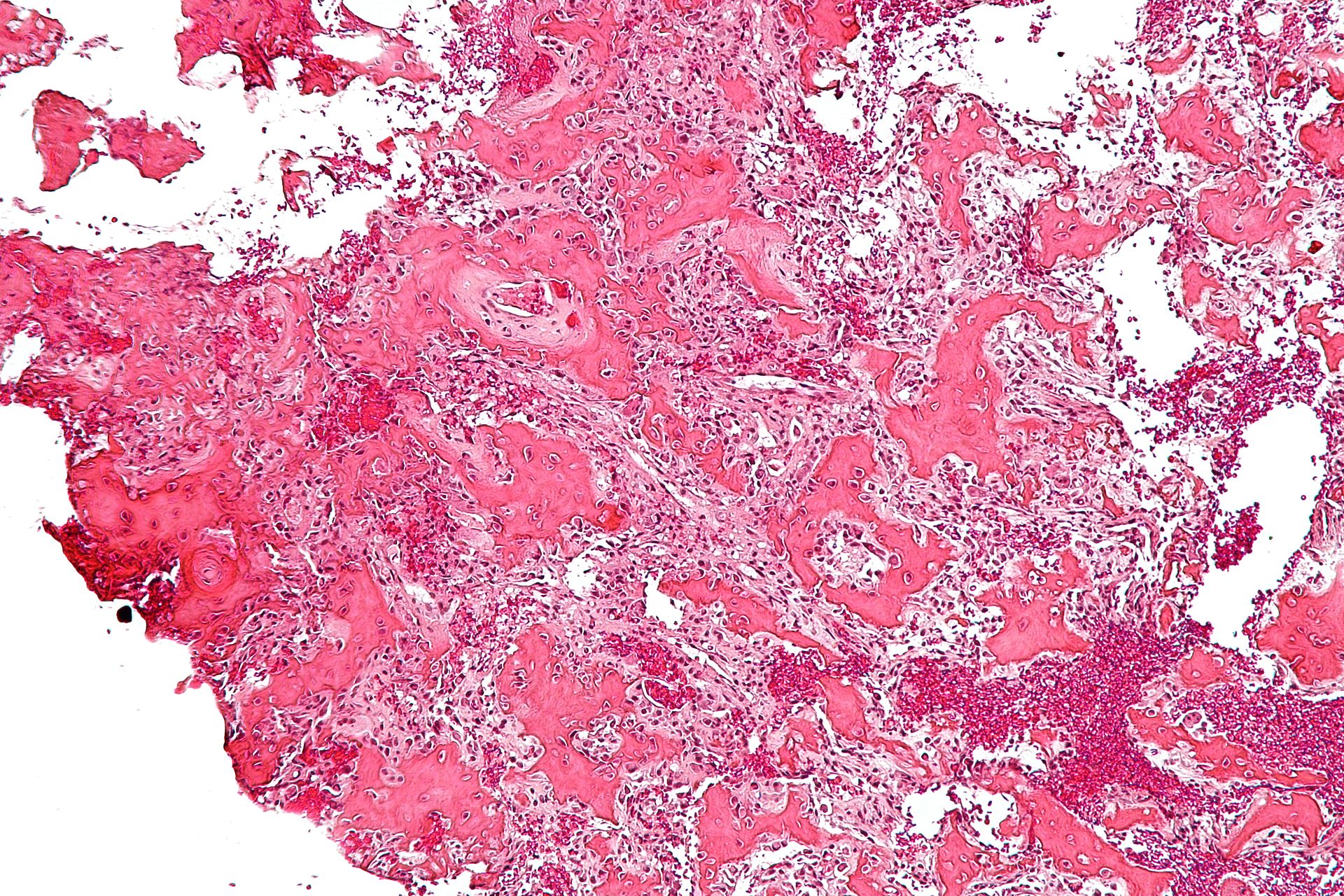 |
Biopsy
- Biopsy may be helpful in the diagnosis of osteoid osteoma.
- Biopsy demonstrates the following features:
- Nidus usually about 1.5-2cms, brownish-red, mottled, and gritty lesion that is distinct from the surrounding bone.
- Network of interconnecting bone, widened vessels, osteoblasts, and bone matrix
- Fibrinoid margin with areas of angiogenesis
- Adjacent sclerosis
- On histological examination:
- Osteoid and woven bone lined with osteoblasts and richly innervated with surrounding hypervascular connective tissue with osteoclasts is seen.
- Osteoid osteoma do not malignantly transform.
Treatment
Medical Therapy
- Clinical observation and NSAID administration.[6][30]
- NSAIDs are 1st line and will lead to a dramatic decrease in symptoms.
- About 50% of the patients can be treated with NSAIDs alone.
- NSAIDs are also indicated for painful spine lesions without scoliosis.
- The natural course of osteoid osteomas is spontaneous regression. However, NSAIDs may accelerate this process.[31][32][31]
- Fingertip lesions (distal phalanx) may not respond to NSAIDs.
Surgery
Surgery is the mainstay of treatment for [disease or malignancy].[6][33][6][31]
Percutaneous Radiofrequency Ablation (RFA)
Indications
- Failure of medical management
- Periarticular lesions which increase the risk of cartilage injury and premature degenerative disease.
- Spinal lesions depending on the location of the lesion and proximity to neural elements
Contraindications
- Lesions close to spinal cord or nerve roots
Technique
- It is done under CT guidance
- Probing is done at 80-90 deg C for 6 minutes to produce a 1cm zone of necrosis
Outcomes
- 90% of patients are successfully treated with 1-2 sessions of RFA.
- 10-15% recurrence rate.
Surgical Resection with Currettage
Indications
- When loocation of lesion is not amenable to CT guided percutaneous radiofrequency ablation such as close to skin or nerve.
- Spine lesion associated with painful scoliosis
- Digital lesions because RFA carries risk of thermal skin necrosis and injury to digital neurovascular bundle.
Technique
- Successful treatment depends on complete marginal resection of nidus.
- Sclerotic bone is normal and can be left behind.
- It can be done by:
- Percutaneous approach
- Open approach
Outcomes
- 94% success with local excision
Primary Prevention
There are no established measures for the primary prevention of osteoid osteoma.
Secondary Prevention
There are no established measures for the secondary prevention of osteoid osteoma.
References
- ↑ Karandikar S, Thakur G, Tijare M, Shreenivas K, Agrawal K (2011). "Osteoid osteoma of mandible". BMJ Case Rep. 2011. doi:10.1136/bcr.10.2011.4886. PMC 3233922. PMID 22669768.
- ↑ 2.0 2.1 2.2 Torg JS, Loughran T, Pavlov H, Schwamm H, Gregg J, Sherman M, Balduini FC (1985). "Osteoid osteoma. Distant, periarticular, and subarticular lesions as a cause of knee pain". Sports Med. 2 (4): 296–304. PMID 3849059.
- ↑ Chai JW, Hong SH, Choi JY, Koh YH, Lee JW, Choi JA; et al. (2010). "Radiologic diagnosis of osteoid osteoma: from simple to challenging findings". Radiographics. 30 (3): 737–49. doi:10.1148/rg.303095120. PMID 20462991.
- ↑ DAHLIN DC, JOHNSON EW (1954). "Giant osteoid osteoma". J Bone Joint Surg Am. 36-A (3): 559–72. PMID 13163088.
- ↑ Morton KS, Vassar PS, Knickerbocker WJ (1975). "Osteoid osteoma and osteoblastoma: reclassification of 43 cases using Schajowicz's classification". Can J Surg. 18 (2): 148–52. PMID 1116053.
- ↑ 6.0 6.1 6.2 6.3 Hakim DN, Pelly T, Kulendran M, Caris JA (2015). "Benign tumours of the bone: A review". J Bone Oncol. 4 (2): 37–41. doi:10.1016/j.jbo.2015.02.001. PMC 4620948. PMID 26579486.
- ↑ Jawad MU, Scully SP (2010). "In brief: classifications in brief: enneking classification: benign and malignant tumors of the musculoskeletal system". Clin Orthop Relat Res. 468 (7): 2000–2. doi:10.1007/s11999-010-1315-7. PMC 2882012. PMID 20333492.
- ↑ Athwal P, Stock H (2014). "Osteoid osteoma: a pictorial review". Conn Med. 78 (4): 233–5. PMID 24830123.
- ↑ O'Connell JX, Nanthakumar SS, Nielsen GP, Rosenberg AE (1998). "Osteoid osteoma: the uniquely innervated bone tumor". Mod. Pathol. 11 (2): 175–80. PMID 9504688.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ Baruffi MR, Volpon JB, Neto JB, Casartelli C (2001). "Osteoid osteomas with chromosome alterations involving 22q". Cancer Genet Cytogenet. 124 (2): 127–31. PMID 11172903.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ Hashemi J, Gharahdaghi M, Ansaripour E, Jedi F, Hashemi S (2011). "Radiological features of osteoid osteoma: pictorial review". Iran J Radiol. 8 (3): 182–9. doi:10.5812/kmp.iranjradiol.17351065.3392. PMC 3522328. PMID 23329939.
- ↑ Atesok KI, Alman BA, Schemitsch EH, Peyser A, Mankin H (2011). "Osteoid osteoma and osteoblastoma". J Am Acad Orthop Surg. 19 (11): 678–89. PMID 22052644.
- ↑ Lee EH, Shafi M, Hui JH (2006). "Osteoid osteoma: a current review". J Pediatr Orthop. 26 (5): 695–700. doi:10.1097/01.bpo.0000233807.80046.7c. PMID 16932114.
- ↑ Kalil RK, Antunes JS (2003). "Familial occurrence of osteoid osteoma". Skeletal Radiol. 32 (7): 416–9. doi:10.1007/s00256-003-0660-y. PMID 12802523.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ 18.0 18.1 18.2 Barlow E, Davies AM, Cool WP, Barlow D, Mangham DC (2013). "Osteoid osteoma and osteoblastoma: novel histological and immunohistochemical observations as evidence for a single entity". J Clin Pathol. 66 (9): 768–74. doi:10.1136/jclinpath-2013-201492. PMID 23814261.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ Rand JA, Sim FH, Unni KK (1982). "Two osteoid-osteomas in one patient. A case report". J Bone Joint Surg Am. 64 (8): 1243. PMID 7130236.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ Greenspan A (1993). "Benign bone-forming lesions: osteoma, osteoid osteoma, and osteoblastoma. Clinical, imaging, pathologic, and differential considerations". Skeletal Radiol. 22 (7): 485–500. PMID 8272884.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ Meire E, Hoogmartens M, De Roo M, Mortelmans L, Nicolai D (1983). "The peroperative use of the mobile gamma camera for the localization of spinal osteoid osteoma". Acta Orthop Belg. 49 (3): 384–90. PMID 6224390.
- ↑ Rinsky LA, Goris M, Bleck EE, Halpern A, Hirshman P (1980). "Intraoperative skeletal scintigraphy for localization of osteoid-osteoma in the spine. Case report". J Bone Joint Surg Am. 62 (1): 143–4. PMID 7351408.
- ↑ Swee RG, McLeod RA, Beabout JW (1979). "Osteoid osteoma. Detection, diagnosis, and localization". Radiology. 130 (1): 117–23. doi:10.1148/130.1.117. PMID 758639.
- ↑ Gangi A. [The treatment of osteoid osteoma: a multitude of choice: surgery, percutaneous resection, alcohol injection or thermocoagulation]. J Radiol 1999; 80:419-420
- ↑ 31.0 31.1 31.2 Iyer RS, Chapman T, Chew FS (2012). "Pediatric bone imaging: diagnostic imaging of osteoid osteoma". AJR Am J Roentgenol. 198 (5): 1039–52. doi:10.2214/AJR.10.7313. PMID 22528893.
- ↑ Goto T, Shinoda Y, Okuma T, Ogura K, Tsuda Y, Yamakawa K, Hozumi T (2011). "Administration of nonsteroidal anti-inflammatory drugs accelerates spontaneous healing of osteoid osteoma". Arch Orthop Trauma Surg. 131 (5): 619–25. doi:10.1007/s00402-010-1179-z. PMID 20737157.
- ↑ Gangi A. [The treatment of osteoid osteoma: a multitude of choice: surgery, percutaneous resection, alcohol injection or thermocoagulation]. J Radiol 1999; 80:419-420