Hemolytic anemia laboratory findings: Difference between revisions
Shyam Patel (talk | contribs) No edit summary |
Shyam Patel (talk | contribs) No edit summary |
||
| Line 7: | Line 7: | ||
==Approach to diagnosis of hemolytic anemia== | ==Approach to diagnosis of hemolytic anemia== | ||
===Peripheral smear=== | ===Peripheral smear=== | ||
Findings on peripheral smears can guide towards diagnosis. Some important findings are: | Findings on peripheral smears can guide towards diagnosis. Some important findings are: | ||
| Line 28: | Line 16: | ||
====Sickle cells==== | ====Sickle cells==== | ||
* Do [[hemoglobulin]] [[electrophoresis]] for [[sickle cell disease]]. | * Do [[hemoglobulin]] [[electrophoresis]] for [[sickle cell disease]]. | ||
====Schistocytes==== | ====Schistocytes==== | ||
* [[HUS]]-[[TTP]], [[DIC]], [[Prosthetic heart valve]], [[malignant hypertension]] | * [[HUS]]-[[TTP]], [[DIC]], [[Prosthetic heart valve]], [[malignant hypertension]] | ||
| Line 53: | Line 35: | ||
==Laboratory Findings== | ==Laboratory Findings== | ||
* Elevated '''total bilirubin''': Elevated bilirubin, or hyperbilirubinemia, is a hallmark of hemolytic anemia | |||
* | * Elevated '''LDH''': | ||
* Low '''haptoglobin''': Haptoglobin is produced in the liver and bind free hemoglobin. During hemolysis, haptoglobin decreases as it is consumed at a faster rate compared to the rate of production by the liver. | |||
* Elevated '''reticulocyte count''': | |||
* Positive '''direct antiglobulin test (DAT)''': | |||
===Specific findings for intravascular hemolysis=== | |||
*Elevated urine hemosiderin | |||
*Elevated urine hemoglobin | |||
*Microangiopathic blood smear | |||
* | |||
* | |||
* | |||
* | |||
* | |||
===Specific findings for extravascular hemolysis=== | |||
*Spherocytic red cell morphology | |||
*Negative urine hemosiderin | |||
*Negative urine hemoglobin | |||
* | |||
* | |||
* | |||
''' | ===Peripheral blood smear=== | ||
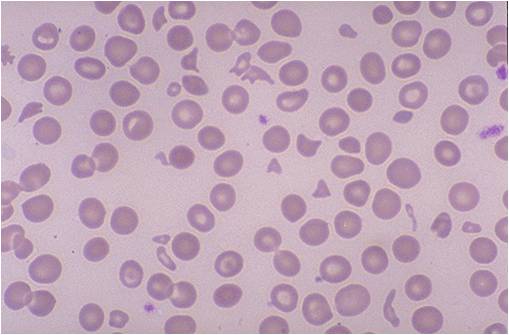
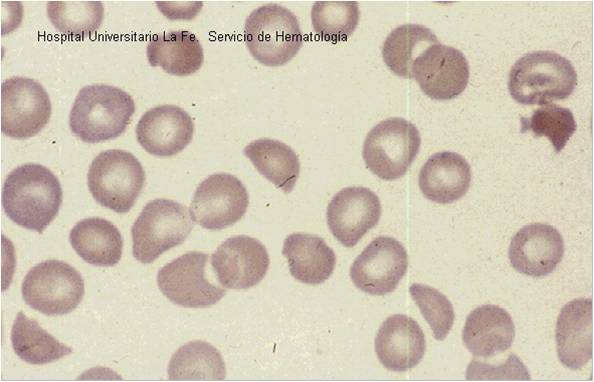
*'''Schistocytes''': These are fragments of red blood cells. They are also known as helmet cells. Presence of schistocytes is not specific for hemolysis but is specific for a microangiopathic process, which can be associated with hemolysis. | |||
*'''Spherocytes''': These are red blood cells that contain a high volume to surface area ratio. These cells have a relative lack of membrane and thus appear as spheres rather than the typical biconcave shape of normal red blood cells. They appear smaller and rounder than normal red blood cells. | |||
*'''Bite cells''': These are also known as Heinz bodies. They are typically seen in patients with hemolysis from G6PD deficiency. Heinz bodies comprise denatured hemoglobin. | |||
*'''Target cells''': These are also known as codocytes. They are not specific for hemolysis, as they can be found in liver disease, thalassemia, hemoglobin E, and hemoglobin C. Electrophoresis helps to differentiate between thalassemia and liver diseases (elevated liver enzymes), and other hemoglobinopathies. | |||
*'''[[Reticulocytes]]''': These are primitive or immature red blood cells. They contain residual ribosomes and RNA. The presence of RNA allows a visible blue stain to bind or, in the case of fluorescent dye, result in a different brightness. This allows them to be detected and counted as a distinct population. When reticulocytes are present in elevated numbers, this suggests an adequate bone marrow response to anemia. The reticulocytes response act as an important indicator for the severity of the hemolytic anemia. The normal reticulocyte count is 0.5-1.5%. In the case of hemolysis, the reticulocyte count can increase to beyond 10%. The different methods used to assess the appropriate response are: | |||
**Absolute reticulocyte count: This is measured in number of cells per microliter. The normal range for absolute reticulocyte count is 25,000 to 75,000 per microliter. | |||
**Corrected reticulocyte count: This is calculated as absolute reticulocyte count divided by reticulocyte maturation time (in days). | |||
**Reticulocyte production index: This is calculated as reticulocytes % x (hematocrit / 45) x (1 / reticulocyte maturation time). The reticulocyte index (RI) should be between 1.0 and 2.0 for a healthy patient. | |||
***RI < 2 with anemia indicates decreased production of reticulocytes and therefore red blood cells. | |||
***RI > 2 with anemia indicates loss of red blood cells (destruction, bleeding, etc) leading to increased compensatory production of reticulocytes to replace the lost red blood cells. | |||
(Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey, and Hospital Universitario La Fe Servicio Hematologia) | (Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey, and Hospital Universitario La Fe Servicio Hematologia) | ||
Revision as of 06:24, 17 October 2017
|
Hemolytic anemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hemolytic anemia laboratory findings On the Web |
|
American Roentgen Ray Society Images of Hemolytic anemia laboratory findings |
|
Risk calculators and risk factors for Hemolytic anemia laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Shyam Patel [2]
Overview
Hemolytic anemia is anemia caused secondary to shortened survival of circulating red blood cells. The normal life span of RBCs is 110 to 120 days. RBC destruction before that time is defined as hemolytic anemia. As opposed to the normal senecence of RBC, the random hemolysis (premature RBC death) is increased in hemolytic anemia.
Approach to diagnosis of hemolytic anemia
Peripheral smear
Findings on peripheral smears can guide towards diagnosis. Some important findings are:
Spherocytes
- Do a direct antiglobulin test
- If antiglobulin negative then diagnosis is hereditary spherocytosis.
- If antiglobulin positive the diagnosis is autoimmune hemolytic anemia.
Sickle cells
Schistocytes
- HUS-TTP, DIC, Prosthetic heart valve, malignant hypertension
- Other tests to rule out between these diagnosis are platelet, PT, PTT, and creatinine
Acanthocytes
- Liver disease
Parasitic inclusion
Thick and thin smear
Direct and Indirect antiglobulin test
- Direct antiglobulin tests test for antibody coating red blood cells.
- Done by mixing the patient's erythrocytes with anti-human globulin (IgG & C3).
- If agglutination occurs, the test is positive.
- 95% sensitive.
- The indirect antiglobulin (indirect Coombs') is done to detect antibodies present in the patient's serum but not coating their red cells.
- Helps in detecting alloantibodies that were introduced by prior transfusion or by fetal transfer of red blood cells to the mother.
Laboratory Findings
- Elevated total bilirubin: Elevated bilirubin, or hyperbilirubinemia, is a hallmark of hemolytic anemia
- Elevated LDH:
- Low haptoglobin: Haptoglobin is produced in the liver and bind free hemoglobin. During hemolysis, haptoglobin decreases as it is consumed at a faster rate compared to the rate of production by the liver.
- Elevated reticulocyte count:
- Positive direct antiglobulin test (DAT):
Specific findings for intravascular hemolysis
- Elevated urine hemosiderin
- Elevated urine hemoglobin
- Microangiopathic blood smear
Specific findings for extravascular hemolysis
- Spherocytic red cell morphology
- Negative urine hemosiderin
- Negative urine hemoglobin
Peripheral blood smear
- Schistocytes: These are fragments of red blood cells. They are also known as helmet cells. Presence of schistocytes is not specific for hemolysis but is specific for a microangiopathic process, which can be associated with hemolysis.
- Spherocytes: These are red blood cells that contain a high volume to surface area ratio. These cells have a relative lack of membrane and thus appear as spheres rather than the typical biconcave shape of normal red blood cells. They appear smaller and rounder than normal red blood cells.
- Bite cells: These are also known as Heinz bodies. They are typically seen in patients with hemolysis from G6PD deficiency. Heinz bodies comprise denatured hemoglobin.
- Target cells: These are also known as codocytes. They are not specific for hemolysis, as they can be found in liver disease, thalassemia, hemoglobin E, and hemoglobin C. Electrophoresis helps to differentiate between thalassemia and liver diseases (elevated liver enzymes), and other hemoglobinopathies.
- Reticulocytes: These are primitive or immature red blood cells. They contain residual ribosomes and RNA. The presence of RNA allows a visible blue stain to bind or, in the case of fluorescent dye, result in a different brightness. This allows them to be detected and counted as a distinct population. When reticulocytes are present in elevated numbers, this suggests an adequate bone marrow response to anemia. The reticulocytes response act as an important indicator for the severity of the hemolytic anemia. The normal reticulocyte count is 0.5-1.5%. In the case of hemolysis, the reticulocyte count can increase to beyond 10%. The different methods used to assess the appropriate response are:
- Absolute reticulocyte count: This is measured in number of cells per microliter. The normal range for absolute reticulocyte count is 25,000 to 75,000 per microliter.
- Corrected reticulocyte count: This is calculated as absolute reticulocyte count divided by reticulocyte maturation time (in days).
- Reticulocyte production index: This is calculated as reticulocytes % x (hematocrit / 45) x (1 / reticulocyte maturation time). The reticulocyte index (RI) should be between 1.0 and 2.0 for a healthy patient.
- RI < 2 with anemia indicates decreased production of reticulocytes and therefore red blood cells.
- RI > 2 with anemia indicates loss of red blood cells (destruction, bleeding, etc) leading to increased compensatory production of reticulocytes to replace the lost red blood cells.
(Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey, and Hospital Universitario La Fe Servicio Hematologia)