Diabetes mellitus type 1 pathophysiology: Difference between revisions
Tarek Nafee (talk | contribs) |
No edit summary |
||
| Line 309: | Line 309: | ||
* T lymphocytes that proliferate when stimulated with islet proteins | * T lymphocytes that proliferate when stimulated with islet proteins | ||
* Release of cytokines within the insulitis | * Release of cytokines within the insulitis | ||
=== Associated conditions === | |||
* Autoimmune thyroid disease (ATD) | |||
* Celiac disease (CD) | |||
* Autoimmune gastritis (AIG) | |||
* Pernicious anemia (PA) | |||
* Vitiligo | |||
* Addison's disease | |||
==References== | ==References== | ||
Revision as of 16:45, 19 December 2016
|
Diabetes mellitus type 1 Microchapters |
|
Differentiating Diabetes mellitus type 1 from other Diseases |
|
Diagnosis |
|
Treatment |
|
Cardiovascular Disease and Risk Management |
|
Case Studies |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Priyamvada Singh, M.B.B.S. [2]; Cafer Zorkun, M.D., Ph.D. [3]
Overview
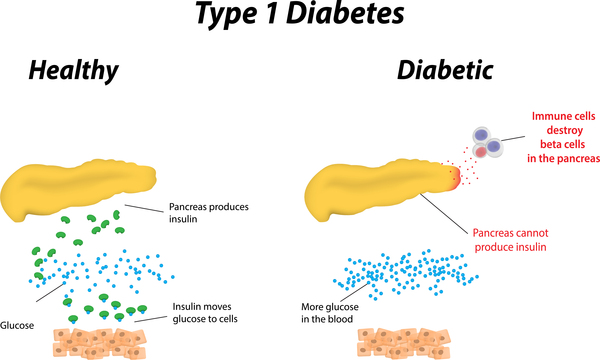
Type 1 diabetes is a disorder characterized by abnormally high blood sugar levels.Type 1 DM is the result of interactions of genetic, environmental, and immunologic factors that ultimately lead to the destruction of the pancreatic beta cells and insulin deficiency.
Pathophysiology
Type 1 diabetes is a disorder characterized by abnormally high blood sugar levels. In this form of diabetes, specialized cells in the pancreas called beta cells stop producing insulin. Insulin controls how much glucose (a type of sugar) is passed from the blood into cells for conversion to energy. Lack of insulin results in the inability to use glucose for energy or to control the amount of sugar in the blood.
Pathogenesis
- Type 1 DM is the result of interactions of genetic, environmental, and immunologic factors that ultimately lead to the destruction of the pancreatic beta cells and insulin deficiency
- Concordance of type 1 DM in identical twins ranges between 40 and 60%, indicating the presence of additional modifying factors.
Genetics
Genes associated with Diabetes mellitus include the following:[1]
- Currently, 58 genomic regions are found to be associated with Type 1 DM.
- Major susceptibility gene for type 1 DM is located on HLA region of chromosome 6. It accounts for 40-50% of the genetic risk for type 1 DM. This region encodes for class II major histocompatibility complex (MHC) molecules. Class II major histocompatibility complex (MHC) molecules play an important role in presenting antigen to helper T cells and initiating immune response.
- Other major susceptibility genes which were associated with Type 1 DM include polymorphisms in the promoter region of the insulin gene, the CTLA-4 gene, interleukin 2 receptor, CTLA4, and PTPN22 etc
- Presence of certain genes confer protection against the development of the disease. Haplotype DQA1*0102, DQB1*0602 is extremely rare in individuals with type 1 DM (<1%) and appears to provide protection from type 1 DM.
| Genes important to type 1 diabetes pathogenesis | Region | Odds ratio | Gene funtion |
|---|---|---|---|
| PTPN22 | 1p13.2 | 1·89 | Regulation of innate immune response, T-cell activation, and natural killer cell proliferation |
| IL10 | 1q32.1 | 0·86 | Cytokines and inflammatory response |
| AFF3 | 2q11.2 | 1·11 | Regulation of transcription |
| IFIH1 | 2q24.2 | 0·85
0·85 0·59 |
Innate immune system NF-κB activation |
| STAT4 | 2q32.3 | 1·10§ | Cytokine-mediated signalling pathway |
| CTLA4 | 2q33.2 | 0·82
0·84 |
T-cell activation |
| CCR5 | 3p21.31 | 0·85 | Th1 cell development and chemokine-mediated signalling pathway |
| IL21, IL2 | 4q27 | 1·13
1·12 1·14 1·15 |
Cytokines and inflammatory response and Th1 or Th2 cell differentiation |
| IL7R | 5p13.2 | 1·11 | T-cell-mediated cytotoxicity, immunoglobulin production, and antigen binding |
| BACH2 | 6q15 | 1·10
0·88 1·20 |
Transcription |
| TNFAIP3 | 6q23.3 | 1·12 | Inflammatory response |
| TAGAP | 6q25.3 | 0·92 | Signal transduction |
| IKZF1 | 7p12.2 | 0·89 | Immune-cell regulation |
| GLIS3 | 9p24.2 | 1·12
1·12 0·90 |
Regulation of transcription |
| IL2RA | 10p15.1 | 1·20
0·73 0·52 0·62 0·82 |
Alternative mRNA splicing Th1 or Th2 cell differentiation |
| PRKCQ | 10p15.1 | 0·69 | Apoptotic process, inflammatory response, innate immune response, and T-cell-receptor signalling pathway |
| NRP1 | 10p11.22 | 1·11 | Signal transduction |
| INS | 11p15.5 | 0·42
0·63 0·63 |
Insulin signalling pathway |
| BAD | 11q13.1 | 0·92 | Apoptosis |
| CD69 | 12p13.31 | 0·87
1·10 |
Signal transduction |
| ITGB7 | 12q13.13 | 1·19 | Response to virus and regulation of immune response |
| ERBB3 | 12q13.2 | 1·25 | Regulation of transcription, innate immune response, and lipid metabolism |
| CYP27B1 | 12q14.1 | 0·82 | Metabolism of lipids, lipoproteins, steroid hormones, and vitamin D |
| SH2B3 | 12q24.12 | 1·24
0·76 0·76 |
Signal transduction |
| GPR183 | 13q32.3 | 1·12 | Humoral immune response |
| DLK1 | 14q32.2 | 0·88
0·90 |
Regulation of gene expression |
| RASGRP1 | 15q14 | 0·85
1·15 |
Inflammatory response to antigenic stimulus and cytokine production |
| CTSH | 15q25.1 | 0·81
0·78 0·90 |
Immune response-regulating signalling pathway T-cell-mediated cytotoxicity adaptive immune response |
| CLEC16A | 16p13.13 | 0·83
0·82 1·14 |
Unknown |
| IL27 | 16p11.2 | 1·19
0·90 1·24 |
Inflammatory response and regulation of defence response to virus |
| ORMDL3 | 17q12 | 0·90 | Protein binding |
| PTPN2 | 18p11.21 | 1·20 | Cytokine signalling and B-cell and T-cell differentiation |
| CD226 | 18q22.2 | 1·13 | Immunoregulation and adaptive immune system |
| TYK2 | 19p13.2 | 0·82
0·87 0·67 |
Cytokine-mediated signalling pathway, intracellular signal transduction, and type I interferon signalling pathway |
| FUT2 | 19q13.33 | 0·87
0·75 0·87 |
Metabolic pathways |
| UBASH3A | 21q22.3 | 1·16 | Regulation of cytokine production
Regulation of T-cell receptor signalling pathway |
| C1QTNF6 | 22q12.3 | 1·11 | B-cell receptor signalling pathway, chemokine signalling pathway, and natural killer cell-mediated cytotoxicity |
Environment
Environmental factors through various pathways were found to influence type 1 DM. Some were found to confer protection against type 1 DM, while others associated with progression and promotion of Type 1 DM, these include :[2]
| Triggers | Protective factors | |
|---|---|---|
| Prenatal triggers |
|
|
| Postnatal triggers |
|
|
| Promoters of progression |
|
Immunological
Several studies have found that abnormalities in the humoral and cellular arm of the immune system, were identified to be associated with Type 1 DM, these include:
- Islet cell autoantibodies
- Activated lymphocytes in the islets, peripancreatic lymph nodes, and systemic circulation
- T lymphocytes that proliferate when stimulated with islet proteins
- Release of cytokines within the insulitis
Associated conditions
- Autoimmune thyroid disease (ATD)
- Celiac disease (CD)
- Autoimmune gastritis (AIG)
- Pernicious anemia (PA)
- Vitiligo
- Addison's disease
References
- ↑ Pociot F, Lernmark Å (2016). "Genetic risk factors for type 1 diabetes". Lancet. 387 (10035): 2331–9. doi:10.1016/S0140-6736(16)30582-7. PMID 27302272.
- ↑ Volume 387, Issue 10035, 4–10 June 2016, Pages 2340–2348 Series Environmental risk factors for type 1 diabetes Prof Marian Rewers, MDa, Prof Johnny Ludvigsson, MD
Template:WH Template:WS Template:WH Template:WS