Sandbox MEN: Difference between revisions
(Created page with "__NOTOC__ {{SI}} '''For patient information, click Insert page name here''' {{CMG}} {{SK}} == Overview == ==Historical Per...") |
No edit summary |
||
| Line 24: | Line 24: | ||
* In 1998 the MEN1 gene was cloned<ref name="Guru1998">Guru SC, Manickam P, Crabtree JS, Olufemi SE, Agarwal SK, Debelenko LV. Identification and characterization of the [[multiple endocrine neoplasia type 1]] (MEN1) gene. ''J Intern Med'' 243(6) 433-9</ref> | * In 1998 the MEN1 gene was cloned<ref name="Guru1998">Guru SC, Manickam P, Crabtree JS, Olufemi SE, Agarwal SK, Debelenko LV. Identification and characterization of the [[multiple endocrine neoplasia type 1]] (MEN1) gene. ''J Intern Med'' 243(6) 433-9</ref> | ||
==Classification== | ==Classification== | ||
==MEN type 1== | |||
{{main|Multiple endocrine neoplasia type 1}} | |||
Type 1 is also known as Wermer's syndrome after Dr Paul Wermer, who described it in 1954:<ref>Wermer P. ''Genetic aspect of adenomatosis of endocrine glands.'' Am J Med 1954;16:363-371. PMID 13138607.</ref> | |||
#[[Parathyroid]] hyperplasia/tumour causing [[hyperparathyroidism]]. | |||
#Pancreatic [[islet cell]] tumours causing [[hypoglycaemia]] ([[insulinoma]]) and [[Zollinger-Ellison syndrome]] ([[gastrinoma]]). | |||
#[[Pituitary]] adenoma which may cause pituitary hormone excess. | |||
The causative mutation is in the MEN1 gene at 11q13 which encodes a nuclear protein called menin that is believed to act as a tumor suppressor. Most cases of multiple endocrine neoplasia type 1 are inherited in an [[autosomal dominant]] pattern. | |||
==MEN type 2== | |||
===MEN type 2/type 2a=== | |||
{{main|Multiple endocrine neoplasia type 2}} | |||
MEN syndrome types 2 and 3 have their basis in molecular genetics. Individuals can be tested for this genetic disorder reliably even when asymptomatic. The mutation is in the [[RET proto-oncogene]]. Most cases of multiple endocrine neoplasia types 2 and 3 are inherited in an [[autosomal dominant]] pattern. | |||
Type 2 is also known as Sipple syndrome (after the American Dr John H. Sipple, who described it in 1961)<ref>Sipple JH. ''The association of pheochromocytoma with carcinoma of the thyroid gland.'' Am J Med 1961;31:163-166.</ref> and used to be called type 2A: | |||
#[[Medullary carcinoma]] of the [[thyroid]] which is associated with increased [[calcitonin]] secretion. A test for elevated calcitonin should be done after [[pentagastrin]] injection and/or calcium infusion, to ensure that all affected patients are detected. | |||
#[[Pheochromocytoma]] | |||
#[[Parathyroid]] hyperplasia/tumour causing [[hyperparathyroidism]]. | |||
===MEN type 3/type 2b=== | |||
This syndrome has no eponym; it was described by Schimke ''et al'' in 1968.<ref>Schimke RN, Hartmann WH, Prout TE, Rimoin DL. ''Syndrome of bilateral pheochromocytoma, medullary thyroid carcinoma and multiple neuromas. A possible regulatory defect in the differentiation of chromaffin tissue.'' [[N Engl J Med]] 1968;279:1-7. PMID 4968712</ref> Originally thought to be a third MEN, then considered a variant of II (especially after linkage to ''RET'' was confirmed), it is now considered its own syndrome. | |||
#[[Pheochromocytoma]] | |||
#Medullary carcinoma of [[thyroid]] which is associated with increased [[calcitonin]] secretion. A test for elevated calcitonin should be done after pentagastrin injection and/or calcium infusion, to ensure that all affected patients are detected. | |||
#Mucosal neuromas which are usually situated in the [[gastrointestinal tract]]. | |||
#[[Marfan syndrome|Marfanoid]] habitus | |||
==Comparison== | |||
[[File:Multiple endocrine neoplasia.png|thumb|center|500px|Presentations of Multiple endocrine neoplasia.]] | |||
Percentages in table below refer to how large fraction of people with the MEN type develop the [[neoplasia]] type. | |||
{| class="wikitable" | |||
|- | |||
! rowspan="2" | Feature | |||
! rowspan="2" | [[Multiple endocrine neoplasia type 1|MEN 1]] | |||
! colspan="3" | [[Multiple endocrine neoplasia type 2|MEN 2]] | |||
|- | |||
! [[Multiple endocrine neoplasia type 2|MEN 2A]] | |||
! Multiple endocrine neoplasia type 2b|MEN 2B | |||
! [[Medullary thyroid cancer|FMTC]] | |||
|- | |||
| Eponym | |||
| Wermer syndrome | |||
| Sipple syndrome | |||
| (multiple) | |||
| (none) | |||
|- | |||
| [[OMIM]] | |||
| {{OMIM4|131100}} | |||
| {{OMIM4|171400}} | |||
| {{OMIM4|162300}} | |||
| {{OMIM4|155240}} | |||
|- | |||
| [[Pancreatic]] tumors | |||
| [[gastrinoma]] (50%<ref name=agabegi2nd4-7/>), <br>[[insulinoma]] (20%<ref name=agabegi2nd4-7/>), <br>[[vipoma]], <br>[[glucagonoma]], <br>[[PPoma]] | |||
| - | |||
| - | |||
| - | |||
|- | |||
| [[Pituitary adenoma]] | |||
| 66%<ref name=agabegi2nd4-7>Table 4-7 in:{{cite book |author=Elizabeth D Agabegi; Agabegi, Steven S. |title=Step-Up to Medicine (Step-Up Series) |publisher=Lippincott Williams & Wilkins |location=Hagerstwon, MD |year=2008 |pages= |isbn=0-7817-7153-6 |oclc= |doi= |accessdate=}}</ref> | |||
| - | |||
| - | |||
| - | |||
|- | |||
| [[Angiofibroma]] | |||
| 64%*<ref name=Asgharian>{{cite journal|last=Asgharian|first=B |author2=Turner, ML |author3=Gibril, F |author4=Entsuah, LK |author5=Serrano, J |author6=Jensen, RT|title=Cutaneous tumors in patients with multiple endocrine neoplasm type 1 (MEN1) and gastrinomas: prospective study of frequency and development of criteria with high sensitivity and specificity for MEN1.|journal=The Journal of Clinical Endocrinology and Metabolism|date=November 2004|volume=89|issue=11|pages=5328–36|pmid=15531478|doi=10.1210/jc.2004-0218}}</ref> | |||
| - | |||
| - | |||
| - | |||
|- | |||
| [[Lipoma]] | |||
| 17%*<ref name=Asgharian /> | |||
| - | |||
| - | |||
| - | |||
|- | |||
| [[Parathyroid]] hyperplasia | |||
| 90%<ref name=agabegi2nd4-7/> | |||
| 50%<ref name=agabegi2nd4-7/> | |||
| - | |||
| - | |||
|- | |||
| [[Medullary thyroid carcinoma]] | |||
| - | |||
| 100%<ref name=agabegi2nd4-7/> | |||
| 85%<ref name=agabegi2nd4-7/> | |||
| 100% | |||
|- | |||
| [[Pheochromocytoma]] | |||
| - | |||
| >33%<ref name=agabegi2nd4-7/> | |||
| 50% | |||
| - | |||
|- | |||
| [[Marfan syndrome|Marfanoid]] body habitus | |||
| - | |||
| - | |||
| 80% | |||
| - | |||
|- | |||
| Mucosal [[neuroma]] | |||
| - | |||
| - | |||
| 100%<ref name=agabegi2nd4-7/> | |||
| - | |||
|- | |||
| [[Gene]](s) | |||
| [[MEN1]] ({{OMIM4|131100}}) | |||
| [[RET proto-oncogene|RET]] ({{OMIM4|164761}}) | |||
| [[RET proto-oncogene|RET]] ({{OMIM4|164761}}) | |||
| [[RET proto-oncogene|RET]] ({{OMIM4|164761}}),<br/>[[NTRK1]] ({{OMIM4|191315}}) | |||
|- | |||
| Approx. [[prevalence]] | |||
| 1 in 35,000 <br> (1 in 20,000 to<br> 1 in 40,000)<ref>[http://www.dovepress.com/getfile.php?fileID=5129] 123I labeled metaiodobenzylguanidine for diagnosis of neuroendocrine tumors. Jiang L, Schipper ML, Li P, Cheng Z, Reports in Medical Imaging. 2009: 2 79-89</ref> | |||
| 1 in 40,000<ref>{{cite journal |author=Dora JM, Siqueira DR, Meyer EL, Puñales MK, Maia AL |title=Pancreatitis as the first manifestation of multiple endocrine neoplasia type 2A |journal=Arq Bras Endocrinol Metabol |volume=52 |issue=8 |pages=1332–6 |date=November 2008 |pmid=19169490 |doi= 10.1590/S0004-27302008000800021|url=}}</ref> | |||
| 1 in 1,000,000<br/>(1 in 600,000<ref>{{cite book |last=Marx |first=Stephen J |editor-last=Melmed |editor-first=Shlomo |title=Williams Textbook of Endocrinology, 12th ed. |year=2011 |pages=1728–1767 |chapter=Chapter 41: Multiple endocrine neoplasia }}</ref> to<br/>1 in 4,000,000<ref>{{cite journal |author=Moline J, Eng C. |title= Multiple endocrine neoplasia type 2: An overview|journal=Genetics in Medicine |volume=13 |issue=9 |pages=755–764 |year=2011 |pmid= 21552134 |url=http://www.nature.com/gim/journal/v13/n9/full/gim2011127a.html |doi=10.1097/GIM.0b013e318216cc6d}}</ref>)<ref>{{cite book |author=Martino Ruggieri |title=Neurocutaneous Disorders : The Phakomatoses |publisher=Springer |location=Berlin |year=2005 |pages= |isbn=3-211-21396-1 |oclc= |doi= |accessdate=}} - Chapter: ''Multiple Endocrine Neoplasia Type 2B '' by Electron Kebebew, Jessica E. Gosnell and Emily Reiff. Pages 695-701. [http://www.springerlink.com/content/qu78313220701167/] This reference quotes a prevalence of 1 in 40,000, but this figure is inconsistent with the same reference's calculated incidence of 4 per 100 million per year for MEN2B.</ref> | |||
| | |||
|- | |||
| Initial description (year) | |||
| 1954<ref>{{cite journal |author=Wermer P |title=Genetic aspects of adenomatosis of endocrine glands |journal=Am. J. Med. |volume=16 |issue=3 |pages=363–71 |year=1954 |pmid=13138607 |doi= 10.1016/0002-9343(54)90353-8|url=http://linkinghub.elsevier.com/retrieve/pii/0002-9343(54)90353-8}}</ref> | |||
| 1961<ref>{{cite journal |author=Sipple JH |title=The association of pheochromocytoma with carcinoma of the thyroid gland |journal=Am. J. Med. |volume=31 |issue= |pages=163–6 |year=1961 |pmid= |doi= 10.1016/0002-9343(61)90234-0|url=}}</ref> | |||
| 1965 | |||
| | |||
|} | |||
<nowiki>*</nowiki>- of patients with MEN1 and gastrinoma | |||
FMTC = familial medullary [[thyroid]] [[cancer]] | |||
* Multiple endocrine neoplasia type 2b|MEN 2B is sometimes known as MEN 3 and the designation varies by institution (c.f. www.ClinicalReview.com). | |||
* Although a variety of additional eponyms have been proposed for MEN2B (e.g. Williams-Pollock syndrome, Gorlin-Vickers syndrome, and Wagenmann–Froboese syndrome), none ever gained sufficient traction to merit continued use and, indeed, are all but abandoned in the medical literature. Another early report was Schimke ''et al.'' in 1968.<ref>{{cite journal |author=Schimke RN, Hartmann WH, Prout TE, Rimoin DL |title=Syndrome of bilateral pheochromocytoma, medullary thyroid carcinoma and multiple neuromas. A possible regulatory defect in the differentiation of chromaffin tissue |journal=N. Engl. J. Med. |volume=279 |issue=1 |pages=1–7 |year=1968 |pmid=4968712 |doi= 10.1056/NEJM196807042790101|url=}}</ref> | |||
* [[OMIM]] also includes a fourth form of multiple endocrine neoplasia ("MEN4"), associated with CDKN1B.<ref>{{OMIM|610755|MULTIPLE ENDOCRINE NEOPLASIA, TYPE IV; MEN4}}</ref> The presentation is believed to overlap that of MEN1 and MEN2.<ref name="pmid17030811">{{cite journal |author=Pellegata NS, Quintanilla-Martinez L, Siggelkow H, et al. |title=Germ-line mutations in p27Kip1 cause a multiple endocrine neoplasia syndrome in rats and humans |journal=Proc. Natl. Acad. Sci. U.S.A. |volume=103 |issue=42 |pages=15558–63 |date=Oct 2006 |pmid=17030811 |pmc=1622862 |doi=10.1073/pnas.0603877103 |url=http://www.pnas.org/cgi/pmidlookup?view=long&pmid=17030811|bibcode=2006PNAS..10315558P |last2=Quintanilla-Martinez |last3=Siggelkow |last4=Samson |last5=Bink |last6=Hofler |last7=Fend |last8=Graw |last9=Atkinson }}</ref> | |||
== Pathophysiology== | == Pathophysiology== | ||
* The term multiple endocrine neoplasia (MEN) encompasses several distinct [[syndrome]]s featuring [[Endocrine gland neoplasm|tumors of endocrine gland]]s, each with its own characteristic pattern. In some cases, the [[tumor]]s are [[malignant]], in others, [[benign]]. [[Benign]] or [[malignant]] [[tumor]]s of nonendocrine [[tissue]]s occur as components of some of these [[tumor]] [[syndrome]]s. | * The term multiple endocrine neoplasia (MEN) encompasses several distinct [[syndrome]]s featuring [[Endocrine gland neoplasm|tumors of endocrine gland]]s, each with its own characteristic pattern. In some cases, the [[tumor]]s are [[malignant]], in others, [[benign]]. [[Benign]] or [[malignant]] [[tumor]]s of nonendocrine [[tissue]]s occur as components of some of these [[tumor]] [[syndrome]]s. | ||
| Line 33: | Line 161: | ||
* [[Von Hippel-Lindau disease]] | * [[Von Hippel-Lindau disease]] | ||
* [[Carney complex]] | * [[Carney complex]] | ||
===Gross Pathology=== | ===Gross Pathology=== | ||
Revision as of 17:40, 30 September 2015
|
WikiDoc Resources for Sandbox MEN |
|
Articles |
|---|
|
Most recent articles on Sandbox MEN Most cited articles on Sandbox MEN |
|
Media |
|
Powerpoint slides on Sandbox MEN |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Sandbox MEN at Clinical Trials.gov Clinical Trials on Sandbox MEN at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Sandbox MEN
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Sandbox MEN Discussion groups on Sandbox MEN Patient Handouts on Sandbox MEN Directions to Hospitals Treating Sandbox MEN Risk calculators and risk factors for Sandbox MEN
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Sandbox MEN |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information, click Insert page name here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]
Synonyms and keywords:
Overview
Historical Perspective
- In 1903 Erdheim described the case of an acromegalic patient with a pituitary adenoma and three enlarged parathyroid glands.
- In 1953 Underdahl et al. reported a case series of 8 patients with a syndrome of pituitary, parathyroid, and pancreatic islet adenomas.
- In 1954 Wermer noted that this syndrome was transmitted as a dominant trait.
- In 1959 Hazard et al. described medullary (solid) thyroid carcinoma.
- In 1961 Sipple described a combination of a pheochromocytoma, medullary thyroid carcinoma and parathyroid adenoma.
- In 1966 Williams et al. described the combination of mucosal neuromas, pheochromocytoma and medullary thyroid carcinoma.
- In 1968 Steiner et al. introduced the term "multiple endocrine neoplasia" (MEN) to describe disorders featuring combinations of endocrine tumors and proposed the terms 'Wermer syndrome' for MEN 1 and 'Sipple syndrome' for MEN 2.
- In 1974 Sizemore et al. showed that the MEN 2 category included two groups of patients with MTC and pheochromocytoma: one with parathyroid disease and a normal appearance (MEN 2A) and the other without parathyroid disease but with mucosal neuromas and mesodermal abnormalities (MEN 2B).
- In 1988 the MEN1 locus was assigned to Chromosome 11 (11q13).
- In 1993 mutations in the RET oncogene were shown to be the cause of MEN 2A by Lois Mulligan, working in the laboratory of Dr Bruce Ponder in Cambridge.[1]
- In 1998 the MEN1 gene was cloned[2]
Classification
MEN type 1
Type 1 is also known as Wermer's syndrome after Dr Paul Wermer, who described it in 1954:[3]
- Parathyroid hyperplasia/tumour causing hyperparathyroidism.
- Pancreatic islet cell tumours causing hypoglycaemia (insulinoma) and Zollinger-Ellison syndrome (gastrinoma).
- Pituitary adenoma which may cause pituitary hormone excess.
The causative mutation is in the MEN1 gene at 11q13 which encodes a nuclear protein called menin that is believed to act as a tumor suppressor. Most cases of multiple endocrine neoplasia type 1 are inherited in an autosomal dominant pattern.
MEN type 2
MEN type 2/type 2a
MEN syndrome types 2 and 3 have their basis in molecular genetics. Individuals can be tested for this genetic disorder reliably even when asymptomatic. The mutation is in the RET proto-oncogene. Most cases of multiple endocrine neoplasia types 2 and 3 are inherited in an autosomal dominant pattern.
Type 2 is also known as Sipple syndrome (after the American Dr John H. Sipple, who described it in 1961)[4] and used to be called type 2A:
- Medullary carcinoma of the thyroid which is associated with increased calcitonin secretion. A test for elevated calcitonin should be done after pentagastrin injection and/or calcium infusion, to ensure that all affected patients are detected.
- Pheochromocytoma
- Parathyroid hyperplasia/tumour causing hyperparathyroidism.
MEN type 3/type 2b
This syndrome has no eponym; it was described by Schimke et al in 1968.[5] Originally thought to be a third MEN, then considered a variant of II (especially after linkage to RET was confirmed), it is now considered its own syndrome.
- Pheochromocytoma
- Medullary carcinoma of thyroid which is associated with increased calcitonin secretion. A test for elevated calcitonin should be done after pentagastrin injection and/or calcium infusion, to ensure that all affected patients are detected.
- Mucosal neuromas which are usually situated in the gastrointestinal tract.
- Marfanoid habitus
Comparison
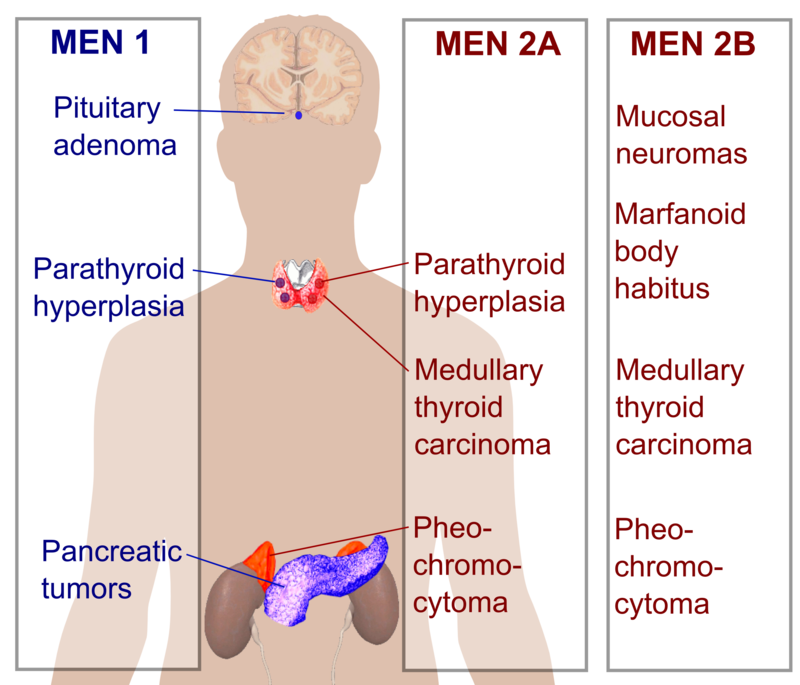
Percentages in table below refer to how large fraction of people with the MEN type develop the neoplasia type.
| Feature | MEN 1 | MEN 2 | ||
|---|---|---|---|---|
| MEN 2A | MEN 2B | FMTC | ||
| Eponym | Wermer syndrome | Sipple syndrome | (multiple) | (none) |
| OMIM | Template:OMIM4 | Template:OMIM4 | Template:OMIM4 | Template:OMIM4 |
| Pancreatic tumors | gastrinoma (50%[6]), insulinoma (20%[6]), vipoma, glucagonoma, PPoma |
- | - | - |
| Pituitary adenoma | 66%[6] | - | - | - |
| Angiofibroma | 64%*[7] | - | - | - |
| Lipoma | 17%*[7] | - | - | - |
| Parathyroid hyperplasia | 90%[6] | 50%[6] | - | - |
| Medullary thyroid carcinoma | - | 100%[6] | 85%[6] | 100% |
| Pheochromocytoma | - | >33%[6] | 50% | - |
| Marfanoid body habitus | - | - | 80% | - |
| Mucosal neuroma | - | - | 100%[6] | - |
| Gene(s) | MEN1 (Template:OMIM4) | RET (Template:OMIM4) | RET (Template:OMIM4) | RET (Template:OMIM4), NTRK1 (Template:OMIM4) |
| Approx. prevalence | 1 in 35,000 (1 in 20,000 to 1 in 40,000)[8] |
1 in 40,000[9] | 1 in 1,000,000 (1 in 600,000[10] to 1 in 4,000,000[11])[12] |
|
| Initial description (year) | 1954[13] | 1961[14] | 1965 | |
*- of patients with MEN1 and gastrinoma
FMTC = familial medullary thyroid cancer
- Multiple endocrine neoplasia type 2b|MEN 2B is sometimes known as MEN 3 and the designation varies by institution (c.f. www.ClinicalReview.com).
- Although a variety of additional eponyms have been proposed for MEN2B (e.g. Williams-Pollock syndrome, Gorlin-Vickers syndrome, and Wagenmann–Froboese syndrome), none ever gained sufficient traction to merit continued use and, indeed, are all but abandoned in the medical literature. Another early report was Schimke et al. in 1968.[15]
- OMIM also includes a fourth form of multiple endocrine neoplasia ("MEN4"), associated with CDKN1B.[16] The presentation is believed to overlap that of MEN1 and MEN2.[17]
Pathophysiology
- The term multiple endocrine neoplasia (MEN) encompasses several distinct syndromes featuring tumors of endocrine glands, each with its own characteristic pattern. In some cases, the tumors are malignant, in others, benign. Benign or malignant tumors of nonendocrine tissues occur as components of some of these tumor syndromes.
- MEN syndromes are inherited as autosomal dominant disorders.[18]
Genetics
Associated Conditions
Gross Pathology
Microscopic Pathology
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
Causes by Organ System
| Cardiovascular | No underlying causes |
| Chemical / poisoning | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | No underlying causes |
| Ear Nose Throat | No underlying causes |
| Endocrine | No underlying causes |
| Environmental | No underlying causes |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | No underlying causes |
| Iatrogenic | No underlying causes |
| Infectious Disease | No underlying causes |
| Musculoskeletal / Ortho | No underlying causes |
| Neurologic | No underlying causes |
| Nutritional / Metabolic | No underlying causes |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | No underlying causes |
| Opthalmologic | No underlying causes |
| Overdose / Toxicity | No underlying causes |
| Psychiatric | No underlying causes |
| Pulmonary | No underlying causes |
| Renal / Electrolyte | No underlying causes |
| Rheum / Immune / Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | No underlying causes |
| Urologic | No underlying causes |
| Dental | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
- A...
- Z...
Make sure that each diagnosis is linked to a page.
Differentiating type page name here from other Diseases
Epidemiology and Demographics
Age
Gender
Race
Developed Countries
Developing Countries
Risk Factors
Screening
Natural History, Complications and Prognosis
Diagnosis
Diagnostic Criteria
If available, the diagnostic criteria are provided here.
History
A directed history should be obtained to ascertain
Symptoms
"Type symptom here" is pathognomonic of the "type disease name here".
"Type non specific symptoms" may be present.
Past Medical History
Family History
Social History
Occupational
Alcohol
The frequency and amount of alcohol consumption should be characterized.
Drug Use
Smoking
Allergies
Physical Examination
Appearance of the Patient
Vital Signs
Skin
Head
Eyes
Ear
Nose
Mouth
Throat
Heart
Lungs
Abdomen
Extremities
Neurologic
Genitals
Other
Laboratory Findings
Electrolyte and Biomarker Studies
Electrocardiogram
Chest X Ray
CT
MRI
Echocardiography or Ultrasound
Other Imaging Findings
Other Diagnostic Studies
Treatment
Pharmacotherapy
Acute Pharmacotherapies
Chronic Pharmacotherapies
Surgery and Device Based Therapy
Indications for Surgery
Pre-Operative Assessment
Post-Operative Management
Transplantation
Primary Prevention
Secondary Prevention
Cost-Effectiveness of Therapy
Future or Investigational Therapies
References
- ↑ Germ-line mutations of the RET proto-oncogene in multiple endocrine neoplasia type 2A. Mulligan LM, Kwok JB, Healey CS, Elsdon MJ, Eng C, Gardner E, Love DR, Mole SE, Moore JK, Papi L, et al. Nature 1993 Jun 3;363(6428) 458-60 PMID 8099202
- ↑ Guru SC, Manickam P, Crabtree JS, Olufemi SE, Agarwal SK, Debelenko LV. Identification and characterization of the multiple endocrine neoplasia type 1 (MEN1) gene. J Intern Med 243(6) 433-9
- ↑ Wermer P. Genetic aspect of adenomatosis of endocrine glands. Am J Med 1954;16:363-371. PMID 13138607.
- ↑ Sipple JH. The association of pheochromocytoma with carcinoma of the thyroid gland. Am J Med 1961;31:163-166.
- ↑ Schimke RN, Hartmann WH, Prout TE, Rimoin DL. Syndrome of bilateral pheochromocytoma, medullary thyroid carcinoma and multiple neuromas. A possible regulatory defect in the differentiation of chromaffin tissue. N Engl J Med 1968;279:1-7. PMID 4968712
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 Table 4-7 in:Elizabeth D Agabegi; Agabegi, Steven S. (2008). Step-Up to Medicine (Step-Up Series). Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 0-7817-7153-6.
- ↑ 7.0 7.1 Asgharian, B; Turner, ML; Gibril, F; Entsuah, LK; Serrano, J; Jensen, RT (November 2004). "Cutaneous tumors in patients with multiple endocrine neoplasm type 1 (MEN1) and gastrinomas: prospective study of frequency and development of criteria with high sensitivity and specificity for MEN1". The Journal of Clinical Endocrinology and Metabolism. 89 (11): 5328–36. doi:10.1210/jc.2004-0218. PMID 15531478.
- ↑ [1] 123I labeled metaiodobenzylguanidine for diagnosis of neuroendocrine tumors. Jiang L, Schipper ML, Li P, Cheng Z, Reports in Medical Imaging. 2009: 2 79-89
- ↑ Dora JM, Siqueira DR, Meyer EL, Puñales MK, Maia AL (November 2008). "Pancreatitis as the first manifestation of multiple endocrine neoplasia type 2A". Arq Bras Endocrinol Metabol. 52 (8): 1332–6. doi:10.1590/S0004-27302008000800021. PMID 19169490.
- ↑ Marx, Stephen J (2011). "Chapter 41: Multiple endocrine neoplasia". In Melmed, Shlomo. Williams Textbook of Endocrinology, 12th ed. pp. 1728–1767.
- ↑ Moline J, Eng C. (2011). "Multiple endocrine neoplasia type 2: An overview". Genetics in Medicine. 13 (9): 755–764. doi:10.1097/GIM.0b013e318216cc6d. PMID 21552134.
- ↑ Martino Ruggieri (2005). Neurocutaneous Disorders : The Phakomatoses. Berlin: Springer. ISBN 3-211-21396-1. - Chapter: Multiple Endocrine Neoplasia Type 2B by Electron Kebebew, Jessica E. Gosnell and Emily Reiff. Pages 695-701. [2] This reference quotes a prevalence of 1 in 40,000, but this figure is inconsistent with the same reference's calculated incidence of 4 per 100 million per year for MEN2B.
- ↑ Wermer P (1954). "Genetic aspects of adenomatosis of endocrine glands". Am. J. Med. 16 (3): 363–71. doi:10.1016/0002-9343(54)90353-8. PMID 13138607.
- ↑ Sipple JH (1961). "The association of pheochromocytoma with carcinoma of the thyroid gland". Am. J. Med. 31: 163–6. doi:10.1016/0002-9343(61)90234-0.
- ↑ Schimke RN, Hartmann WH, Prout TE, Rimoin DL (1968). "Syndrome of bilateral pheochromocytoma, medullary thyroid carcinoma and multiple neuromas. A possible regulatory defect in the differentiation of chromaffin tissue". N. Engl. J. Med. 279 (1): 1–7. doi:10.1056/NEJM196807042790101. PMID 4968712.
- ↑ Online Mendelian Inheritance in Man (OMIM) MULTIPLE ENDOCRINE NEOPLASIA, TYPE IV; MEN4 -610755
- ↑ Pellegata NS, Quintanilla-Martinez L, Siggelkow H; Quintanilla-Martinez; Siggelkow; Samson; Bink; Hofler; Fend; Graw; Atkinson; et al. (Oct 2006). "Germ-line mutations in p27Kip1 cause a multiple endocrine neoplasia syndrome in rats and humans". Proc. Natl. Acad. Sci. U.S.A. 103 (42): 15558–63. Bibcode:2006PNAS..10315558P. doi:10.1073/pnas.0603877103. PMC 1622862. PMID 17030811.
- ↑ Template:DorlandsDict