Colorectal cancer screening: Difference between revisions
(→Other screening techniques: Added new study to DNA) |
|||
| (70 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
{{tocleft}} | |||
{{Colon cancer}} | {{Colon cancer}} | ||
To view the screening of familial adenomatous polyposis (FAP), click [[Familial adenomatous polyposis differential screening|'''here''']]<br> | |||
To view the screening of hereditary nonpolyposis colorectal cancer (HNPCC), click [[Hereditary nonpolyposis colorectal cancer differential screening|'''here''']]<br><br> | |||
{{CMG}} {{AE}}; {{RAK}} Elliot B. Tapper, M.D.; Saarah T. Alkhairy, M.D. | |||
''' | ==Overview== | ||
Early detection of premalignant colorectal masses or early-stage colorectal cancers is essential in treating these patients and possibly preventing cancer or colorectal cancer related death. According to the [[United states preventive services task force recommendations scheme|USPSTF]] (United States Preventive Services Task Force): [[Screening]] for colorectal cancer is recommended among adults older than 50 years of age and do not have an increased risk of developing the disease (average-risk adults). | |||
==Clinical practice guidelines== | |||
According to the '''USPSTF''' (United States Preventive Services Task Force):<ref name="pmid27304597">{{cite journal| author=US Preventive Services Task Force. Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW et al.| title=Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. | journal=JAMA | year= 2016 | volume= 315 | issue= 23 | pages= 2564-2575 | pmid=27304597 | doi=10.1001/jama.2016.5989 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27304597 }}</ref> | |||
* Screening for colorectal cancer is recommended among adults older than 50 years of age and do not have an increased risk of developing the disease ('''average-risk''' adults). | |||
* Decision to screen for colorectal cancer among adults aged 76 to 85 years is an individual one. | |||
** Screening would be more beneficial for healthier individuals that are able to undergo possible treatment. | |||
* Screening for colorectal cancer among adults aged 86 years and older is not recommended. | |||
* No preference is given to one screening modality over the other | |||
** Decision should be shared and according to the patient's preferences when it comes to choosing an option. | |||
* Screening options:<ref name="pmid27304597" /> | |||
*# '''[[Colonoscopy]]''' | |||
*# '''FIT''' | |||
*#* Fecal immunochemical testing for occult blood | |||
*# '''[[Flexible sigmoidoscopy]]''' | |||
*# '''Flexible sigmoidoscopy''' + '''FIT''' | |||
*# '''CT colonography''' | |||
*# '''FIT-DNA''' | |||
*#* multitargeted stool DNA testing | |||
*# '''gFOBT''' | |||
*#* Guaiac-based fecal occult blood testing | |||
Screening for colorectal cancer in individuals that are at increased risk of developing the disease is different and depends on several factors:<ref name="Lieberman2009">{{cite journal|last1=Lieberman|first1=David A.|title=Screening for Colorectal Cancer|journal=New England Journal of Medicine|volume=361|issue=12|year=2009|pages=1179–1187|issn=0028-4793|doi=10.1056/NEJMcp0902176}}</ref><ref name="pmid27304597" /> | |||
* Family history of colorectal cancer before age 50 | |||
** Begin screening at an earlier age | |||
* Risk of rapid disease progression | |||
** Perform screening more frequently | |||
* Family history of [[Hereditary nonpolyposis colorectal cancer|HNPCC]] or [[FAP]] | |||
** Use most sensitive screening modality: colonoscopy | |||
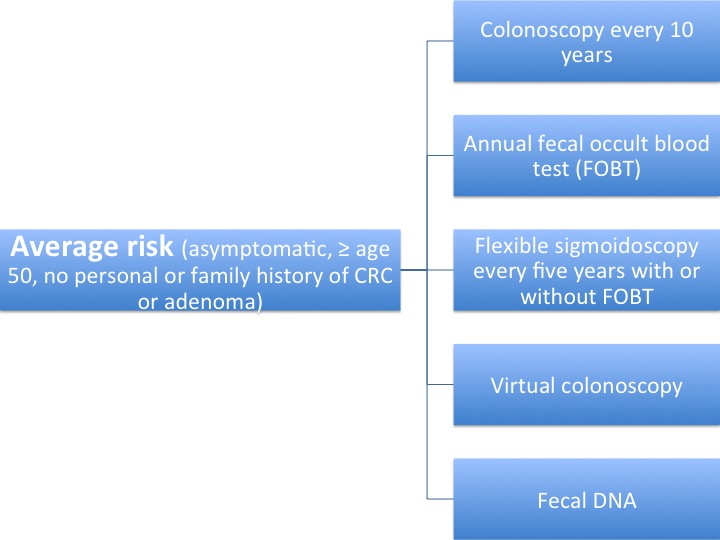
== Screening protocols summarized in the figures below: == | |||
Protocols have been summarized according to USPSTF guidelines.<ref name="pmid27304597" />[[Image:Average risk CRC.jpg|center|500x500px|frame|Screening protocol for '''average risk''' patients]] | |||
[[Image:Moderate risk CRC.jpg|center|500x500px|frame|Screening protocol for '''moderate risk''' patients]] | |||
[[Image:High risk CRC.jpg|center|500x500px|frame|Screening protocol for '''high risk''' patients]] | |||
==Types of Screening Methods== | |||
===Fecal Occult Blood Testing=== | |||
*A [[fecal occult blood]] test is a test for blood in the stool. | |||
* There are two types of tests that can be used for detecting occult blood in stools:<ref name="pmid27304597" /><ref name="pmid20824704">{{cite journal| author=Duffy MJ, van Rossum LG, van Turenhout ST, Malminiemi O, Sturgeon C, Lamerz R et al.| title=Use of faecal markers in screening for colorectal neoplasia: a European group on tumor markers position paper. | journal=Int J Cancer | year= 2011 | volume= 128 | issue= 1 | pages= 3-11 | pmid=20824704 | doi=10.1002/ijc.25654 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20824704 }}</ref> | |||
*# '''FIT''' | |||
*#* Fecal immunochemical testing for occult blood | |||
*# '''gFOBT''' | |||
*#* Guaiac-based fecal occult blood testing | |||
* Use of low-sensitivity guaiac fecal tests is not recommended due to its of low sensitivity.<ref name="pmid27304597" /> | |||
== | ===Endoscopy=== | ||
*A [[sigmoidoscopy|'''sigmoidoscopy''']] is a lighted probe ([[sigmoidoscope]]) that is inserted into the [[rectum]] and lower [[colon]] to check for [[polyps]] and other abnormalities.<ref name="pmid16635231" /> | |||
*A [[colonoscopy|'''colonoscopy''']] is a lighted probe ([[colonoscope]]) that is inserted into the [[rectum]] and the entire [[colon]] to look for [[polyp (medicine)|polyp]]s and other abnormalities that may be caused by [[cancer]]. A [[colonoscopy]] has the advantage that if [[polyp (medicine)|polyp]]s are found during the procedure they can be immediately removed, and the tissue can also be taken for [[biopsy]]. The [http://www.asge.org/ American Society for Gastrointestinal Endoscopy] has released quality indicators for screening [[colonoscopy]], which include:<ref name="pmid16635231">{{cite journal| author=Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE et al.| title=Quality indicators for colonoscopy. | journal=Am J Gastroenterol | year= 2006 | volume= 101 | issue= 4 | pages= 873-85 | pmid=16635231 | doi=10.1111/j.1572-0241.2006.00673.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16635231 }} </ref> | |||
:*Documentation of prep quality | |||
:*Photo documentation of [[Cecum|cecal]] [[intubation]] | |||
:*Withdrawal time of 6 minutes or more | |||
:*[[Adenoma]] detection rate of greater than 25% in males and 15% in females greater than 50 years old | |||
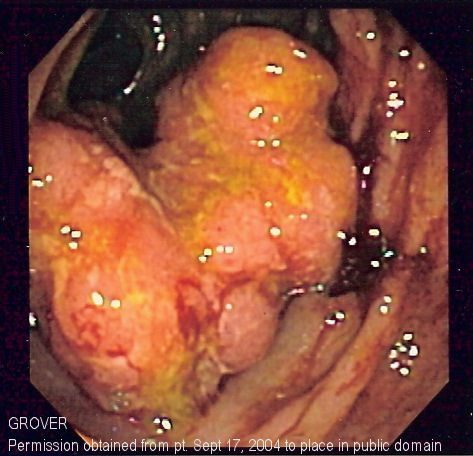
[[Image:Colorectal cancer endo 2.jpg|473x473px]] | |||
==Screening | === CT colonography === | ||
:* Also known as Virtual Colonoscopy | |||
:* Requires special workstation software in order for the [[radiologist]] to interpret | |||
:* This technique is approaching [[colonoscopy]] in sensitivity for [[polyps]] | |||
:* Any polyps found must still be removed by standard [[colonoscopy]]<ref name="pmid14657435">{{cite journal| author=Morrin MM, LaMont JT| title=Screening virtual colonoscopy--ready for prime time? | journal=N Engl J Med | year= 2003 | volume= 349 | issue= 23 | pages= 2261-4 | pmid=14657435 | doi=10.1056/NEJMe038181 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14657435 }}</ref> | |||
=== Fecal DNA testing === | |||
:* Multitargeted stool DNA testing | |||
:* Ability to detect mutations from DNA shed by colorectal cancer<ref name="pmid15017656">{{cite journal| author=Calistri D, Rengucci C, Bocchini R, Saragoni L, Zoli W, Amadori D| title=Fecal multiple molecular tests to detect colorectal cancer in stool. | journal=Clin Gastroenterol Hepatol | year= 2003 | volume= 1 | issue= 5 | pages= 377-83 | pmid=15017656 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15017656 }}</ref> | |||
==Accuracy of screening methods== | |||
Advanced adenomas are defined as being ≥10 mm, having villous histology, or having high grade dysplasia. Advanced neoplasia is defined as cancer or advanced adenoma<ref name="pmid27441328">{{cite journal| author=Lin JS, Piper MA, Perdue LA, Rutter C, Webber EM, O’Connor E | display-authors=etal| title=Screening for Colorectal Cancer: A Systematic Review for the U.S. Preventive Services Task Force | journal=U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews | year= 2016 | volume= | issue= | pages= | pmid=27441328 | doi= | pmc= | url= }} </ref>. | |||
< | |||
= | {| class="wikitable" | ||
|+ Accuracy of screening tests to detect colorectal cancer and advanced adenomas<ref name="pmid34003220">{{cite journal| author=Lin JS, Perdue LA, Henrikson NB, Bean SI, Blasi PR| title=Screening for Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. | journal=JAMA | year= 2021 | volume= 325 | issue= 19 | pages= 1978-1997 | pmid=34003220 | doi=10.1001/jama.2021.4417 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=34003220 }} </ref>. | |||
|- | |||
! Method | |||
! Sensitivity | |||
! Specificity | |||
|- | |||
| colspan="3" style="text-align:center;" | Colorectal cancer | |||
|- | |||
| Colonoscopy | |||
| NA | |||
| NA | |||
|- | |||
| Fecal Immunochemical Test (FIT) | |||
| 74 | |||
| 94 | |||
|- | |||
| Cologuard (sDNA + FIT) | |||
| 93 | |||
| 85 | |||
|- | |||
| colspan="3" style="text-align:center;" | Advanced adenoma | |||
|- | |||
| Colonoscopy (for adenoma > 10 mm) | |||
| 89 to 95 | |||
| NA | |||
|- | |||
| Fecal Immunochemical Test (FIT) | |||
| 23 | |||
| 96 | |||
|- | |||
| Cologuard (sDNA + FIT) | |||
| 43 | |||
| 89 | |||
|} | |||
==References== | == References == | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
[[Category:Types of cancer]] | [[Category:Types of cancer]] | ||
[[Category:Conditions diagnosed by stool test]] | [[Category:Conditions diagnosed by stool test]] | ||
| Line 56: | Line 127: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Gastroenterology]] | |||
[[Category:Surgery]] | |||
Latest revision as of 15:03, 2 June 2021
|
Colorectal cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Colorectal cancer screening On the Web |
|
American Roentgen Ray Society Images of Colorectal cancer screening |
|
Risk calculators and risk factors for Colorectal cancer screening |
To view the screening of familial adenomatous polyposis (FAP), click here
To view the screening of hereditary nonpolyposis colorectal cancer (HNPCC), click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: ; Roukoz A. Karam, M.D.[2] Elliot B. Tapper, M.D.; Saarah T. Alkhairy, M.D.
Overview
Early detection of premalignant colorectal masses or early-stage colorectal cancers is essential in treating these patients and possibly preventing cancer or colorectal cancer related death. According to the USPSTF (United States Preventive Services Task Force): Screening for colorectal cancer is recommended among adults older than 50 years of age and do not have an increased risk of developing the disease (average-risk adults).
Clinical practice guidelines
According to the USPSTF (United States Preventive Services Task Force):[1]
- Screening for colorectal cancer is recommended among adults older than 50 years of age and do not have an increased risk of developing the disease (average-risk adults).
- Decision to screen for colorectal cancer among adults aged 76 to 85 years is an individual one.
- Screening would be more beneficial for healthier individuals that are able to undergo possible treatment.
- Screening for colorectal cancer among adults aged 86 years and older is not recommended.
- No preference is given to one screening modality over the other
- Decision should be shared and according to the patient's preferences when it comes to choosing an option.
- Screening options:[1]
- Colonoscopy
- FIT
- Fecal immunochemical testing for occult blood
- Flexible sigmoidoscopy
- Flexible sigmoidoscopy + FIT
- CT colonography
- FIT-DNA
- multitargeted stool DNA testing
- gFOBT
- Guaiac-based fecal occult blood testing
Screening for colorectal cancer in individuals that are at increased risk of developing the disease is different and depends on several factors:[2][1]
- Family history of colorectal cancer before age 50
- Begin screening at an earlier age
- Risk of rapid disease progression
- Perform screening more frequently
- Family history of HNPCC or FAP
- Use most sensitive screening modality: colonoscopy
Screening protocols summarized in the figures below:
Protocols have been summarized according to USPSTF guidelines.[1]


Types of Screening Methods
Fecal Occult Blood Testing
- A fecal occult blood test is a test for blood in the stool.
- There are two types of tests that can be used for detecting occult blood in stools:[1][3]
- FIT
- Fecal immunochemical testing for occult blood
- gFOBT
- Guaiac-based fecal occult blood testing
- FIT
- Use of low-sensitivity guaiac fecal tests is not recommended due to its of low sensitivity.[1]
Endoscopy
- A sigmoidoscopy is a lighted probe (sigmoidoscope) that is inserted into the rectum and lower colon to check for polyps and other abnormalities.[4]
- A colonoscopy is a lighted probe (colonoscope) that is inserted into the rectum and the entire colon to look for polyps and other abnormalities that may be caused by cancer. A colonoscopy has the advantage that if polyps are found during the procedure they can be immediately removed, and the tissue can also be taken for biopsy. The American Society for Gastrointestinal Endoscopy has released quality indicators for screening colonoscopy, which include:[4]
- Documentation of prep quality
- Photo documentation of cecal intubation
- Withdrawal time of 6 minutes or more
- Adenoma detection rate of greater than 25% in males and 15% in females greater than 50 years old
CT colonography
- Also known as Virtual Colonoscopy
- Requires special workstation software in order for the radiologist to interpret
- This technique is approaching colonoscopy in sensitivity for polyps
- Any polyps found must still be removed by standard colonoscopy[5]
Fecal DNA testing
- Multitargeted stool DNA testing
- Ability to detect mutations from DNA shed by colorectal cancer[6]
Accuracy of screening methods
Advanced adenomas are defined as being ≥10 mm, having villous histology, or having high grade dysplasia. Advanced neoplasia is defined as cancer or advanced adenoma[7].
| Method | Sensitivity | Specificity |
|---|---|---|
| Colorectal cancer | ||
| Colonoscopy | NA | NA |
| Fecal Immunochemical Test (FIT) | 74 | 94 |
| Cologuard (sDNA + FIT) | 93 | 85 |
| Advanced adenoma | ||
| Colonoscopy (for adenoma > 10 mm) | 89 to 95 | NA |
| Fecal Immunochemical Test (FIT) | 23 | 96 |
| Cologuard (sDNA + FIT) | 43 | 89 |
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 US Preventive Services Task Force. Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW; et al. (2016). "Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement". JAMA. 315 (23): 2564–2575. doi:10.1001/jama.2016.5989. PMID 27304597.
- ↑ Lieberman, David A. (2009). "Screening for Colorectal Cancer". New England Journal of Medicine. 361 (12): 1179–1187. doi:10.1056/NEJMcp0902176. ISSN 0028-4793.
- ↑ Duffy MJ, van Rossum LG, van Turenhout ST, Malminiemi O, Sturgeon C, Lamerz R; et al. (2011). "Use of faecal markers in screening for colorectal neoplasia: a European group on tumor markers position paper". Int J Cancer. 128 (1): 3–11. doi:10.1002/ijc.25654. PMID 20824704.
- ↑ 4.0 4.1 Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE; et al. (2006). "Quality indicators for colonoscopy". Am J Gastroenterol. 101 (4): 873–85. doi:10.1111/j.1572-0241.2006.00673.x. PMID 16635231.
- ↑ Morrin MM, LaMont JT (2003). "Screening virtual colonoscopy--ready for prime time?". N Engl J Med. 349 (23): 2261–4. doi:10.1056/NEJMe038181. PMID 14657435.
- ↑ Calistri D, Rengucci C, Bocchini R, Saragoni L, Zoli W, Amadori D (2003). "Fecal multiple molecular tests to detect colorectal cancer in stool". Clin Gastroenterol Hepatol. 1 (5): 377–83. PMID 15017656.
- ↑ Lin JS, Piper MA, Perdue LA, Rutter C, Webber EM, O’Connor E; et al. (2016). "Screening for Colorectal Cancer: A Systematic Review for the U.S. Preventive Services Task Force". U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. PMID 27441328.
- ↑ Lin JS, Perdue LA, Henrikson NB, Bean SI, Blasi PR (2021). "Screening for Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force". JAMA. 325 (19): 1978–1997. doi:10.1001/jama.2021.4417. PMID 34003220 Check
|pmid=value (help).