|
|
| (337 intermediate revisions by 2 users not shown) |
| Line 3: |
Line 3: |
| {{CMG}} {{AE}} {{Trusha}} | | {{CMG}} {{AE}} {{Trusha}} |
|
| |
|
| == tab == | | ==new== |
|
| |
|
| {| class="wikitable"
| |
| |- style="background: #4479BA; color: #FFFFFF; text-align: center;"
| |
| ! rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Diseases
| |
| | colspan="6" rowspan="1" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Clinical manifestations'''
| |
| ! colspan="7" rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Para-clinical findings
| |
| | colspan="1" rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Gold standard'''
| |
| ! rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Comments
| |
| |-
| |
| | colspan="6" rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Symptoms'''
| |
| |-
| |
| ! colspan="3" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Lab Findings
| |
| ! colspan="3" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Imaging
| |
| ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Histopathology
| |
| |-
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Constipation/Diarrhea
| |
| ! colspan="1" rowspan="1" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Blood in stool
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Abdominal pain
| |
| ! colspan="3" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Other symptoms
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Anemia
| |
| ! colspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Tumor marker
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Endoscopy
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |CT scan
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Other
| |
| diagnostic
| |
|
| |
|
| study
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |Adenocarcinoma
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | colspan="2" style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Arteriovenous malformation]]<ref name="pmid28139503">{{cite journal |vauthors=Lee HH, Kwon HM, Gil S, Kim YS, Cho M, Seo KJ, Chae HS, Cho YS |title=Endoscopic resection of asymptomatic, colonic, polypoid arteriovenous malformations: Two case reports and a literature review |journal=Saudi J Gastroenterol |volume=23 |issue=1 |pages=67–70 |date=2017 |pmid=28139503 |pmc=5329980 |doi=10.4103/1319-3767.199111 |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" | +
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" | +
| |
| | colspan="2" style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Bright red, flat lesions
| |
| * Rarely, polypoid
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Aberrant vessels with thickened, hypertrophic walls in the mucosa and the submucosa.
| |
| * Arteries directly connected to veins without capillary beds
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Diverticular disease|Diverticular diseases]]<ref name="pmid16187597">{{cite journal |vauthors=Shen SH, Chen JD, Tiu CM, Chou YH, Chiang JH, Chang CY, Lee CH |title=Differentiating colonic diverticulitis from colon cancer: the value of computed tomography in the emergency setting |journal=J Chin Med Assoc |volume=68 |issue=9 |pages=411–8 |date=September 2005 |pmid=16187597 |doi=10.1016/S1726-4901(09)70156-X |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Constipation]]
| |
| and/or
| |
| * [[Diarrhea]]<ref name="ShenChen2005">{{cite journal|last1=Shen|first1=Shu-Huei|last2=Chen|first2=Jen-Dar|last3=Tiu|first3=Chui-Mei|last4=Chou|first4=Yi-Hong|last5=Chiang|first5=Jen-Huei|last6=Chang|first6=Cheng-Yen|last7=Lee|first7=Chen-Hsen|title=Differentiating Colonic Diverticulitis from Colon Cancer: The Value of Computed Tomography in the Emergency Setting|journal=Journal of the Chinese Medical Association|volume=68|issue=9|year=2005|pages=411–418|issn=17264901|doi=10.1016/S1726-4901(09)70156-X}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" | +/-
| |
| | style="background: #F5F5F5; padding: 5px;" | +
| |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Fever]], [[Rigor|chills]]<ref name="ShenChen2005">{{cite journal|last1=Shen|first1=Shu-Huei|last2=Chen|first2=Jen-Dar|last3=Tiu|first3=Chui-Mei|last4=Chou|first4=Yi-Hong|last5=Chiang|first5=Jen-Huei|last6=Chang|first6=Cheng-Yen|last7=Lee|first7=Chen-Hsen|title=Differentiating Colonic Diverticulitis from Colon Cancer: The Value of Computed Tomography in the Emergency Setting|journal=Journal of the Chinese Medical Association|volume=68|issue=9|year=2005|pages=411–418|issn=17264901|doi=10.1016/S1726-4901(09)70156-X}}</ref>
| |
| * [[Nausea and vomiting|Nausea/vomiting(N/V)]]
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | colspan="2" style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |Not recommended <ref name="ShenChen2005">{{cite journal|last1=Shen|first1=Shu-Huei|last2=Chen|first2=Jen-Dar|last3=Tiu|first3=Chui-Mei|last4=Chou|first4=Yi-Hong|last5=Chiang|first5=Jen-Huei|last6=Chang|first6=Cheng-Yen|last7=Lee|first7=Chen-Hsen|title=Differentiating Colonic Diverticulitis from Colon Cancer: The Value of Computed Tomography in the Emergency Setting|journal=Journal of the Chinese Medical Association|volume=68|issue=9|year=2005|pages=411–418|issn=17264901|doi=10.1016/S1726-4901(09)70156-X}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Outpouchings of the colonic wall (Diverticula)<ref name="ShenChen2005">{{cite journal|last1=Shen|first1=Shu-Huei|last2=Chen|first2=Jen-Dar|last3=Tiu|first3=Chui-Mei|last4=Chou|first4=Yi-Hong|last5=Chiang|first5=Jen-Huei|last6=Chang|first6=Cheng-Yen|last7=Lee|first7=Chen-Hsen|title=Differentiating Colonic Diverticulitis from Colon Cancer: The Value of Computed Tomography in the Emergency Setting|journal=Journal of the Chinese Medical Association|volume=68|issue=9|year=2005|pages=411–418|issn=17264901|doi=10.1016/S1726-4901(09)70156-X}}</ref>
| |
| * Inflamed diverticula
| |
| * Abscess formation
| |
| * Intraperitoneal free air (microperforation)
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Barium enema: Circumferential narrowing<ref name="SheimanLevine20082">{{cite journal|last1=Sheiman|first1=Laura|last2=Levine|first2=Marc S.|last3=Levin|first3=Alicia A.|last4=Hogan|first4=Jonathan|last5=Rubesin|first5=Stephen E.|last6=Furth|first6=Emma E.|last7=Laufer|first7=Igor|title=Chronic Diverticulitis: Clinical, Radiographic, and Pathologic Findings|journal=American Journal of Roentgenology|volume=191|issue=2|year=2008|pages=522–528|issn=0361-803X|doi=10.2214/AJR.07.3597}}</ref>
| |
| * Spiculated contour and tapered margins
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hemorrhoids]]<ref name="JacobsSolomon2014">{{cite journal|last1=Jacobs|first1=Danny|last2=Solomon|first2=Caren G.|title=Hemorrhoids|journal=New England Journal of Medicine|volume=371|issue=10|year=2014|pages=944–951|issn=0028-4793|doi=10.1056/NEJMcp1204188}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Constipation]]
| |
| | style="background: #F5F5F5; padding: 5px;" | +
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" |
| |
| * Perianal Itching
| |
| * Pain with [[defecation]]
| |
| * Painful, hard lump in anus
| |
| | style="background: #F5F5F5; padding: 5px;" | +
| |
| | colspan="2" style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Anoscopy]]: Protruding mass from the [[anus]]
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * DRE: Palpable mass, tender if thrombosed
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Anal fissure]]<ref name="pmid27041801">{{cite journal |vauthors=Schlichtemeier S, Engel A |title=Anal fissure |journal=Aust Prescr |volume=39 |issue=1 |pages=14–7 |year=2016 |pmid=27041801 |pmc=4816871 |doi=10.18773/austprescr.2016.007 |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" | +
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" |
| |
| * Painful [[defecation]]
| |
| * [[Itching]]
| |
| * [[Irritation]]
| |
| | style="background: #F5F5F5; padding: 5px;" | +/-
| |
| | colspan="2" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Anoscopy]]: Anal wall laceration
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Infectious colitis]]<ref name="pmid22080825">{{cite journal |vauthors=DuPont HL |title=Approach to the patient with infectious colitis |journal=Curr. Opin. Gastroenterol. |volume=28 |issue=1 |pages=39–46 |date=January 2012 |pmid=22080825 |doi=10.1097/MOG.0b013e32834d3208 |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Diarrhea]]
| |
| | style="background: #F5F5F5; padding: 5px;" | +
| |
| | style="background: #F5F5F5; padding: 5px;" | +
| |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Fever]], [[Rigor|chills]]
| |
| * [[Nausea and vomiting|N/V]]
| |
| * [[Bloating]]
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | colspan="2" style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Patchy or diffuse [[Erythematous|erythematous mucosa]]
| |
| * Edema, [[hemorrhage]], with or without [[ulcers]] of mucosa
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Stool culture|Stool cultures]] in adequate [[culture media]]
| |
| * Stool analysis: Leukocytosis
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |Peutz-Jeghers syndrome<ref name="pmid27298573">{{cite journal |vauthors=Zhong ME, Niu BZ, Ji WY, Wu B |title=Laparoscopic restorative proctocolectomy with ileal pouch-anal anastomosis for Peutz-Jeghers syndrome with synchronous rectal cancer |journal=World J. Gastroenterol. |volume=22 |issue=22 |pages=5293–6 |date=June 2016 |pmid=27298573 |doi=10.3748/wjg.v22.i22.5293 |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| |- style="background: #4479BA; color: #FFFFFF; text-align: center;"
| |
| ! rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Diseases
| |
| | colspan="6" rowspan="1" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Clinical manifestations'''
| |
| ! colspan="7" rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Para-clinical findings
| |
| | colspan="1" rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Gold standard'''
| |
| ! rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Comments
| |
| |-
| |
| | colspan="6" rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Symptoms'''
| |
| |-
| |
| ! colspan="3" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Lab Findings
| |
| ! colspan="3" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Imaging
| |
| ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Histopathology
| |
| |-
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Constipation/Diarrhea
| |
| ! colspan="1" rowspan="1" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Blood in stool
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Abdominal pain
| |
| ! colspan="3" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Other symptoms
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Anemia
| |
| ! colspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Tumor marker
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Colonoscopy
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |CT scan
| |
| ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Other diagnostic study
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |Carcinoids<ref name="pmid20011309">{{cite journal |vauthors=Chung TP, Hunt SR |title=Carcinoid and neuroendocrine tumors of the colon and rectum |journal=Clin Colon Rectal Surg |volume=19 |issue=2 |pages=45–8 |date=May 2006 |pmid=20011309 |pmc=2780103 |doi=10.1055/s-2006-942343 |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |Juvenile Polyposis Coli
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |Gastrointestinal Stromal Tumors (GIST)<ref name="pmid24778074">{{cite journal |vauthors=Niazi AK, Kaley K, Saif MW |title=Gastrointestinal stromal tumor of colon: a case report and review of literature |journal=Anticancer Res. |volume=34 |issue=5 |pages=2547–50 |date=May 2014 |pmid=24778074 |doi= |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |Hamartoms
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |Colorectal Lymphoma<ref name="pmid20011310">{{cite journal |vauthors=Quayle FJ, Lowney JK |title=Colorectal lymphoma |journal=Clin Colon Rectal Surg |volume=19 |issue=2 |pages=49–53 |date=May 2006 |pmid=20011310 |pmc=2780105 |doi=10.1055/s-2006-942344 |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Kaposi's sarcoma]]<ref name="pmid20827371">{{cite journal |vauthors=Arora M, Goldberg EM |title=Kaposi sarcoma involving the gastrointestinal tract |journal=Gastroenterol Hepatol (N Y) |volume=6 |issue=7 |pages=459–62 |date=July 2010 |pmid=20827371 |pmc=2933764 |doi= |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Diarrhea]]
| |
| | style="background: #F5F5F5; padding: 5px;" |+
| |
| | style="background: #F5F5F5; padding: 5px;" |Diffuse
| |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Melena]]
| |
|
| |
|
| * [[Hematochezia]]
| | {| align="right" |
| * [[Abdominal pain]]
| | | |
| * [[Nausea and vomiting|N/V]]
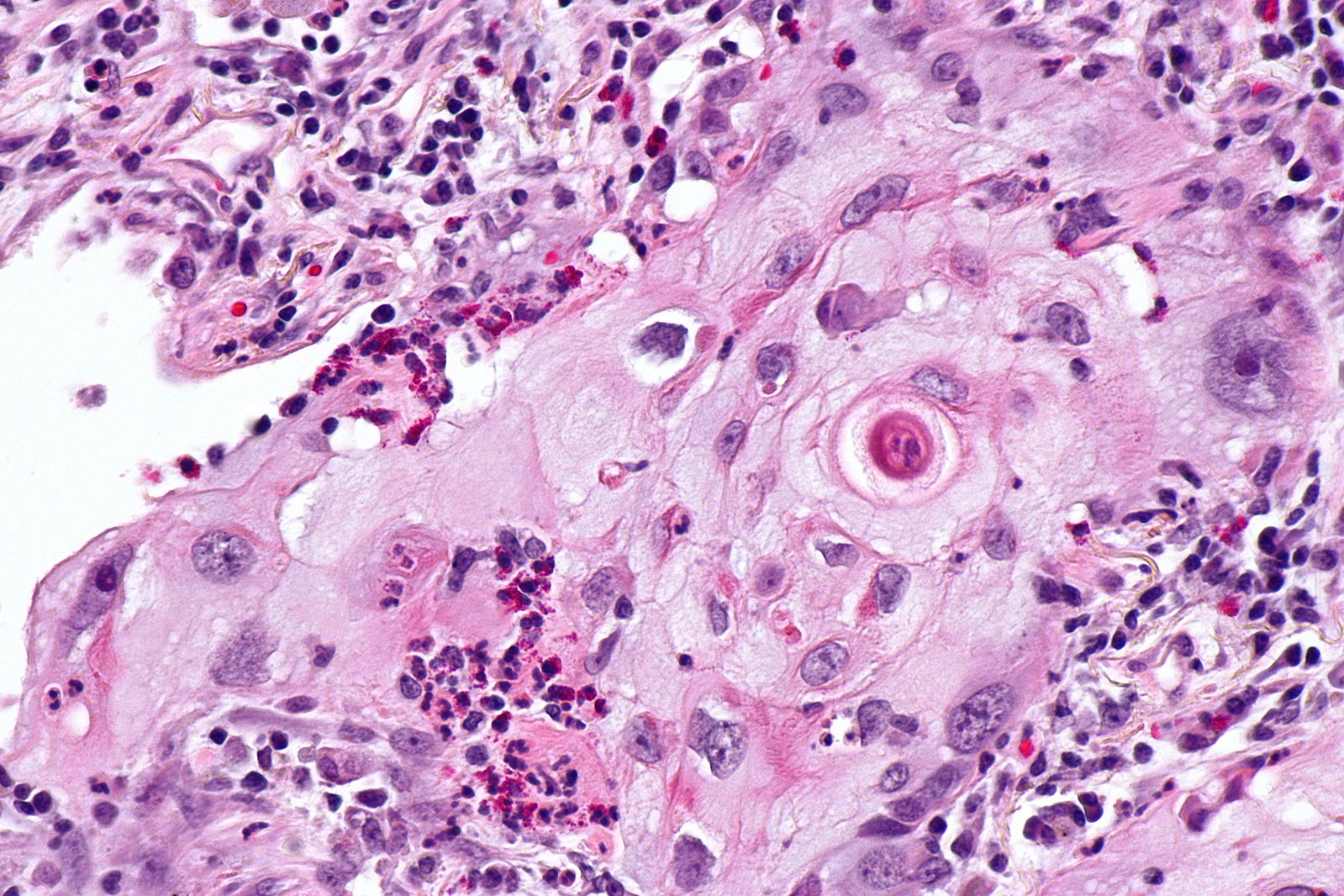
| | [[Image:Squamous cell mircopathology2.jpeg|x200px|thumb| Micropathology: Squamous cell carcinoma of the lung. H&E stain, By Nephron [https://commons.wikimedia.org/wiki/File%3ALung_squamous_carcinoma_--_high_mag.jpg Wikimedia Commons]]] |
| | style="background: #F5F5F5; padding: 5px;" |+
| | |} |
| | colspan="2" style="background: #F5F5F5; padding: 5px;" | | | {| align="right" |
| * [[CD34]]
| | | |
| * [[CD31]]
| | [[Image:Bronchial cancer.jpeg|x200px|thumb|Gross pathology: Bronchial squamous lung cell cancer By John Hayman [Public domain], (Image source: [https://commons.wikimedia.org/wiki/File%3ACa_bronchus.jpg Wikimedia Commons])]] |
| * [[D2-40]]
| | |} |
| * [[HHV-8]]
| | |
| * [[FHI-1]] antibody
| | {| |
| * [[LANA-1]]
| | |
| | style="background: #F5F5F5; padding: 5px;" |
| | |
| * Localized purpuric lesion
| | # [[Superior vena cava obstruction]] |
| | style="background: #F5F5F5; padding: 5px;" | | | # [[Partial anomalous pulmonary venous connection]] |
| * N/A
| | # [[Esophageal achalasia]] |
| | style="background: #F5F5F5; padding: 5px;" |
| | # [[Esophageal cancer]] |
| * Electrophoresis: [[antibodies]] against Kaposi sarcoma herpes virus (HHV-8)
| | # [[Esophageal rupture]] |
| * Biopsy: [[Vascular]] proliferation, red blood cell and [[hemosiderin]] extravasation,[[Lymphocyte|lymphocytes]] and [[Monocyte|monocytes]], neovascular lesion wrapped around a pre-existing space, intracytoplasmic PAS +ve [[hyaline]] globules
| | # [[Hiatus hernia]] |
| | style="background: #F5F5F5; padding: 5px;" |
| | # [[Hilar lymphadenopathy]] |
| * [[Vascular]] proliferation
| | # [[Pneumomediastinum]] |
| * Red blood cell and [[hemosiderin]] extravasation
| | # [[Sarcoidosis]] |
| * [[Lymphocyte|Lymphocytes]] and [[Monocyte|monocytes]]
| | # [[Lymphoma]] |
| * Premonitory sign (a neovascular lesion wrapped around a pre-existing space)
| | # [[Neurilemmoma]] |
| * Intracytoplasmic PAS +ve [[hyaline]] globules
| | # [[Non-Hodgkin lymphoma]] |
| | style="background: #F5F5F5; padding: 5px;" | | | # [[Teratoma]] |
| * Biopsy
| | # [[Thymoma]] |
| | style="background: #F5F5F5; padding: 5px;" |
| | |
| |- | | # [[Thyroid cancer]] |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Ulcerative colitis]]<ref name="pmid25075198">{{cite journal |vauthors=Fakhoury M, Negrulj R, Mooranian A, Al-Salami H |title=Inflammatory bowel disease: clinical aspects and treatments |journal=J Inflamm Res |volume=7 |issue= |pages=113–20 |date=2014 |pmid=25075198 |pmc=4106026 |doi=10.2147/JIR.S65979 |url=}}</ref>
| | # [[Goitre]] |
| | style="background: #F5F5F5; padding: 5px;" | | | # [[Mediastinal germ cell tumor]], |
| * [[Diarrhea]]
| | # [[Mediastinal tumor]], |
| | style="background: #F5F5F5; padding: 5px;" |<big>+</big>
| | # [[Mediastinitis]] |
| | style="background: #F5F5F5; padding: 5px;" |LLQ<ref name="pmid25075198">{{cite journal |vauthors=Fakhoury M, Negrulj R, Mooranian A, Al-Salami H |title=Inflammatory bowel disease: clinical aspects and treatments |journal=J Inflamm Res |volume=7 |issue= |pages=113–20 |date=2014 |pmid=25075198 |pmc=4106026 |doi=10.2147/JIR.S65979 |url=}}</ref>
| | |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" |
| | # [[Churg-Strauss syndrome]] |
| | style="background: #F5F5F5; padding: 5px;" | +
| | # [[Bronchogenic cyst]], |
| | colspan="2" style="background: #F5F5F5; padding: 5px;" |
| | # [[Dermoid cyst]] |
| | style="background: #F5F5F5; padding: 5px;" |
| | # [[Anthrax]]: |
| * Continuous lesions<ref name="pmid25075198">{{cite journal |vauthors=Fakhoury M, Negrulj R, Mooranian A, Al-Salami H |title=Inflammatory bowel disease: clinical aspects and treatments |journal=J Inflamm Res |volume=7 |issue= |pages=113–20 |date=2014 |pmid=25075198 |pmc=4106026 |doi=10.2147/JIR.S65979 |url=}}</ref>
| | # [[Tularemia]] |
| * [[Erythema]] (or redness of the [[mucosa]]) and friability of the [[mucosa]]
| | |
| * Crypts, formation of residual mucosal tissue
| | |
| * [[Polyp (medicine)|Pseudopolyps]]
| | [[File:Mediastinal lymohangioma GIF.gif|x200px|thumb| CT scan shows cystic mass which was located on the posterior to the lower esophagus later diagnosed as thoracic duct lymphangioma. [https://doi.org/10.5090/kjtcs.2014.47.4.423 Source:Case courtesy of Jin San Bok et al, Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital]]] |
| | style="background: #F5F5F5; padding: 5px;" | -
| | |
| | style="background: #F5F5F5; padding: 5px;" |
| | |
| | style="background: #F5F5F5; padding: 5px;" |
| | [[File:Posterior-mediastinal-schwannoma.gif|x200px|thumb| CT scan showing a soft tissue density lesion within the left posterior mediastinum, in a paravertebral location. The lesion is closely related to the left neural exit foramen, but there is no definite extension into the spinal canal. The lesion does extend into the intercostal space. |
| * Mucosal and submucosal inflammation<ref name="pmid25075198">{{cite journal |vauthors=Fakhoury M, Negrulj R, Mooranian A, Al-Salami H |title=Inflammatory bowel disease: clinical aspects and treatments |journal=J Inflamm Res |volume=7 |issue= |pages=113–20 |date=2014 |pmid=25075198 |pmc=4106026 |doi=10.2147/JIR.S65979 |url=}}</ref>
| | Case courtesy of Dr Paul Leong |
| * Hemorrhage or inflammatory polymorphonuclear cells aggregate in the lamina propria
| | (Picture courtesy:[https://radiopaedia.org/cases/26625 Radiopedia])]] |
| * Distorted crypts
| | |
| * Crypt abscess
| | |
| | style="background: #F5F5F5; padding: 5px;" |
| | |
| * Endoscopy and a mucosal biopsy<ref name="pmid16902215" />
| | |
| | style="background: #F5F5F5; padding: 5px;" |
| | __NOTOC__ |
| |-
| | {{SI}} |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Crohn's disease]]<ref name="pmid25075198">{{cite journal |vauthors=Fakhoury M, Negrulj R, Mooranian A, Al-Salami H |title=Inflammatory bowel disease: clinical aspects and treatments |journal=J Inflamm Res |volume=7 |issue= |pages=113–20 |date=2014 |pmid=25075198 |pmc=4106026 |doi=10.2147/JIR.S65979 |url=}}</ref>
| | {{CMG}}; {{AE}} {{Trusha}}, {{AM}} |
| | style="background: #F5F5F5; padding: 5px;" |
| | |
| * [[Diarrhea]]
| | {{SK}} Mediastinal enlargement; mass in the mediastinum |
| | style="background: #F5F5F5; padding: 5px;" | +
| | |
| | style="background: #F5F5F5; padding: 5px;" |LRQ<ref name="pmid25075198">{{cite journal |vauthors=Fakhoury M, Negrulj R, Mooranian A, Al-Salami H |title=Inflammatory bowel disease: clinical aspects and treatments |journal=J Inflamm Res |volume=7 |issue= |pages=113–20 |date=2014 |pmid=25075198 |pmc=4106026 |doi=10.2147/JIR.S65979 |url=}}</ref>
| | ==Overview== |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" |
| |
| * Tenesmus
| |
| *
| |
| | style="background: #F5F5F5; padding: 5px;" | +
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Discontinuous lesions
| |
| * Strictures
| |
| * Linear ulcerations<ref name="pmid25075198">{{cite journal |vauthors=Fakhoury M, Negrulj R, Mooranian A, Al-Salami H |title=Inflammatory bowel disease: clinical aspects and treatments |journal=J Inflamm Res |volume=7 |issue= |pages=113–20 |date=2014 |pmid=25075198 |pmc=4106026 |doi=10.2147/JIR.S65979 |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Transmural pattern of inflammation<ref name="pmid25075198">{{cite journal |vauthors=Fakhoury M, Negrulj R, Mooranian A, Al-Salami H |title=Inflammatory bowel disease: clinical aspects and treatments |journal=J Inflamm Res |volume=7 |issue= |pages=113–20 |date=2014 |pmid=25075198 |pmc=4106026 |doi=10.2147/JIR.S65979 |url=}}</ref>
| |
| * Mucosal damage
| |
| * Focal infiltration of leukocytes into the epithelium
| |
| * Granulomas
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Endoscopy and a mucosal biopsy<ref name="pmid16902215">{{cite journal |vauthors=Collins P, Rhodes J |title=Ulcerative colitis: diagnosis and management |journal=BMJ |volume=333 |issue=7563 |pages=340–3 |date=August 2006 |pmid=16902215 |pmc=1539087 |doi=10.1136/bmj.333.7563.340 |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |Irritable bowel syndrome
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Constipation]]
| |
| and/or
| |
| * [[diarrhea]]
| |
| | style="background: #F5F5F5; padding: 5px;" | +
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" |
| |
| * Straining during [[defecation]]
| |
| * [[Urgency]]
| |
| * Sensation of incomplete evacuation
| |
| * [[Mucus]] passage
| |
| * [[Bloating]]
| |
| * Weight loss
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | colspan="2" style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |Nor recommended
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Diagnosis of exclusion with fulfilment of [[Irritable bowel syndrome diagnostic criteria|Rome criteria]]<ref name="pmid28875974">{{cite journal |vauthors=Iwańczak B, Iwańczak F |title=[Functional gastrointestinal disorders in children and adolescents. The Rome IV criteria] |language=Polish |journal=Pol. Merkur. Lekarski |volume=43 |issue=254 |pages=75–82 |date=August 2017 |pmid=28875974 |doi= |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Clinical diagnosis ([[Irritable bowel syndrome Diagnostic Study of Choice|Rome criteria]])<ref name="pmid28875974" />
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Appendicitis]]<ref name="pmid14616200">{{cite journal |vauthors=Choi D, Park H, Lee YR, Kook SH, Kim SK, Kwag HJ, Chung EC |title=The most useful findings for diagnosing acute appendicitis on contrast-enhanced helical CT |journal=Acta Radiol |volume=44 |issue=6 |pages=574–82 |year=2003 |pmid=14616200 |doi= |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * [[Diarrhea]]
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |RLQ
| |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" |
| |
| * Pain starting periumbilical before localizing to the [[right iliac fossa]]
| |
| * [[Nausea and vomiting|N/V]]
| |
| * [[Fever]], [[Rigor|chills]]
| |
| * [[Anorexia|Loss of appetite]]
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | colspan="2" style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Appendiceal wall thickening (wall ≥ 3mm)
| |
| * Periappendiceal fat stranding
| |
| * Thickening of the [[Fascia|lateral conal fascia]] and [[mesoappendix]]
| |
| * Extraluminal fluid
| |
| * [[Phlegmon]]
| |
| * [[Abscess]]
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Tc-99m labeled anti-CD15 antibodies
| |
| * Ultrasound:
| |
| ** Aperistaltic, noncompressible, dilated appendix (>6 mm outer diameter)
| |
| ** [[Appendicolith]]
| |
| ** Echogenic prominent pericaecal fat
| |
| ** Periappeniceal fluid collection
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" | | |
| * [[Computed tomography|CT scan]]
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |
| |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| |- style="background: #4479BA; color: #FFFFFF; text-align: center;"
| |
| !Diseases
| |
| !Symptom 1
| |
| ! colspan="1" rowspan="1" |Symptom 2
| |
| !Symptom 3
| |
| !Physical exam 1
| |
| ! colspan="1" rowspan="1" |Physical exam 2
| |
| !Physical exam 3
| |
| !Lab 1
| |
| !Lab 2
| |
| !Lab 3
| |
| !Imaging 1
| |
| !Imaging 2
| |
| !Imaging 3
| |
| !Histopathology
| |
| |'''Gold standard'''
| |
| !Additional findings
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Strangulated hernia]]
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * Constipation
| |
| | style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |[[Right lower quadrant abdominal pain resident survival guide|RLQ]]
| |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" |[[Nausea and vomiting|N/V]]
| |
|
| |
|
| Heaviness or dull discomfort in the groin, with straining, lifting, coughing, or exercising
| | The [[mediastinum]] is a non-delineated group of structures in the thorax (chest), surrounded by loose connective tissue. Since it is the central compartment of the thoracic cavity, and it contains a lot of important structures, it is the site of involvement of various tumors. |
|
| |
|
| Weakness, heaviness, burning, or aching in the groin
| | ==Causes== |
|
| |
|
| Pain and [[swelling]]
| |
|
| |
|
| [[Fever]]
| |
|
| |
|
| | style="background: #F5F5F5; padding: 5px;" | -
| | ==Initial Evaluation== |
| | colspan="2" style="background: #F5F5F5; padding: 5px;" | - | | {{familytree/start}} |
| | style="background: #F5F5F5; padding: 5px;" | -
| | {{Family tree |border=2|boxstyle=background: WhiteSmoke;| | | | | A01 | | | | |A01=<div style="float: left; text-align: center; height: 1.25em; width: 25em; padding: 1em;">'''Mediastinal Mass'''</div>}} |
| | style="background: #F5F5F5; padding: 5px;" | | | {{familytree | | | | | |!| | | | | | | | }} |
| * Defect in the abdominal wall muscles
| | {{familytree | | | | | B01 | | | |B01=<div style="float: left; text-align: left; line-height: 150%; padding: 1em; "> '''Workups''' |
| * Appearance of bowel loops within the lesion
| | ---- |
| * Lateral crescent sign
| | ❑ CT chest with contrast <br> ❑ Serum beta-HCG, AFP, if appropriate <br> ❑ CBC, platelets <br> ❑ PET-CT scan (optional) <br> ❑ Pulmonary function tests if clinically indicated <br> ❑ MRI chest if clinically indicated |
| * The hernia neck will be superolateral to the course of the inferior [[epigastric]] vessels.
| | </div>}} |
| *
| | {{familytree | |,|-|-|-|^|-|-|-|.| | | | | | | }} |
| | style="background: #F5F5F5; padding: 5px;" | | | {{familytree | C01 | | | | | | C02 | | | |C01=<div style="float: left; text-align: center; height: 1.25em; width: 15em; padding: 1em;"> '''Thymic Tumor Likely''' </div> |C02= <div style="float: left; text-align: center; height: 1.25em; width: 15em; padding: 1em;"> '''Thymic Tumor Unlikely''' </div>}} |
| | style="background: #F5F5F5; padding: 5px;" | | | {{familytree | |!| | | | | | | |!| | | | | }} |
| | style="background: #F5F5F5; padding: 5px;" | | | |
| | style="background: #F5F5F5; padding: 5px;" | | | {{familytree | D01 | | | | | | D02 | | | |D01=<div style="float: left; text-align: center; height: 1.25em; width: 15em; padding: 1em; text-size: 85%;">Consider [[Thymoma surgery|surgery]]</div>|D02=<div style="float: left; text-align: center; height: 1.25em; width: 15em; padding: 1em; text-size: 85%;">Disease-specific management</div>}} |
| |-
| | |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |
| | {{familytree/start}} |
| | style="background: #F5F5F5; padding: 5px;" |
| | |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |-
| |
| | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Endometriosis|Bowel endometriosis]]<ref name="pmid25400445">{{cite journal |vauthors=Wolthuis AM, Meuleman C, Tomassetti C, D'Hooghe T, de Buck van Overstraeten A, D'Hoore A |title=Bowel endometriosis: colorectal surgeon's perspective in a multidisciplinary surgical team |journal=World J. Gastroenterol. |volume=20 |issue=42 |pages=15616–23 |date=November 2014 |pmid=25400445 |pmc=4229526 |doi=10.3748/wjg.v20.i42.15616 |url=}}</ref>
| |
| | style="background: #F5F5F5; padding: 5px;" | | |
| * [[Constipation]]
| |
| and/or
| |
| * [[Diarrhea]]
| |
| | style="background: #F5F5F5; padding: 5px;" | + | |
| | style="background: #F5F5F5; padding: 5px;" | | |
| * Pelvic pain
| |
| | colspan="3" style="background: #F5F5F5; padding: 5px;" | | |
| * Dyschezia
| |
| * Tenesmus
| |
| | style="background: #F5F5F5; padding: 5px;" | +
| |
| | colspan="2" style="background: #F5F5F5; padding: 5px;" | -
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * N/A
| |
| | style="background: #F5F5F5; padding: 5px;" | | |
| * N/A
| |
| | style="background: #F5F5F5; padding: 5px;" | | |
| * Transvaginal ultrasonography: heterogeneous, hypoechoic, spiculated mass
| |
| * Barium enema: Extrinsic mass compressing the bowel, fine crenulation of the mucosa, bowel strictures at the rectosigmoid junction
| |
| * T1-weighted or fat-suppression T1-weighted MRIs: Contrast enhanced mass or hyperintense foci, hemorrhagic foci or hyperintense cavities
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| * N/A
| |
| | style="background: #F5F5F5; padding: 5px;" | | |
| * Transvaginal ultrasonography
| |
| | style="background: #F5F5F5; padding: 5px;" |
| |
| |}
| |
|
| |
|
| ==References== | | ==References== |
| {{Reflist|2}} | | {{Reflist|2}} |