Sandbox: Maria 13: Difference between revisions
(Created page with "__NOTOC__ {{SI}} {{CMG}} {{AE}} {{MV}} {{SK}} Juvenile nasopharyngeal angiofibroma; angiofibroma of the n...") |
No edit summary |
||
| (21 intermediate revisions by the same user not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}} {{AE}} {{MV}} | {{CMG}} {{AE}} {{MV}} | ||
{{SK}} Juvenile nasopharyngeal angiofibroma; angiofibroma of the nasopharynx; | {{SK}} Juvenile nasopharyngeal angiofibroma; angiofibroma of the nasopharynx; JNA | ||
==Overview== | ==Overview== | ||
'''Nasopharyngeal angiofibroma''' (also called juvenile nasopharyngeal angiofibroma) is a histologically [[benign]] but locally aggressive vascular tumor that grows in the back of the nasal cavity. It almost exclusively affects adolescent males. Patients with nasopharyngeal angiofibroma usually present with one-sided nasal obstruction and recurrent bleeding. | '''Nasopharyngeal angiofibroma''' (also called juvenile nasopharyngeal angiofibroma) is a histologically [[benign]] but locally aggressive vascular tumor that grows in the back of the nasal cavity. It almost exclusively affects adolescent males. Patients with nasopharyngeal angiofibroma usually present with one-sided nasal obstruction and recurrent bleeding. Nasopharyngeal angiofibroma may be classified according to Radkowski Classification System into 3 categories: I, II, and III. Nasopharyngeal angiofibroma is a vascular neoplasm, originates from the pterygopalatine fossa. The majority of nasopharyngeal angiofibromas are irrigated by the external carotid artery. Nasopharyngeal angiofibroma is rare, it account for 0.05% of all head and neck tumors. Nasopharyngeal angiofibromas are more commonly observed among children and adolescents. Common risk factors in the development of nasopharyngeal angiofibroma, include: | ||
presence of tumor in the pterygoid fossa and young age. Early clinical features include epistaxis, facial pain, and headache. The most common symptom is unilateral nasal obstruction. | |||
==Historical Perspective== | ==Historical Perspective== | ||
*Nasopharyngeal angiofibroma was first | *Nasopharyngeal angiofibroma was first described by Hippocrates, a Greek physician, in the 5th century BC. | ||
==Classification== | ==Classification== | ||
*Nasopharyngeal angiofibroma may be classified according to | *Nasopharyngeal angiofibroma may be classified according to Radkowski Classification System into 3 categories: | ||
:* | *'''Stage I''' | ||
:* | :*Ia: limited to nasal cavity/nasopharynx | ||
:* | :*Ib: extension into one or more paranasal sinuses | ||
* | *'''Stage II''' | ||
:*IIa: minimal extension through sphenopalatine foramen into pterygomaxillary fossa | |||
:*IIb: fills pterygomaxillary fossa bowing the posterior wall of the maxiallary antrum anteriorly or extending into the orbit via the inferior orbital fissure. | |||
:*IIc: extends beyond pterygomaxillary fossa into infratemporal fossa | |||
*'''Stage III''' | |||
:*Stage IIIA: intracranial extension | |||
==Pathophysiology== | ==Pathophysiology== | ||
*The pathogenesis of nasopharyngeal angiofibroma is characterized by | *The pathogenesis of nasopharyngeal angiofibroma is characterized by the following features:<ref name="pmid11374252">{{cite journal |vauthors=Paris J, Guelfucci B, Moulin G, Zanaret M, Triglia JM |title=Diagnosis and treatment of juvenile nasopharyngeal angiofibroma |journal=Eur Arch Otorhinolaryngol |volume=258 |issue=3 |pages=120–4 |year=2001 |pmid=11374252 |doi= |url=}}</ref> | ||
*The | :*Vascular neoplasm | ||
*On gross pathology, | :*Originates from the pterygopalatine fossa | ||
*On microscopic histopathological analysis, | :*The majority are associated with the external carotid artery | ||
*Genetic alterations associated with the development of nasopharyngeal angiofibroma, include:<ref name="pmid18228521">{{cite journal |vauthors=Coutinho-Camillo CM, Brentani MM, Nagai MA |title=Genetic alterations in juvenile nasopharyngeal angiofibromas |journal=Head Neck |volume=30 |issue=3 |pages=390–400 |year=2008 |pmid=18228521 |doi=10.1002/hed.20775 |url=}}</ref> | |||
:*Overexpression PDGF-B | |||
:*Overexpression bFGF | |||
:*Overexpression bFGF | |||
:*Deletion of chromosome 17 | |||
:*Tumor suppressor gene p53 | |||
:*Overexpression of Her-2/neu oncogene | |||
*On gross pathology, characteristic findings of nasopharyngeal angiofibroma, include: | |||
:*Unencapsulated | |||
:*Polypoid fibrous mass | |||
:*Bleeding on manipulation | |||
*On microscopic histopathological analysis, characteristic findings of nasopharyngeal angiofibroma, include: | |||
:*Fibroblastic cells with plump (near cuboidal) nuclei | |||
:*Fibrous stroma | |||
:*Abundant capillaries | |||
==Causes== | ==Causes== | ||
* | * There are no known causes of nasopharyngeal angiofibroma. | ||
==Differentiating Nasopharyngeal Angiofibroma from Other Diseases== | ==Differentiating Nasopharyngeal Angiofibroma from Other Diseases== | ||
*Nasopharyngeal angiofibroma must be differentiated from other diseases that cause | *Nasopharyngeal angiofibroma must be differentiated from other diseases that cause epistaxis, unilateral nasal obstruction, and rhinorrhea, such as: | ||
:* Antro-choanal polyp (antral-choanal polyp) | :* Antro-choanal polyp (antral-choanal polyp) | ||
:* Rhinosporidiosis | :* Rhinosporidiosis | ||
| Line 37: | Line 57: | ||
:* Nasopharanageal cyst | :* Nasopharanageal cyst | ||
:* Pyogenic granuloma | :* Pyogenic granuloma | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
* Nasopharyngeal angiofibroma is rare | |||
* Nasopharyngeal angiofibroma accounts for 0.05% of all head and neck tumors. | |||
* The prevalence of nasopharyngeal angiofibroma is approximately 1 per 100,000 individuals worldwide. | |||
===Age=== | ===Age=== | ||
| Line 48: | Line 68: | ||
===Gender=== | ===Gender=== | ||
*Males are more commonly affected with nasopharyngeal angiofibroma than females. | *Males are more commonly affected with nasopharyngeal angiofibroma than females. | ||
*The male to female ratio for nasopharyngeal angiofibroma is approximately 4 to 1. | *The male to female ratio for nasopharyngeal angiofibroma is approximately 4 to 1. | ||
| Line 54: | Line 73: | ||
===Race=== | ===Race=== | ||
*There is no racial predilection for nasopharyngeal angiofibroma. | *There is no racial predilection for nasopharyngeal angiofibroma. | ||
==Risk Factors== | ==Risk Factors== | ||
*Common risk factors in the development of nasopharyngeal angiofibroma | *Common risk factors in the development of nasopharyngeal angiofibroma, include:<ref name="pmid11374252">{{cite journal |vauthors=Paris J, Guelfucci B, Moulin G, Zanaret M, Triglia JM |title=Diagnosis and treatment of juvenile nasopharyngeal angiofibroma |journal=Eur Arch Otorhinolaryngol |volume=258 |issue=3 |pages=120–4 |year=2001 |pmid=11374252 |doi= |url=}}</ref> | ||
:*Presence of tumor in the pterygoid fossa | |||
:*Young age | |||
:*Feeders from the internal carotid artery | |||
:*Residual tumor | |||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
*The majority of patients with nasopharyngeal angiofibroma are symptomatic at diagnosis. | *The majority of patients with nasopharyngeal angiofibroma are symptomatic at diagnosis. | ||
*Early clinical features include epistaxis, facial pain, and headache. | *Early clinical features include epistaxis, facial pain, and headache. | ||
*If left untreated, the majority of patients with nasopharyngeal angiofibroma may progress to develop | *If left untreated, the majority of patients with nasopharyngeal angiofibroma may progress to develop malignant transformation. | ||
*Common complications of nasopharyngeal angiofibroma include transient blindness, optic nerve damage, and low-grade consumption coagulopathy. | |||
*Prognosis is generally good, and the 5-year survival rate of patients with early stage nasopharyngeal angiofibroma is approximately 90% | |||
*Survival rate of patients with late stage nasopharyngeal angiofibroma is approximately 40% | |||
== Diagnosis == | == Diagnosis == | ||
===Diagnostic Criteria=== | ===Diagnostic Criteria=== | ||
*The diagnosis of nasopharyngeal angiofibroma is | *The diagnosis of nasopharyngeal angiofibroma is with the following diagnostic criteria:<ref name="pmid11374252">{{cite journal |vauthors=Paris J, Guelfucci B, Moulin G, Zanaret M, Triglia JM |title=Diagnosis and treatment of juvenile nasopharyngeal angiofibroma |journal=Eur Arch Otorhinolaryngol |volume=258 |issue=3 |pages=120–4 |year=2001 |pmid=11374252 |doi= |url=}}</ref> | ||
:* | :*Clinical criteria | ||
:* | ::*Young patient | ||
:* | ::*Epistaxis | ||
:* | :*Positive physical exam | ||
::*A smooth submucosal mass in the posterior nasal cavity | |||
:*Positive imaging finding: visualisation of a nasopharyngeal mass | |||
=== Symptoms === | === Symptoms === | ||
*Common symptoms of nasopharyngeal angiofibroma, may include:<ref name="pmid11374252">{{cite journal |vauthors=Paris J, Guelfucci B, Moulin G, Zanaret M, Triglia JM |title=Diagnosis and treatment of juvenile nasopharyngeal angiofibroma |journal=Eur Arch Otorhinolaryngol |volume=258 |issue=3 |pages=120–4 |year=2001 |pmid=11374252 |doi= |url=}}</ref> | |||
*Common symptoms of nasopharyngeal angiofibroma, may include: | |||
:*Epistaxis or blood-tinged nasal discharge | :*Epistaxis or blood-tinged nasal discharge | ||
:*Unilateral nasal obstruction | |||
:*Rhinorrhea | :*Rhinorrhea | ||
:*Hearing loss | :*Hearing loss | ||
| Line 87: | Line 108: | ||
:*Rarely anosmia | :*Rarely anosmia | ||
:*Eye pain | :*Eye pain | ||
=== Physical Examination === | === Physical Examination === | ||
*Patients with nasopharyngeal angiofibroma usually are well-appearing. | *Patients with nasopharyngeal angiofibroma usually are well-appearing. | ||
*Physical examination may be remarkable for: | *Physical examination may be remarkable for: | ||
:* | :*A smooth submucosal mass in the posterior nasal cavity | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
* | *There are no specific laboratory findings associated with the diagnosis of nasopharyngeal angiofibroma. | ||
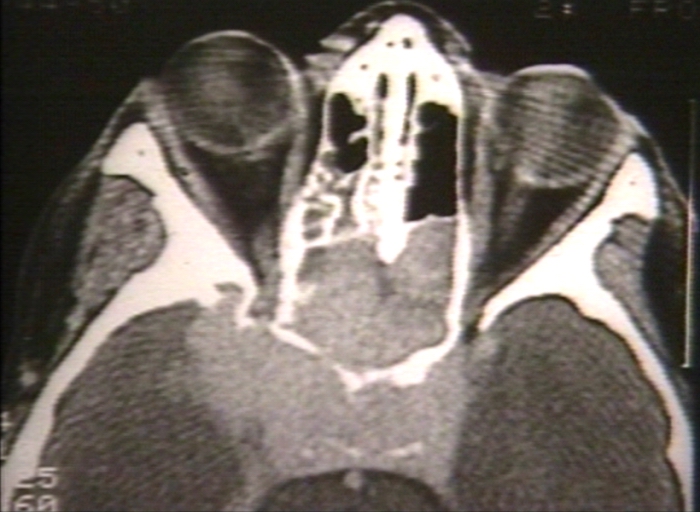
===Imaging Findings=== | ===Imaging Findings=== | ||
*Computed tomography is the imaging modality of choice for nasopharyngeal angiofibroma. | *Computed tomography is the imaging modality of choice for nasopharyngeal angiofibroma.<ref name="pmid11374252">{{cite journal |vauthors=Paris J, Guelfucci B, Moulin G, Zanaret M, Triglia JM |title=Diagnosis and treatment of juvenile nasopharyngeal angiofibroma |journal=Eur Arch Otorhinolaryngol |volume=258 |issue=3 |pages=120–4 |year=2001 |pmid=11374252 |doi= |url=}}</ref> | ||
*On conventional radiography, findings of nasopharyngeal angiofibroma, include: | |||
:*Visualisation of a nasopharyngeal mass | |||
:*Opacification of the sphenoid sinus | |||
:*Anterior bowing of the posterior wall of the maxillary antrum | |||
:*Holman-miller sign: the anterior bowing of the posterior wall of the maxillary antrum which is seen on lateral skull film or cross-sectional imaging | |||
:*Widening of the pterygomaxillary fissure and pterygopalatine fossa | |||
:*Erosion of the medial pterygoid plate | |||
*On CT, findings of nasopharyngeal angiofibroma, include: | *On CT, findings of nasopharyngeal angiofibroma, include: | ||
:* | :*Bony changes | ||
:* | :*Non-encapsulated soft tissue mass | ||
:* | :*Bowing the posterior wall of the maxillary antrum anteriorly | ||
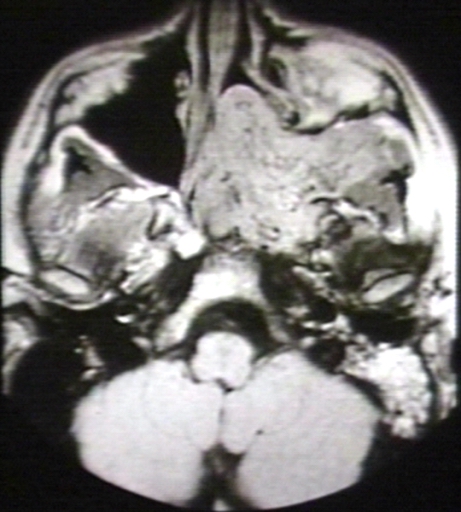
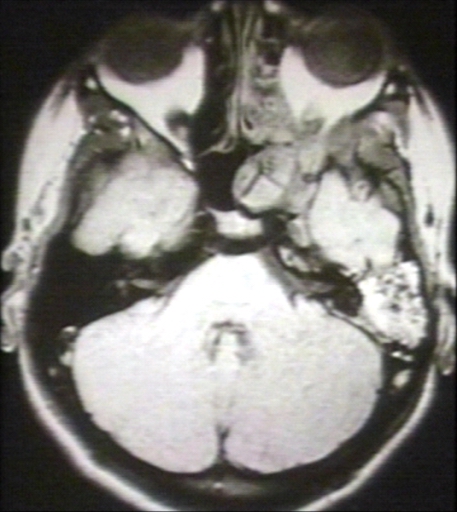
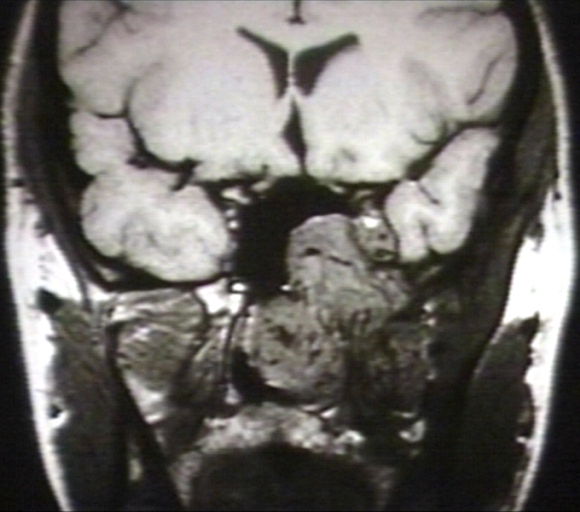
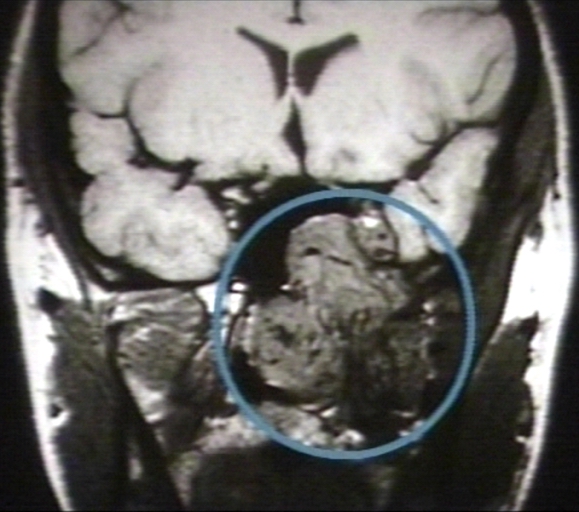
*On MRI, findings of nasopharyngeal angiofibroma, include: | *On MRI, findings of nasopharyngeal angiofibroma, include: | ||
:* | :*T1: intermediate signal | ||
:* | :*T2: heterogeneous signal: flow voids appear dark | ||
:* | :*T1 C+ (Gd): shows prominent enhancement | ||
*The images below demonstrate findings of nasopharyngeal angiofibroma. | *The images below demonstrate findings of nasopharyngeal angiofibroma. | ||
<gallery> | <gallery> | ||
Image:Nasopharyngeal angiofibroma 001.jpg| | Image:Nasopharyngeal angiofibroma 001.jpg| Nasopharyngeal angiofibroma. Skull base invasion[http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | ||
Image:Nasopharyngeal angiofibroma 002.jpg | Image:Nasopharyngeal angiofibroma 002.jpg|MRI (T1): Nasopharyngeal angiofibroma 1/3 [http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | ||
Image:Nasopharyngeal angiofibroma 003.jpg | Image:Nasopharyngeal angiofibroma 003.jpg| MRI (T1): Nasopharyngeal angiofibroma [http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | ||
Image:Nasopharyngeal angiofibroma 004.jpg | Image:Nasopharyngeal angiofibroma 004.jpg| MRI (T1): Nasopharyngeal angiofibroma 3/3 [http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | ||
Image:Nasopharyngeal angiofibroma 005.jpg | Image:Nasopharyngeal angiofibroma 005.jpg| MRI (T1): Nasopharyngeal angiofibroma 3/3 (circled)[http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | ||
</gallery> | </gallery> | ||
=== Other Diagnostic Studies === | === Other Diagnostic Studies === | ||
*Nasopharyngeal angiofibroma may also be diagnosed using [ | *Nasopharyngeal angiofibroma may also be diagnosed using nasal [[endoscopy]]. | ||
== Treatment == | == Treatment == | ||
=== Medical Therapy === | === Medical Therapy === | ||
* | *Medical therapy for nasopharyngeal angiofibroma is divided into 2 categories:<ref name="pmid11374252">{{cite journal |vauthors=Paris J, Guelfucci B, Moulin G, Zanaret M, Triglia JM |title=Diagnosis and treatment of juvenile nasopharyngeal angiofibroma |journal=Eur Arch Otorhinolaryngol |volume=258 |issue=3 |pages=120–4 |year=2001 |pmid=11374252 |doi= |url=}}</ref> | ||
:*Hormonal therapy | |||
* | :*Radiotherapy | ||
* | *Hormonal therapy for nasopharyngeal angiofibroma, includes: | ||
* | :*Flutamide | ||
*Medical treatment is usually given before surgery to reduce the blood loss | |||
*Radiotherapy for nasopharyngeal angiofibroma, include: | |||
:*Stereotactic radiotherapy | |||
=== Surgery === | === Surgery === | ||
*Surgery is the mainstay of therapy for nasopharyngeal angiofibroma. | *Surgery is the mainstay of therapy for nasopharyngeal angiofibroma. | ||
* | *Surgical approach for nasopharyngeal angiofibroma will depend on the stage. | ||
* | :*The treatment of choice for early stage for nasopharyngeal angiofibroma is intranasal endoscopic surgery. Lateral rhinotomy is the usual preferred surgical approach of choice. | ||
:*The treatment of choice for late stage for nasopharyngeal angiofibroma include the infratemporal fossa approach, and the mid-facial degloving approach. | |||
=== Prevention === | === Prevention === | ||
*There are no primary preventive measures available for nasopharyngeal angiofibroma. | *There are no primary preventive measures available for nasopharyngeal angiofibroma. | ||
*Once diagnosed and successfully treated, patients with nasopharyngeal angiofibroma are followed-up after surgery, and every 3, 6, or 12 months. | |||
*Once diagnosed and successfully treated, patients with nasopharyngeal angiofibroma are followed-up every | |||
==References== | ==References== | ||
Latest revision as of 14:26, 15 April 2016
|
WikiDoc Resources for Sandbox: Maria 13 |
|
Articles |
|---|
|
Most recent articles on Sandbox: Maria 13 Most cited articles on Sandbox: Maria 13 |
|
Media |
|
Powerpoint slides on Sandbox: Maria 13 |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Sandbox: Maria 13 |
|
Clinical Trials |
|
Ongoing Trials on Sandbox: Maria 13 at Clinical Trials.gov Trial results on Sandbox: Maria 13 Clinical Trials on Sandbox: Maria 13 at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Sandbox: Maria 13 NICE Guidance on Sandbox: Maria 13
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Sandbox: Maria 13 Discussion groups on Sandbox: Maria 13 Patient Handouts on Sandbox: Maria 13 Directions to Hospitals Treating Sandbox: Maria 13 Risk calculators and risk factors for Sandbox: Maria 13
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Sandbox: Maria 13 |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Maria Fernanda Villarreal, M.D. [2]
Synonyms and keywords: Juvenile nasopharyngeal angiofibroma; angiofibroma of the nasopharynx; JNA
Overview
Nasopharyngeal angiofibroma (also called juvenile nasopharyngeal angiofibroma) is a histologically benign but locally aggressive vascular tumor that grows in the back of the nasal cavity. It almost exclusively affects adolescent males. Patients with nasopharyngeal angiofibroma usually present with one-sided nasal obstruction and recurrent bleeding. Nasopharyngeal angiofibroma may be classified according to Radkowski Classification System into 3 categories: I, II, and III. Nasopharyngeal angiofibroma is a vascular neoplasm, originates from the pterygopalatine fossa. The majority of nasopharyngeal angiofibromas are irrigated by the external carotid artery. Nasopharyngeal angiofibroma is rare, it account for 0.05% of all head and neck tumors. Nasopharyngeal angiofibromas are more commonly observed among children and adolescents. Common risk factors in the development of nasopharyngeal angiofibroma, include: presence of tumor in the pterygoid fossa and young age. Early clinical features include epistaxis, facial pain, and headache. The most common symptom is unilateral nasal obstruction.
Historical Perspective
- Nasopharyngeal angiofibroma was first described by Hippocrates, a Greek physician, in the 5th century BC.
Classification
- Nasopharyngeal angiofibroma may be classified according to Radkowski Classification System into 3 categories:
- Stage I
- Ia: limited to nasal cavity/nasopharynx
- Ib: extension into one or more paranasal sinuses
- Stage II
- IIa: minimal extension through sphenopalatine foramen into pterygomaxillary fossa
- IIb: fills pterygomaxillary fossa bowing the posterior wall of the maxiallary antrum anteriorly or extending into the orbit via the inferior orbital fissure.
- IIc: extends beyond pterygomaxillary fossa into infratemporal fossa
- Stage III
- Stage IIIA: intracranial extension
Pathophysiology
- The pathogenesis of nasopharyngeal angiofibroma is characterized by the following features:[1]
- Vascular neoplasm
- Originates from the pterygopalatine fossa
- The majority are associated with the external carotid artery
- Genetic alterations associated with the development of nasopharyngeal angiofibroma, include:[2]
- Overexpression PDGF-B
- Overexpression bFGF
- Overexpression bFGF
- Deletion of chromosome 17
- Tumor suppressor gene p53
- Overexpression of Her-2/neu oncogene
- On gross pathology, characteristic findings of nasopharyngeal angiofibroma, include:
- Unencapsulated
- Polypoid fibrous mass
- Bleeding on manipulation
- On microscopic histopathological analysis, characteristic findings of nasopharyngeal angiofibroma, include:
- Fibroblastic cells with plump (near cuboidal) nuclei
- Fibrous stroma
- Abundant capillaries
Causes
- There are no known causes of nasopharyngeal angiofibroma.
Differentiating Nasopharyngeal Angiofibroma from Other Diseases
- Nasopharyngeal angiofibroma must be differentiated from other diseases that cause epistaxis, unilateral nasal obstruction, and rhinorrhea, such as:
- Antro-choanal polyp (antral-choanal polyp)
- Rhinosporidiosis
- Malignancy
- Chordoma
- Nasopharanageal cyst
- Pyogenic granuloma
Epidemiology and Demographics
- Nasopharyngeal angiofibroma is rare
- Nasopharyngeal angiofibroma accounts for 0.05% of all head and neck tumors.
- The prevalence of nasopharyngeal angiofibroma is approximately 1 per 100,000 individuals worldwide.
Age
- Nasopharyngeal angiofibroma is more commonly observed among patients aged 7-19 years
- Nasopharyngeal angiofibroma is more commonly observed among children and adolescents .
Gender
- Males are more commonly affected with nasopharyngeal angiofibroma than females.
- The male to female ratio for nasopharyngeal angiofibroma is approximately 4 to 1.
Race
- There is no racial predilection for nasopharyngeal angiofibroma.
Risk Factors
- Common risk factors in the development of nasopharyngeal angiofibroma, include:[1]
- Presence of tumor in the pterygoid fossa
- Young age
- Feeders from the internal carotid artery
- Residual tumor
Natural History, Complications and Prognosis
- The majority of patients with nasopharyngeal angiofibroma are symptomatic at diagnosis.
- Early clinical features include epistaxis, facial pain, and headache.
- If left untreated, the majority of patients with nasopharyngeal angiofibroma may progress to develop malignant transformation.
- Common complications of nasopharyngeal angiofibroma include transient blindness, optic nerve damage, and low-grade consumption coagulopathy.
- Prognosis is generally good, and the 5-year survival rate of patients with early stage nasopharyngeal angiofibroma is approximately 90%
- Survival rate of patients with late stage nasopharyngeal angiofibroma is approximately 40%
Diagnosis
Diagnostic Criteria
- The diagnosis of nasopharyngeal angiofibroma is with the following diagnostic criteria:[1]
- Clinical criteria
- Young patient
- Epistaxis
- Positive physical exam
- A smooth submucosal mass in the posterior nasal cavity
- Positive imaging finding: visualisation of a nasopharyngeal mass
Symptoms
- Common symptoms of nasopharyngeal angiofibroma, may include:[1]
- Epistaxis or blood-tinged nasal discharge
- Unilateral nasal obstruction
- Rhinorrhea
- Hearing loss
- Diplopia
- Rarely anosmia
- Eye pain
Physical Examination
- Patients with nasopharyngeal angiofibroma usually are well-appearing.
- Physical examination may be remarkable for:
- A smooth submucosal mass in the posterior nasal cavity
Laboratory Findings
- There are no specific laboratory findings associated with the diagnosis of nasopharyngeal angiofibroma.
Imaging Findings
- Computed tomography is the imaging modality of choice for nasopharyngeal angiofibroma.[1]
- On conventional radiography, findings of nasopharyngeal angiofibroma, include:
- Visualisation of a nasopharyngeal mass
- Opacification of the sphenoid sinus
- Anterior bowing of the posterior wall of the maxillary antrum
- Holman-miller sign: the anterior bowing of the posterior wall of the maxillary antrum which is seen on lateral skull film or cross-sectional imaging
- Widening of the pterygomaxillary fissure and pterygopalatine fossa
- Erosion of the medial pterygoid plate
- On CT, findings of nasopharyngeal angiofibroma, include:
- Bony changes
- Non-encapsulated soft tissue mass
- Bowing the posterior wall of the maxillary antrum anteriorly
- On MRI, findings of nasopharyngeal angiofibroma, include:
- T1: intermediate signal
- T2: heterogeneous signal: flow voids appear dark
- T1 C+ (Gd): shows prominent enhancement
- The images below demonstrate findings of nasopharyngeal angiofibroma.
-
Nasopharyngeal angiofibroma. Skull base invasionImage courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma 1/3 Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma 3/3 Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma 3/3 (circled)Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
Other Diagnostic Studies
- Nasopharyngeal angiofibroma may also be diagnosed using nasal endoscopy.
Treatment
Medical Therapy
- Medical therapy for nasopharyngeal angiofibroma is divided into 2 categories:[1]
- Hormonal therapy
- Radiotherapy
- Hormonal therapy for nasopharyngeal angiofibroma, includes:
- Flutamide
- Medical treatment is usually given before surgery to reduce the blood loss
- Radiotherapy for nasopharyngeal angiofibroma, include:
- Stereotactic radiotherapy
Surgery
- Surgery is the mainstay of therapy for nasopharyngeal angiofibroma.
- Surgical approach for nasopharyngeal angiofibroma will depend on the stage.
- The treatment of choice for early stage for nasopharyngeal angiofibroma is intranasal endoscopic surgery. Lateral rhinotomy is the usual preferred surgical approach of choice.
- The treatment of choice for late stage for nasopharyngeal angiofibroma include the infratemporal fossa approach, and the mid-facial degloving approach.
Prevention
- There are no primary preventive measures available for nasopharyngeal angiofibroma.
- Once diagnosed and successfully treated, patients with nasopharyngeal angiofibroma are followed-up after surgery, and every 3, 6, or 12 months.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Paris J, Guelfucci B, Moulin G, Zanaret M, Triglia JM (2001). "Diagnosis and treatment of juvenile nasopharyngeal angiofibroma". Eur Arch Otorhinolaryngol. 258 (3): 120–4. PMID 11374252.
- ↑ Coutinho-Camillo CM, Brentani MM, Nagai MA (2008). "Genetic alterations in juvenile nasopharyngeal angiofibromas". Head Neck. 30 (3): 390–400. doi:10.1002/hed.20775. PMID 18228521.