Sandbox: Maria 13
|
WikiDoc Resources for Sandbox: Maria 13 |
|
Articles |
|---|
|
Most recent articles on Sandbox: Maria 13 Most cited articles on Sandbox: Maria 13 |
|
Media |
|
Powerpoint slides on Sandbox: Maria 13 |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Sandbox: Maria 13 |
|
Clinical Trials |
|
Ongoing Trials on Sandbox: Maria 13 at Clinical Trials.gov Trial results on Sandbox: Maria 13 Clinical Trials on Sandbox: Maria 13 at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Sandbox: Maria 13 NICE Guidance on Sandbox: Maria 13
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Sandbox: Maria 13 Discussion groups on Sandbox: Maria 13 Patient Handouts on Sandbox: Maria 13 Directions to Hospitals Treating Sandbox: Maria 13 Risk calculators and risk factors for Sandbox: Maria 13
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Sandbox: Maria 13 |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Maria Fernanda Villarreal, M.D. [2]
Synonyms and keywords: Juvenile nasopharyngeal angiofibroma; angiofibroma of the nasopharynx; JNA
Overview
Nasopharyngeal angiofibroma (also called juvenile nasopharyngeal angiofibroma) is a histologically benign but locally aggressive vascular tumor that grows in the back of the nasal cavity. It almost exclusively affects adolescent males. Patients with nasopharyngeal angiofibroma usually present with one-sided nasal obstruction and recurrent bleeding. Nasopharyngeal angiofibroma may be classified according to Radkowski Classification System into 3 categories: I, II, and III. Nasopharyngeal angiofibroma is a vascular neoplasm, originates from the pterygopalatine fossa. The majority of nasopharyngeal angiofibromas are irrigated by the external carotid artery. Nasopharyngeal angiofibroma is rare, it account for 0.05% of all head and neck tumors. Nasopharyngeal angiofibromas are more commonly observed among children and adolescents. Common risk factors in the development of nasopharyngeal angiofibroma, include: presence of tumor in the pterygoid fossa and young age. Early clinical features include epistaxis, facial pain, and headache. The most common symptom is unilateral nasal obstruction.
Historical Perspective
- Nasopharyngeal angiofibroma was first described by Hippocrates, a Greek physician, in the 5th century BC.
Classification
- Nasopharyngeal angiofibroma may be classified according to Radkowski Classification System into 3 categories:
- Stage I
- Ia: limited to nasal cavity/nasopharynx
- Ib: extension into one or more paranasal sinuses
- Stage II
- IIa: minimal extension through sphenopalatine foramen into pterygomaxillary fossa
- IIb: fills pterygomaxillary fossa bowing the posterior wall of the maxiallary antrum anteriorly or extending into the orbit via the inferior orbital fissure.
- IIc: extends beyond pterygomaxillary fossa into infratemporal fossa
- Stage III
- Stage IIIA: intracranial extension
Pathophysiology
- The pathogenesis of nasopharyngeal angiofibroma is characterized by the following features:[1]
- Vascular neoplasm
- Originates from the pterygopalatine fossa
- The majority are associated with the external carotid artery
- Genetic alterations associated with the development of nasopharyngeal angiofibroma, include:[2]
- Overexpression PDGF-B
- Overexpression bFGF
- Overexpression bFGF
- Deletion of chromosome 17
- Tumor suppressor gene p53
- Overexpression of Her-2/neu oncogene
- On gross pathology, characteristic findings of nasopharyngeal angiofibroma, include:
- Unencapsulated
- Polypoid fibrous mass
- Bleeding on manipulation
- On microscopic histopathological analysis, characteristic findings of nasopharyngeal angiofibroma, include:
- Fibroblastic cells with plump (near cuboidal) nuclei
- Fibrous stroma
- Abundant capillaries
Causes
- There are no known causes of nasopharyngeal angiofibroma.
Differentiating Nasopharyngeal Angiofibroma from Other Diseases
- Nasopharyngeal angiofibroma must be differentiated from other diseases that cause epistaxis, unilateral nasal obstruction, and rhinorrhea, such as:
- Antro-choanal polyp (antral-choanal polyp)
- Rhinosporidiosis
- Malignancy
- Chordoma
- Nasopharanageal cyst
- Pyogenic granuloma
Epidemiology and Demographics
- Nasopharyngeal angiofibroma is rare
- Nasopharyngeal angiofibroma accounts for 0.05% of all head and neck tumors.
- The prevalence of nasopharyngeal angiofibroma is approximately 1 per 100,000 individuals worldwide.
Age
- Nasopharyngeal angiofibroma is more commonly observed among patients aged 7-19 years
- Nasopharyngeal angiofibroma is more commonly observed among children and adolescents .
Gender
- Males are more commonly affected with nasopharyngeal angiofibroma than females.
- The male to female ratio for nasopharyngeal angiofibroma is approximately 4 to 1.
Race
- There is no racial predilection for nasopharyngeal angiofibroma.
Risk Factors
- Common risk factors in the development of nasopharyngeal angiofibroma, include:[1]
- Presence of tumor in the pterygoid fossa
- Young age
- Feeders from the internal carotid artery
- Residual tumor
Natural History, Complications and Prognosis
- The majority of patients with nasopharyngeal angiofibroma are symptomatic at diagnosis.
- Early clinical features include epistaxis, facial pain, and headache.
- If left untreated, the majority of patients with nasopharyngeal angiofibroma may progress to develop malignant transformation.
- Common complications of nasopharyngeal angiofibroma include transient blindness, optic nerve damage, and low-grade consumption coagulopathy.
- Prognosis is generally good, and the 5-year survival rate of patients with early stage nasopharyngeal angiofibroma is approximately 90%
- Survival rate of patients with late stage nasopharyngeal angiofibroma is approximately 40%
Diagnosis
Diagnostic Criteria
- The diagnosis of nasopharyngeal angiofibroma is with the following diagnostic criteria:[1]
- Clinical criteria
- Young patient
- Epistaxis
- Positive physical exam
- A smooth submucosal mass in the posterior nasal cavity
- Positive imaging finding: visualisation of a nasopharyngeal mass
Symptoms
- Common symptoms of nasopharyngeal angiofibroma, may include:[1]
- Epistaxis or blood-tinged nasal discharge
- Unilateral nasal obstruction
- Rhinorrhea
- Hearing loss
- Diplopia
- Rarely anosmia
- Eye pain
Physical Examination
- Patients with nasopharyngeal angiofibroma usually are well-appearing.
- Physical examination may be remarkable for:
- A smooth submucosal mass in the posterior nasal cavity
Laboratory Findings
- There are no specific laboratory findings associated with the diagnosis of nasopharyngeal angiofibroma.
Imaging Findings
- Computed tomography is the imaging modality of choice for nasopharyngeal angiofibroma.[1]
- On conventional radiography, findings of nasopharyngeal angiofibroma, include:
- Visualisation of a nasopharyngeal mass
- Opacification of the sphenoid sinus
- Anterior bowing of the posterior wall of the maxillary antrum
- Holman-miller sign: the anterior bowing of the posterior wall of the maxillary antrum which is seen on lateral skull film or cross-sectional imaging
- Widening of the pterygomaxillary fissure and pterygopalatine fossa
- Erosion of the medial pterygoid plate
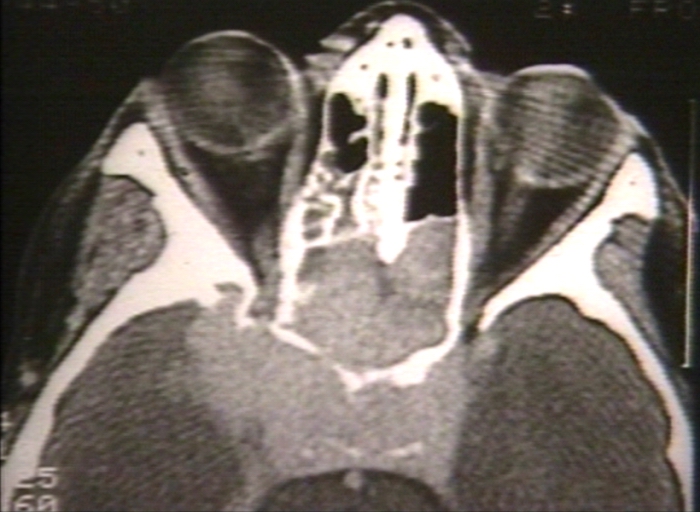
- On CT, findings of nasopharyngeal angiofibroma, include:
- Bony changes
- Non-encapsulated soft tissue mass
- Bowing the posterior wall of the maxillary antrum anteriorly
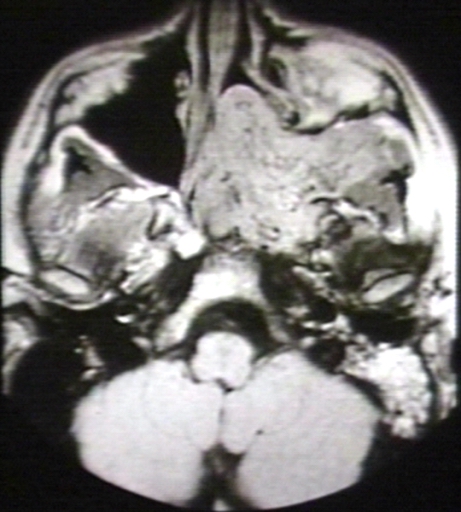
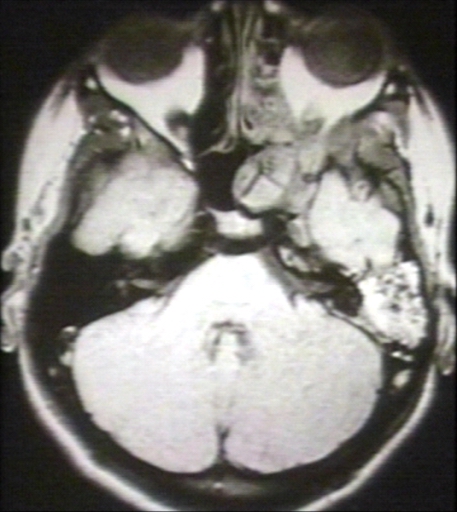
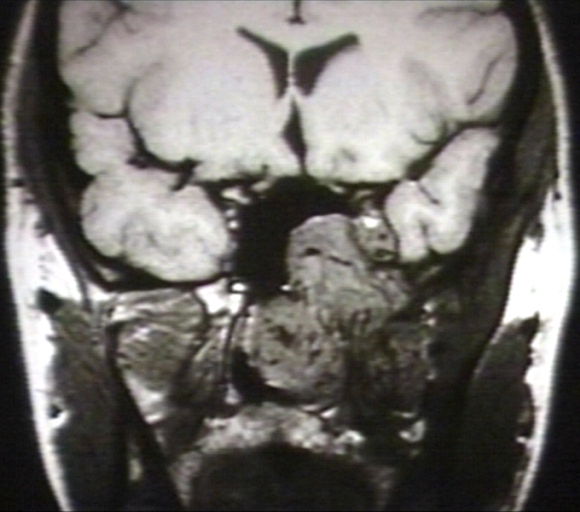
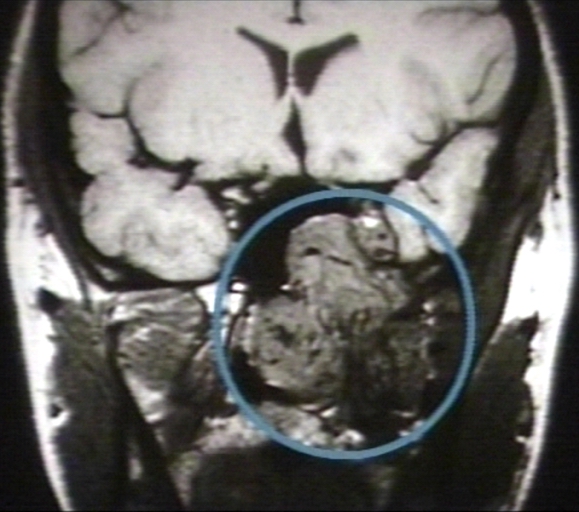
- On MRI, findings of nasopharyngeal angiofibroma, include:
- T1: intermediate signal
- T2: heterogeneous signal: flow voids appear dark
- T1 C+ (Gd): shows prominent enhancement
- The images below demonstrate findings of nasopharyngeal angiofibroma.
-
Nasopharyngeal angiofibroma. Skull base invasionImage courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma 1/3 Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma 3/3 Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma 3/3 (circled)Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
Other Diagnostic Studies
- Nasopharyngeal angiofibroma may also be diagnosed using nasal endoscopy.
Treatment
Medical Therapy
- Medical therapy for nasopharyngeal angiofibroma is divided into 2 categories:[1]
- Hormonal therapy
- Radiotherapy
- Hormonal therapy for nasopharyngeal angiofibroma, includes:
- Flutamide
- Medical treatment is usually given before surgery to reduce the blood loss
- Radiotherapy for nasopharyngeal angiofibroma, include:
- Stereotactic radiotherapy
Surgery
- Surgery is the mainstay of therapy for nasopharyngeal angiofibroma.
- Surgical approach for nasopharyngeal angiofibroma will depend on the stage.
- The treatment of choice for early stage for nasopharyngeal angiofibroma is intranasal endoscopic surgery. Lateral rhinotomy is the usual preferred surgical approach of choice.
- The treatment of choice for late stage for nasopharyngeal angiofibroma include the infratemporal fossa approach, and the mid-facial degloving approach.
Prevention
- There are no primary preventive measures available for nasopharyngeal angiofibroma.
- Once diagnosed and successfully treated, patients with nasopharyngeal angiofibroma are followed-up after surgery, and every 3, 6, or 12 months.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Paris J, Guelfucci B, Moulin G, Zanaret M, Triglia JM (2001). "Diagnosis and treatment of juvenile nasopharyngeal angiofibroma". Eur Arch Otorhinolaryngol. 258 (3): 120–4. PMID 11374252.
- ↑ Coutinho-Camillo CM, Brentani MM, Nagai MA (2008). "Genetic alterations in juvenile nasopharyngeal angiofibromas". Head Neck. 30 (3): 390–400. doi:10.1002/hed.20775. PMID 18228521.