Quadrilateral Space Syndrome
Editor in Chief: Elliot B Tapper, MD. Department of Medicine Beth Israel Deaconess Medical Center
Introduction and Overview
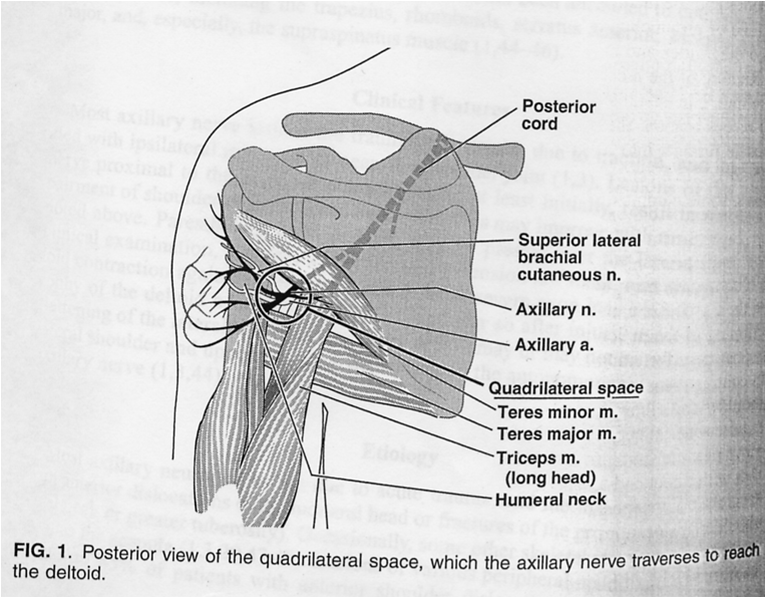
The Quadrilateral Space Syndrome (QSS) is a complex of shoulder pain and parasthesias found in approximately 0.8% of patients with a shoulder pain complaint. Predominantly, it is an affliction of middle aged men and it presents classically in the throwing athlete and those with a history rotator cuff surgery. QSS was uncovered in patients with a supposed thoracic outlet syndrome for whom surgery provided poor results. Bernard Cahill, an Orthopaedic surgeon and pioneer of sports medicine, found in these cases a common link: a compression of the posterior humeral circumflex artery (PHCA), specifically during abduction and external rotation of the humerus on physical exam. After deeper investigation, Cahill reported with Palmer in 1983 that the syndrome was caused by compression in the quadrilateral space of the PHCA and the axillary nerve, or one if its major branches.[1]
Pathophysiology
At the centre of the patient presentation are symptoms with respect to functions related to the teres minor. It is a component of the rotator cuff and it originates on the dorsal surface of the axillary border of the scapula, inserting on the greater tubercle of the humerus. Its innervation is from the axillary nerve (C5, C6), its blood is supplied by the axillary artery vis-à-vis the PHCA and its functions are external rotation, adduction and extension of the humerus.
It is from within this space that muscular hypertrophy or, more commonly, fibrous bands cause the compression of the artery and/or nerve that yield the clinical presentation. Typically, the patient with QSS will complain of a pain localized over the QS, a diffuse and non-dermatomal pain anteriorly as well as posteriorly, intermittent claudication after sustained abduction or external rotation and often parasthesias over the lateral aspect of the shoulder. Indeed the classic aggravating factors are external rotation and abduction.
Diagnosis
Since the first description of QSS, the emphasis has always been on diagnosis. Given its rarity and peculiar presentation, the potential is real for either misdiagnosis or misattribution to the psychosomatic. Modalities at our disposal include ultrasound, MRI, EMG/NCS and arteriography.
Cahill and Palmer themselves suggested diagnosis by subclavian arteriogram. The procedure is the same as if one were attempting to diagnose of thoracic outlet syndrome, simply following the dye out to the PHCA. And it is in this territory that occlusion is seen but only upon abduction and external rotation of the humerus. Of course, while this test may provide direct evidence, it is invasive and may miss the cases of pure nerve entrapment. Furthermore, angiography is unacceptably unnspecifc. One study describes occlusion of the PHCA in 80% of healthy volunteers, a finding that may highlight as causal the nervous, rather than vascular, pathology.[3]

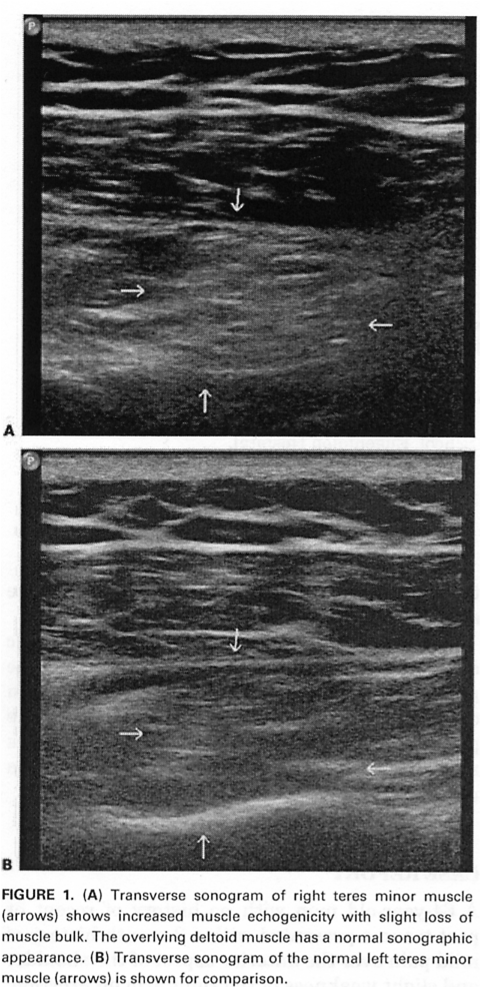
While ultrasound is the least useful modality, detecting change only at stages far more advanced than MRI, it is worth discussing briefly for an enhanced understanding of the pathology. Not only can ultrasound show arterial occlusion (by colour doppler) in a less invasive fashion than arteriography, it can also diagnose by increased echogenicity the atrophy of teres minor. Depicted below is the right teres minor in a case of QSS that is notably atrophied in comparison to both the left teres minor and the overlying deltoid.[4]
Magnetic resonance with or without angiography can tell us the same information but has the advantage of detecting denervation earliest. Indeed, the earliest sign of neurogenic muscle atrophy is edema and that can be detected as increased signal intensity on T2 sequences. Moreover, the MRI can further distinguish between acute and chronic atrophy as chronic denervation will appear with increased intensity on spin-echo sequences. Indeed, the basic diagnostic criteria by MRI involve identifying the combination of disproportionate volume loss or fatty infiltration of the teres minor in comparison to the other rotator cuff muscles with the increased T2 signal of neurogenic edema.[5]
Treatment
Given the diagnosis, the treatment is at first conservative with a trial of analgesics, physiotherapy, and avoidance of athletic activities.[6] Physiotherapy should include the application “cross friction” (moving the skin against the grain of muscle tissue) and active release soft tissue massage techniques to the QS, internal mobilization of the humerus, stretching into horizontal adduction and internal rotation, and posterior rotator cuff strengthening.[7]
If the pain is severe or if the patient fails conservative measurement then one might opt for surgical decompression. The best series in the literature is in fact Cahill and Palmer’s first for which there was a post-surgical success rate of 44%. In this surgery, the teres minor is detached at its insertion into the rotator cuff and reflected medially. The QS is then decompressed by blunt and sharp dissection followed by a more careful dissection of the fibrous bands about the neurovascular bundle beginning from the origin of the PHCA at the axillary artery.
References
- ↑ Cahill and Palmer. Quadrilateral Space Syndrome. J Hand Surg 1983. Vol 8(1):65-69
- ↑ Dawson. Entrapment Neuropathies 3rd Edition. Lippincott-Raven. Chapters 13, 16.
- ↑ Mochizuki et al. Occlusion of the posterior humeral circumflex artery: detection with MR angiography in healthy volunteers and in a patient with quadrilateral space syndrome. AJR 1994; 163: 625-627
- ↑ Brestas et al. Ultrasound findings of Teres Minor Denervation in Suspected QSS. J Clin Ultrasound 2006;34:343-7
- ↑ Cothran and Helms. QSS: Incidence of Imaging Findings in a Population Referred for MRI of the Shoulder. AJR 2005;184:989-92
- ↑ Paladini et al. Axillary Neuropathy in Volleyball Players: Report of Two Cases and Literature Review. JNNP 1996;60:345-7
- ↑ Hoskins et al. Quadrilateral space syndrome: a case study and review of the literature. Br J Sports Med 2005;39;9-10