Micafungin adverse reactions
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ahmed Zaghw, M.D. [2]
Adverse Reactions
The overall safety of Mycamine was assessed in 3227 adult and pediatric patients and 520 volunteers in 46 clinical trials, including the invasive candidiasis, esophageal candidiasis and prophylaxis trials, who received single or multiple doses of Mycamine, ranging from 0.75 mg/kg to 10 mg/kg in pediatric patients and 12.5 mg to 150 mg/day or greater in adult patients.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of Mycamine cannot be directly compared to rates in clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does provide a basis for identifying adverse events that appear to be related to drug use and for approximating rates.
Infusion Reactions
Possible histamine-mediated symptoms have been reported with Mycamine, including rash, pruritus, facial swelling, and vasodilatation.
Injection site reactions, including phlebitis and thrombophlebitis have been reported, at Mycamine doses of 50-150 mg/day. These reactions tended to occur more often in patients receiving Mycamine via peripheral intravenous administration.
Clinical Trials Experience in Adults
In all clinical trials with Mycamine, 2497/2748 (91%) adult patients experienced at least one treatment-emergent adverse reaction.
Candidemia and Other Candida InfectionsIn a randomized, double-blind study for treatment of candidemia and other Candida infections, treatment-emergent adverse reactions occurred in 183/200 (92%), 187/202 (93%) and 171/193 (89%) patients in the Mycamine 100 mg/day, Mycamine 150 mg/day, and caspofungin (a 70 mg loading dose followed by a 50 mg/day dose) treatment groups, respectively. Selected treatment-emergent adverse reactions, those occurring in 5% or more of the patients and more frequently in a Mycamine treatment group, are shown inTable 3.[1]
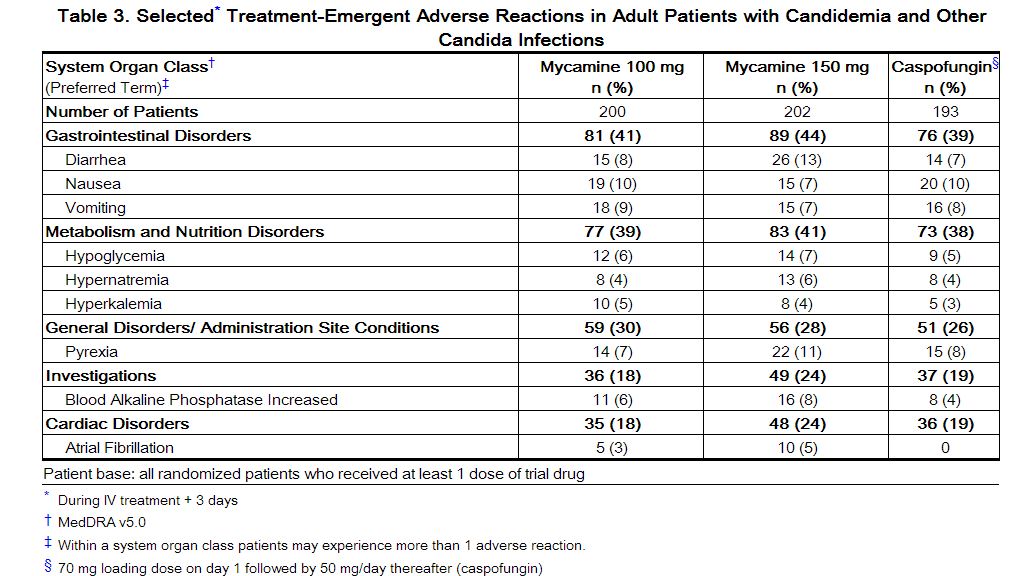 |
In a second, supportive, randomized, double-blind study for treatment of candidemia and other Candidainfections, treatment-emergent adverse reactions occurred in 245/264 (93%) and 250/265 (94%) patients in the Mycamine (100 mg/day) and AmBisome (3 mg/kg/day) treatment groups, respectively. The following treatment-emergent adverse reactions in the Mycamine treated patients at least 16 years of age were notable: nausea (10% vs. 8%); diarrhea (11% vs. 11%), vomiting (13% vs. 9%), abnormal liver function tests (4% vs. 3%); increased aspartate aminotransferase (3% vs. 2%), and increased blood alkaline phosphatase (3% vs. 2%), in the Mycamine and AmBisome treatment groups, respectively.
Esophageal Candidiasis
In a randomized, double-blind study for treatment of esophageal candidiasis, a total of 202/260 (78%) patients who received Mycamine 150 mg/day and 186/258 (72%) patients who received intravenous fluconazole 200 mg/day experienced an adverse reaction. Treatment-emergent adverse reactions resulting in discontinuation were reported in 17 (7%) Mycamine treated patients; and in 12 (5%) fluconazole treated patients. Selected treatment-emergent adverse reactions, those occurring in 5% or more of the patients and more frequently in the Mycamine group, are shown in Table 4.
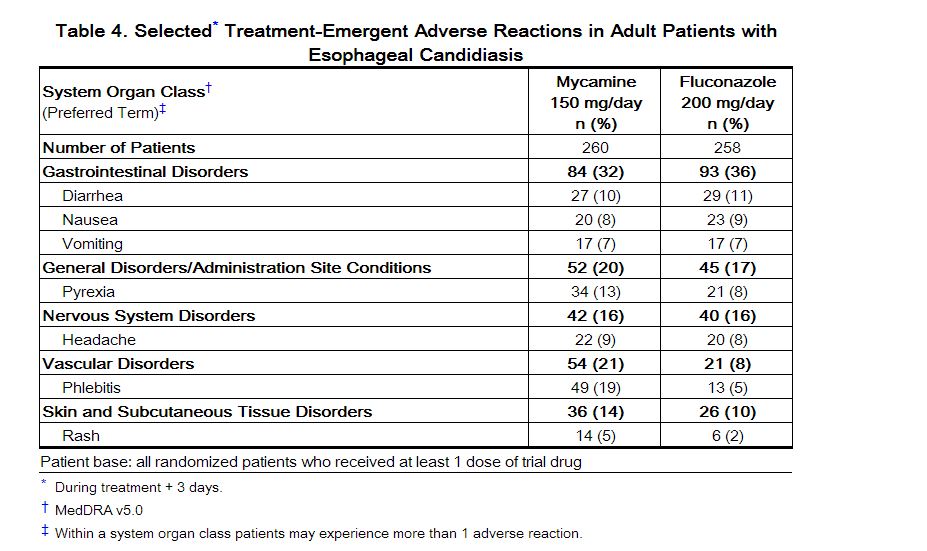 |
Prophylaxis of Candida Infections in Hematopoietic Stem Cell Transplant Recipients
A double-blind study was conducted in a total of 882 patients scheduled to undergo an autologous or allogeneic hematopoietic stem cell transplant. The median duration of treatment was 18 days (range 1 to 51 days) in both treatment arms.
All adult patients who received Mycamine (382) or fluconazole (409) experienced at least one adverse reaction during the study. Treatment-emergent adverse reactions resulting in Mycamine discontinuation were reported in 15 (4%) adult patients; while those resulting in fluconazole discontinuation were reported in 32 (8%). Selected adverse reactions, those reported in 15% or more of adult patients and more frequently on the Mycamine treatment arm, are shown in Table 5.
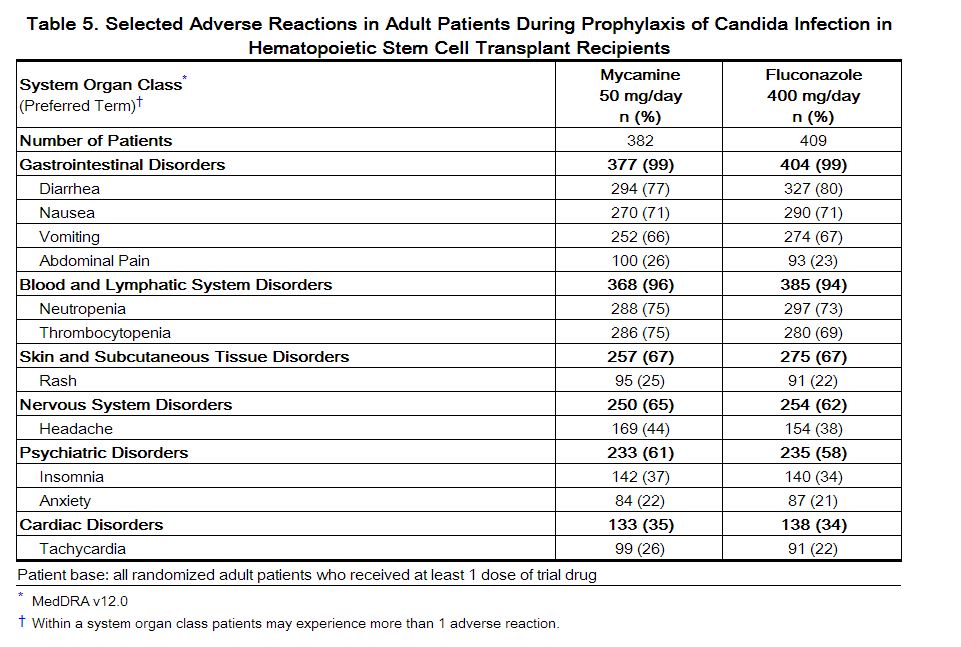 |
Other selected adverse reactions reported at less than 5% in adult clinical trials are listed below:
• Blood and lymphatic system disorders: coagulopathy, pancytopenia, thrombotic thrombocytopenic purpura • Cardiac disorders: cardiac arrest, myocardial infarction, pericardial effusion • General disorders and administration site conditions: infusion reaction, injection site thrombosis • Hepatobiliary disorders: hepatocellular damage, hepatomegaly, jaundice, hepatic failure • Immune disorders: hypersensitivity, anaphylactic reaction • Nervous system disorders: convulsions, encephalopathy, intracranial hemorrhage • Psychiatric disorders: delirium • Skin and subcutaneous tissue disorders: urticaria
Clinical Trials Experience in Pediatric Patients
The overall safety of Mycamine was assessed in 479 patients 3 days through 16 years of age who received at least one dose of Mycamine in 11 separate clinical studies. The mean treatment duration was 24.8 days. A total of 246 patients received at least one dose of Mycamine 2 mg/kg or higher.
Of the 479 pediatric patients, 264 (55%) were male, 319 (67%) were Caucasians, with the following age distribution: 116 (24%) less than 2 years, 108 (23%) between 2 and 5 years, 140 (29%) between 6 years and 11 years, and 115 (24%) between 12 and 16 years of age.
In all pediatric studies with Mycamine, 439/479 (92%) patients experienced at least one treatment-emergent adverse reaction.
Two studies that included pediatric patients were randomized, double-blind, and active-controlled: The invasive candidiasis and candidemia study investigated the efficacy and safety of Mycamine (2 mg/kg/day for patients weighing 40 kg or less and 100 mg/day for patients weighing greater than 40 kg) compared to AmBisome (3 mg/kg/day) in 112 pediatric patients. Treatment-emergent adverse reactions occurred in 51/56 (91%) of patients in the Mycamine group and 52/56 (93%) of patients in the AmBisome group. Treatment-emergent adverse reactions resulting in Mycamine discontinuation were reported in 2 (4%) pediatric patients; while those resulting in AmBisome discontinuation were reported in 9 (16%).
The prophylaxis study in patients undergoing HSCT investigated the efficacy of Mycamine (1 mg/kg/day for patients weighing 50 kg or less and 50 mg/day for patients weighing greater than 50 kg) as compared to fluconazole (8 mg/kg/day for patients weighing 50 kg or less and 400 mg/day for patients weighing greater than 50 kg). All 91 pediatric patients experienced at least one treatment-emergent adverse reaction. Three (7%) pediatric patients discontinued Mycamine due to adverse reaction; while one (2%) patient discontinued fluconazole.
The selected treatment-emergent adverse reactions, those occurring in 15% or more of the patients and more frequently in a Mycamine group, for all Mycamine pediatric studies and for the two comparative studies (candidemia and prophylaxis) described above are shown in Table 6.
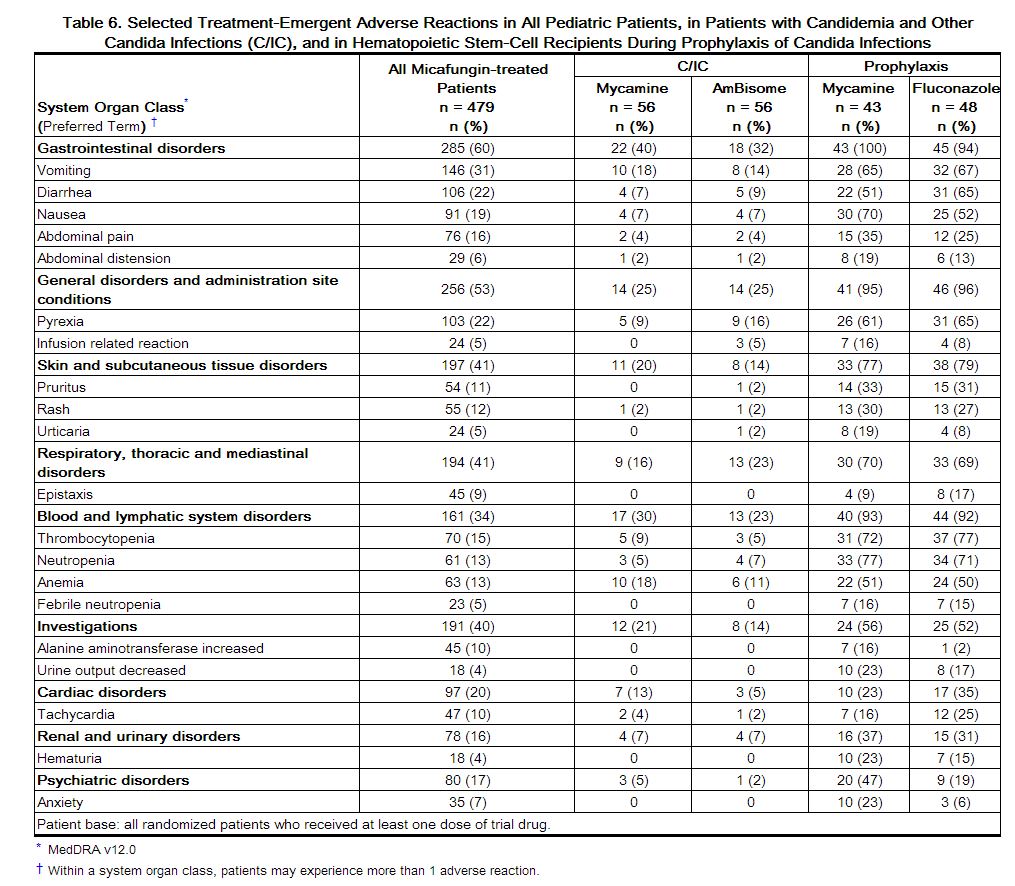 |
Other clinically significant adverse reactions reported at less than 15% in pediatric clinical trials are listed below:
• Hepatobiliary disorders: hyperbilirubinemia
• Investigations: liver function tests abnormal
• Renal Disorders: renal failure
Postmarketing Adverse Reactions
The following adverse reactions have been identified during the post-approval use of micafungin sodium for injection. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency.
• Blood and lymphatic system disorders: disseminated intravascular coagulation
• Hepatobiliary disorders: hepatic disorder
• Renal and urinary disorders: renal impairment
• Skin and subcutaneous tissue disorders: Stevens-Johnson syndrome, toxic epidermal necrolysis
• Vascular disorders: shock
References
Adapted from the FDA Package Insert.