Levofloxacin adverse reactions
Template:Levofloxacin Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Abdurahman Khalil, M.D. [2]
ADVERSE REACTIONS
Serious and Otherwise Important Adverse Reactions
The following serious and otherwise important adverse drug reactions are discussed in greater detail in other sections of labeling:
- Tendon Effects
- Hypersensitivity Reactions
- Other Serious and Sometimes Fatal Reactions
- Hepatotoxicity
- Central Nervous System Effects
- Clostridium difficile-Associated Diarrhea
- Peripheral Neuropathy
- Prolongation of the QT Interval
- Musculoskeletal Disorders in Pediatric Patients
- Blood Glucose Disturbances
- Photosensitivity/Phototoxicity
- Development of Drug Resistant Bacteria
Hypotension has been associated with rapid or bolus intravenous infusion of LEVAQUIN®. LEVAQUIN® should be infused slowly over 60 to 90 minutes, depending on dosage [see Dosage and Administration (2.5)].
Crystalluria and cylindruria have been reported with quinolones, including LEVAQUIN®. Therefore, adequate hydration of patients receiving LEVAQUIN®should be maintained to prevent the formation of a highly concentrated urine [see Dosage and Administration (2.5)].
Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data described below reflect exposure to LEVAQUIN® in 7537 patients in 29 pooled Phase 3 clinical trials. The population studied had a mean age of 50 years (approximately 74% of the population was < 65 years of age), 50% were male, 71% were Caucasian, 19% were Black. Patients were treated with LEVAQUIN® for a wide variety of infectious diseases [see Indications and Usage (1)]. Patients received LEVAQUIN® doses of 750 mg once daily, 250 mg once daily, or 500 mg once or twice daily. Treatment duration was usually 3–14 days, and the mean number of days on therapy was 10 days.
The overall incidence, type and distribution of adverse reactions was similar in patients receiving LEVAQUIN® doses of 750 mg once daily, 250 mg once daily, and 500 mg once or twice daily. Discontinuation of LEVAQUIN® due to adverse drug reactions occurred in 4.3% of patients overall, 3.8% of patients treated with the 250 mg and 500 mg doses and 5.4% of patients treated with the 750 mg dose. The most common adverse drug reactions leading to discontinuation with the 250 and 500 mg doses were gastrointestinal (1.4%), primarily nausea (0.6%); vomiting (0.4%); dizziness (0.3%); and headache (0.2%). The most common adverse drug reactions leading to discontinuation with the 750 mg dose were gastrointestinal (1.2%), primarily nausea (0.6%), vomiting (0.5%); dizziness (0.3%); and headache (0.3%).
Adverse reactions occurring in ≥1% of LEVAQUIN®-treated patients and less common adverse reactions, occurring in 0.1 to <1% of LEVAQUIN®-treated patients, are shown in Table 6 and Table 7, respectively. The most common adverse drug reactions (≥3%) are nausea, headache, diarrhea, insomnia, constipation, and dizziness.
In clinical trials using multiple-dose therapy, ophthalmologic abnormalities, including cataracts and multiple punctate lenticular opacities, have been noted in patients undergoing treatment with quinolones, including LEVAQUIN®. The relationship of the drugs to these events is not presently established.
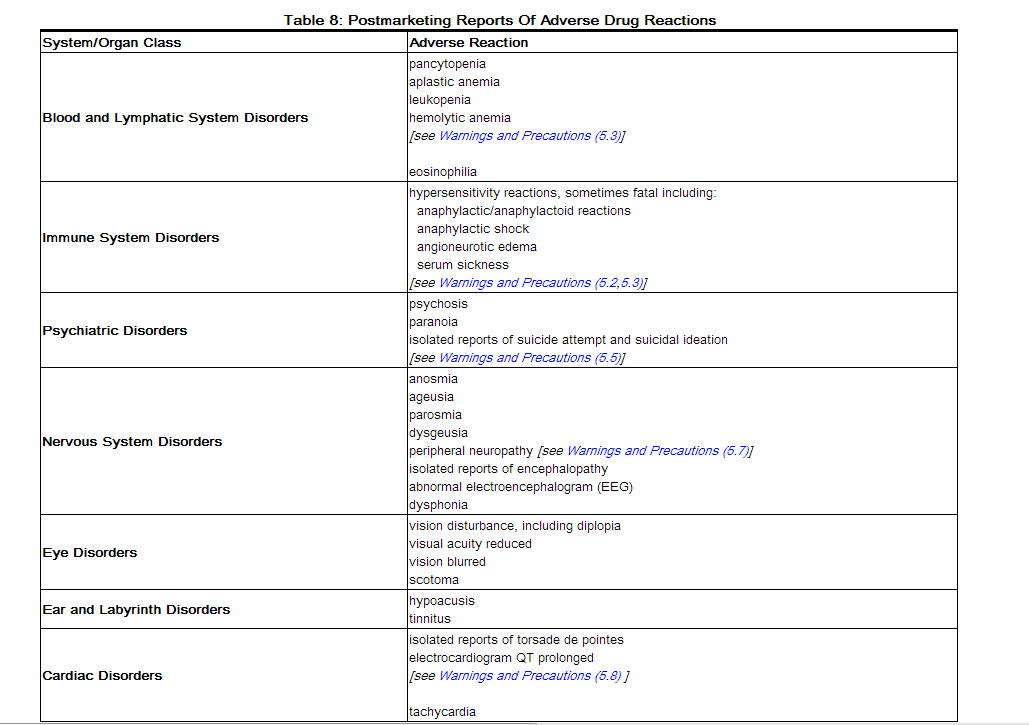
Postmarketing Experience
Table 8 lists adverse reactions that have been identified during post-approval use of LEVAQUIN®. Because these reactions are reported voluntarily from a population of uncertain size, reliably estimating their frequency or establishing a causal relationship to drug exposure is not always possible.