Intracoronary stenting
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Bifurcation Lesions
1. Kissing Stent Technique
Benefits
- Ensures complete coverage of the side branch ostium
- Immediate patency of parent and side branch
- Access to both branches maintained through procedure
- No need for final kissing balloon
Detriments
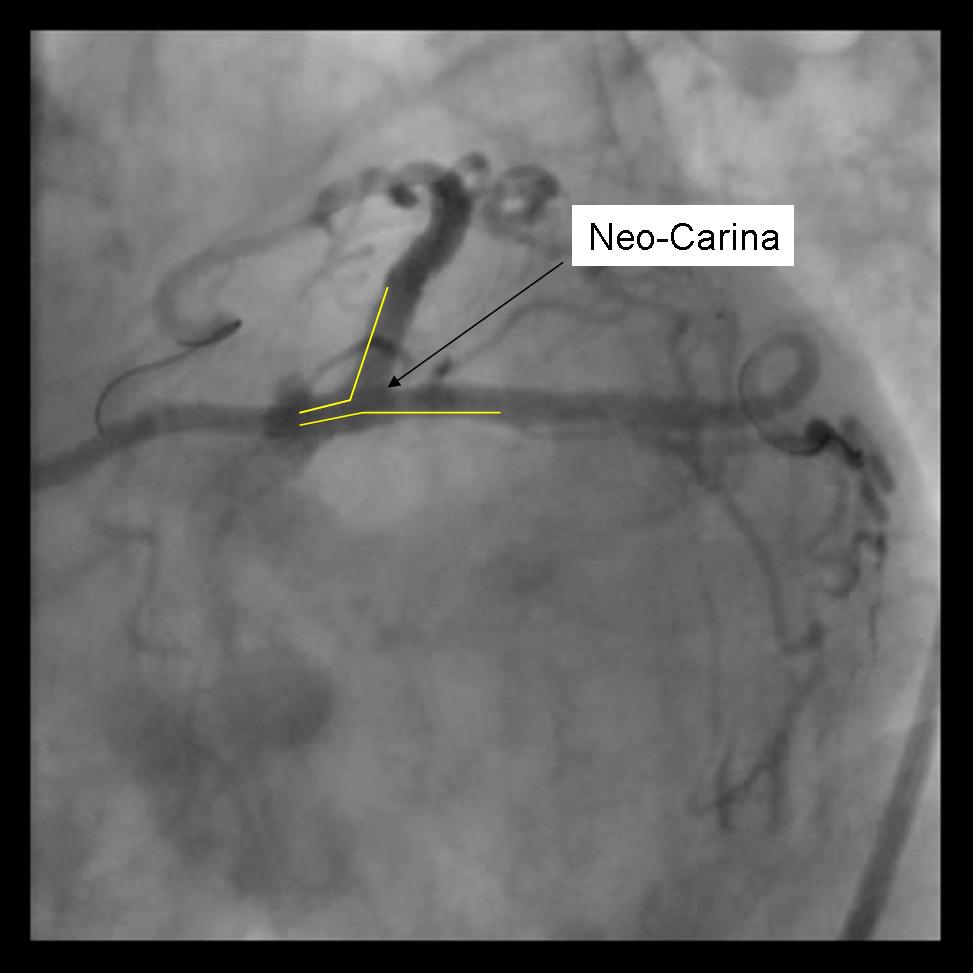
- Un-endothelialized layer of stents forming neo-carina may predispose to stent thrombosis.
- 8Fr Guide system required
- May be difficult to re-access side branch or parent vessel
Technical Considerations
- Requires minimum of a 8Fr Guiding system
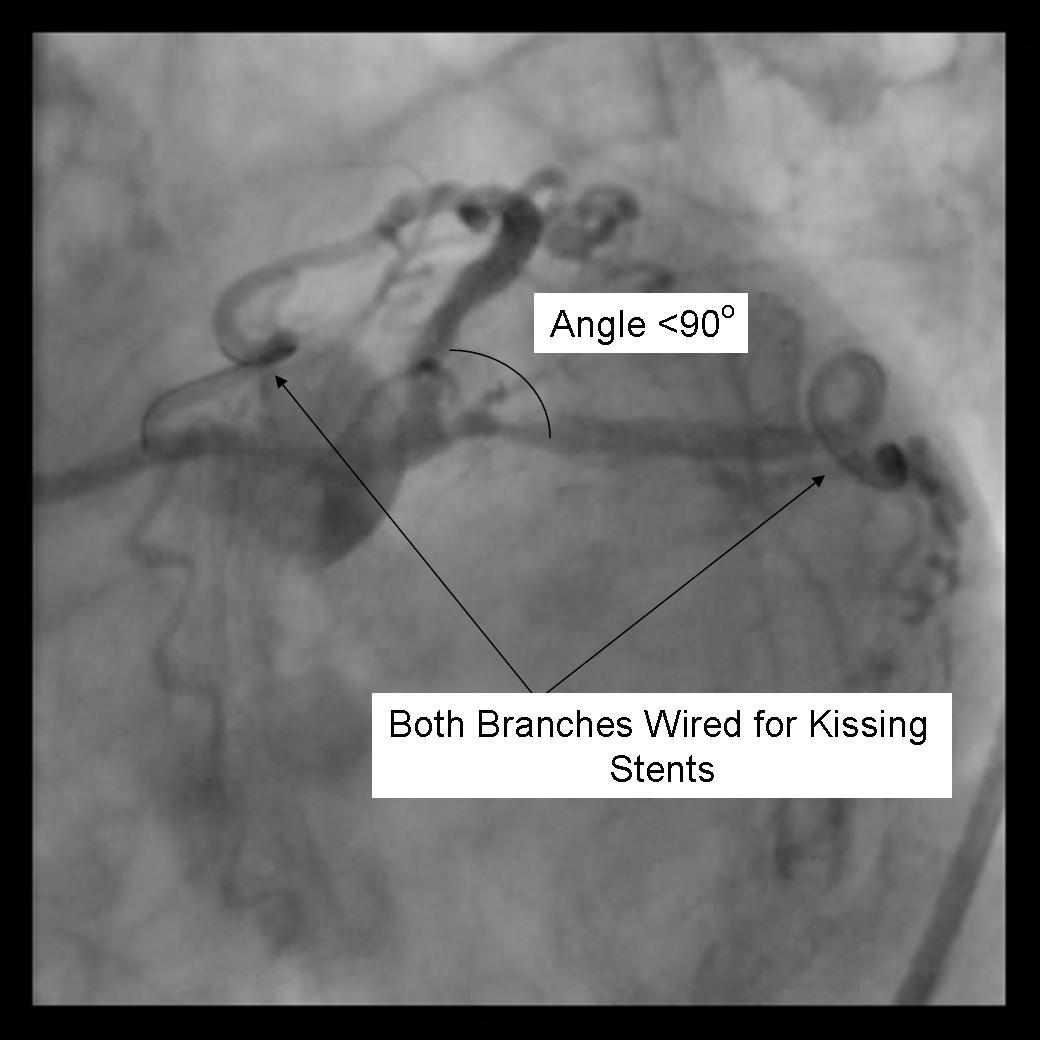
- Optimal angle of bifurcation less than 90 degrees.
Technique
1) Using a minimum 8Fr guide system, both the parent and side branch are wired. Predilation is recommended to ensure optimal balloon expansion and ease stent delivery. It is important to identify which wire is placed in which branch. We recommend either using 2 separate colored guide wires, keeping a marker on 1 wire, or covering a wire with a sterile towel while not in use.
 |
<googlevideo>1873623062002840911&hl=en</googlevideo> |
2) Any disease distal to the side branch or parent vessel should optimally be repaired before the kissing stents are deployed.
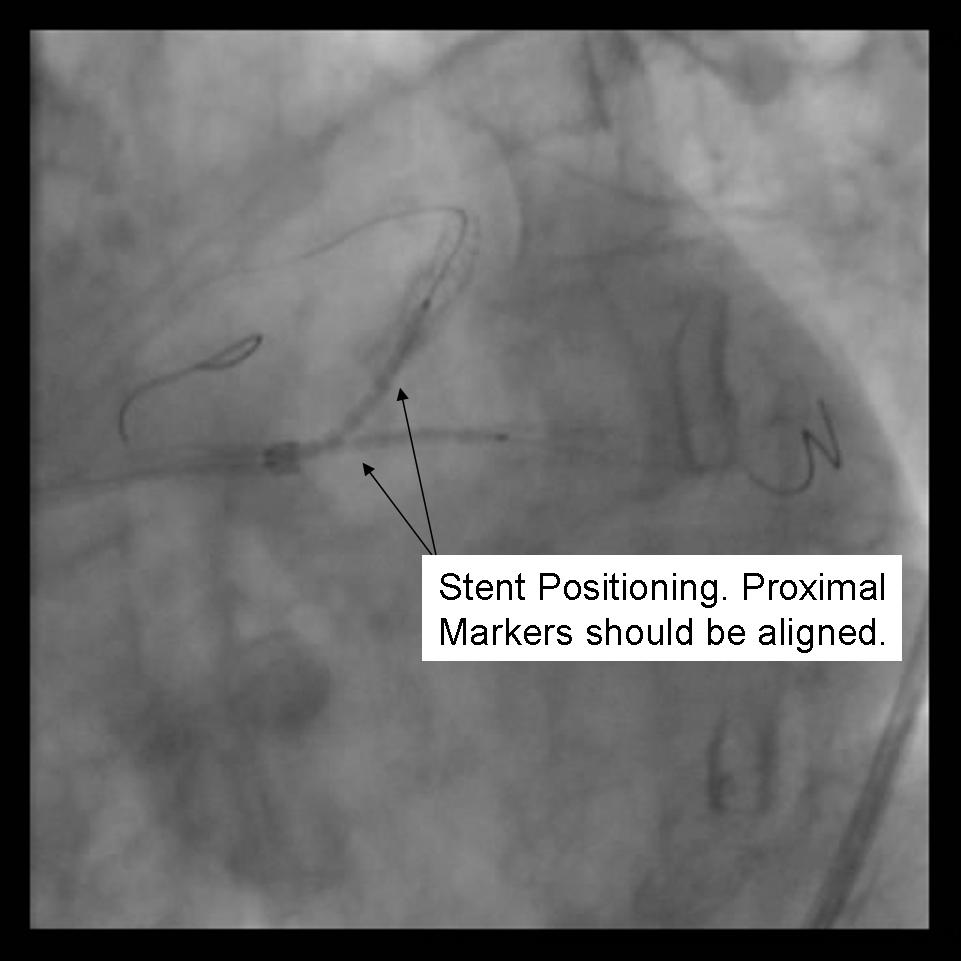
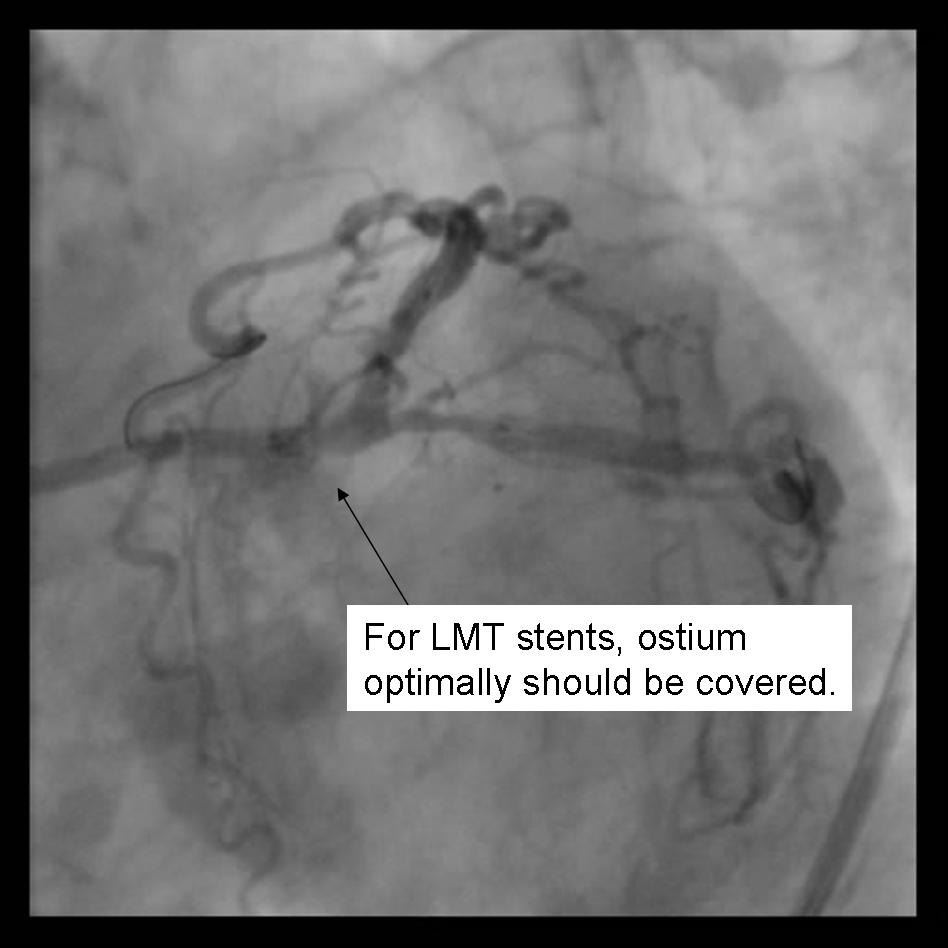
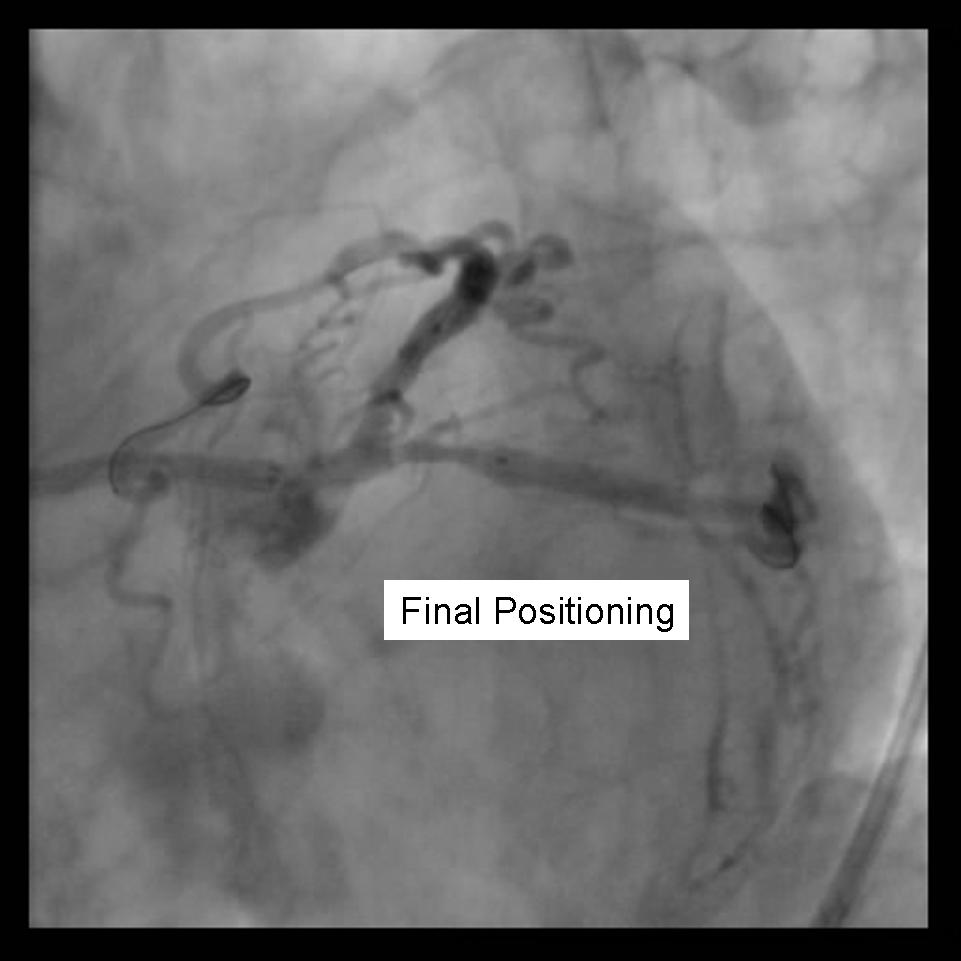
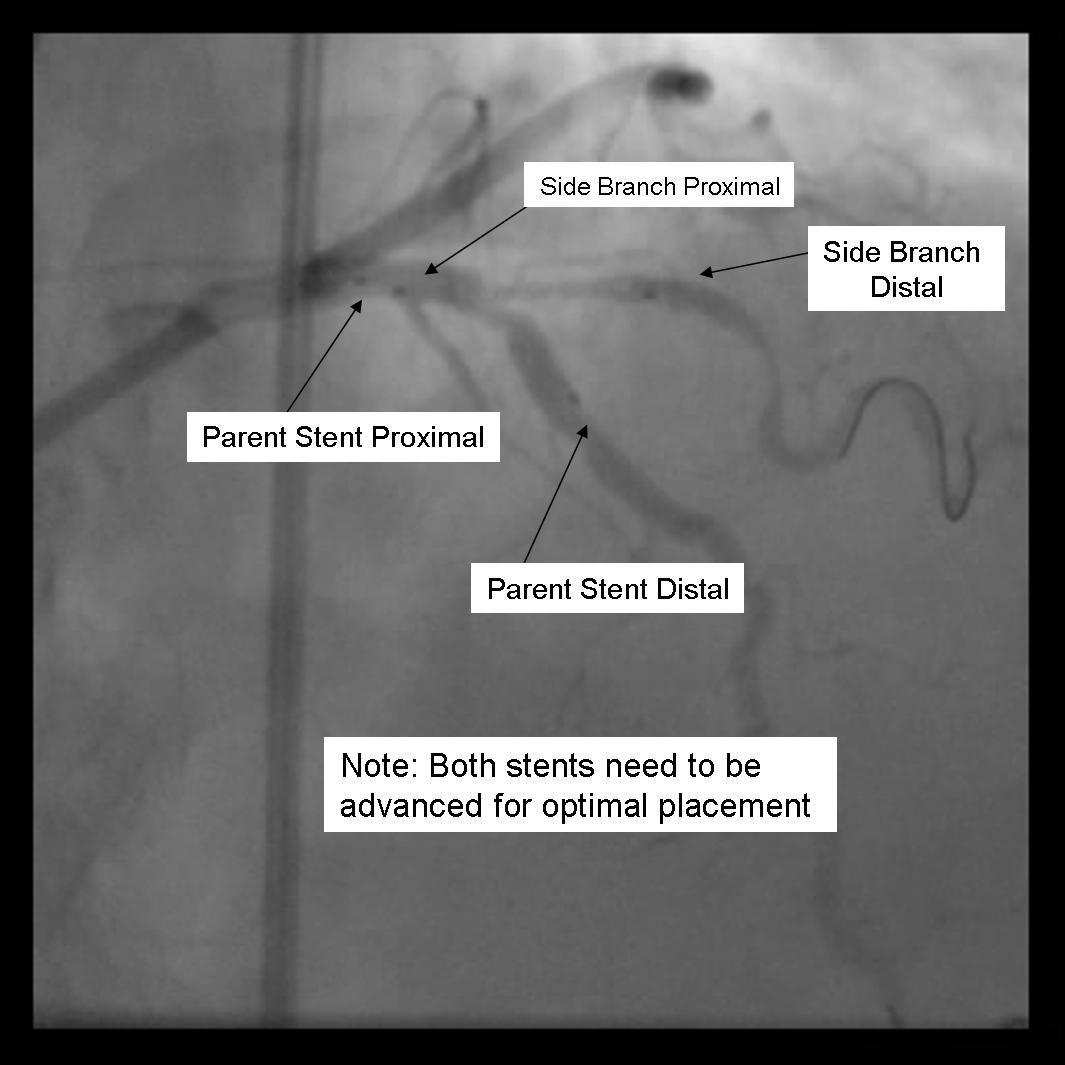
3) Both stents are advanced into the side branch and parent vessel. This may require further predilitation. Generally, the stents are advanced beyond the delivery point. Operator preference differs with respect to amount of overlap. Some operators form a long segment of overlap (>5mm), while others try to minimize overlap. It is absolutely essential that both vessels are covered during the balloon inflation. Optimal placement is ensured by advancing both stents distal to the intended deployment site then pulling them back into position. The proximal marker segements should be aligned, with positional confirmation in at least 2 separate views.
 |
<googlevideo>-2198706559365896519&hl=en</googlevideo> |
 |
<googlevideo>6739334144213459915&hl=en</googlevideo> |
4) Using 2 Insufflators, both stents are inflated to low pressure. Then alternating with side branch and parent branch inflated to optimal deployment size. There is some risk of over sizing the main branch with the overlapping stent segments. In the case where proximal disease may interfere with the 2 overlapping stents, a proximal stent may be deployed prior to inflating the 2 distal stents. (Pants-and-trousers technique)
 |
<googlevideo>6739334144213459915&hl=en</googlevideo> |
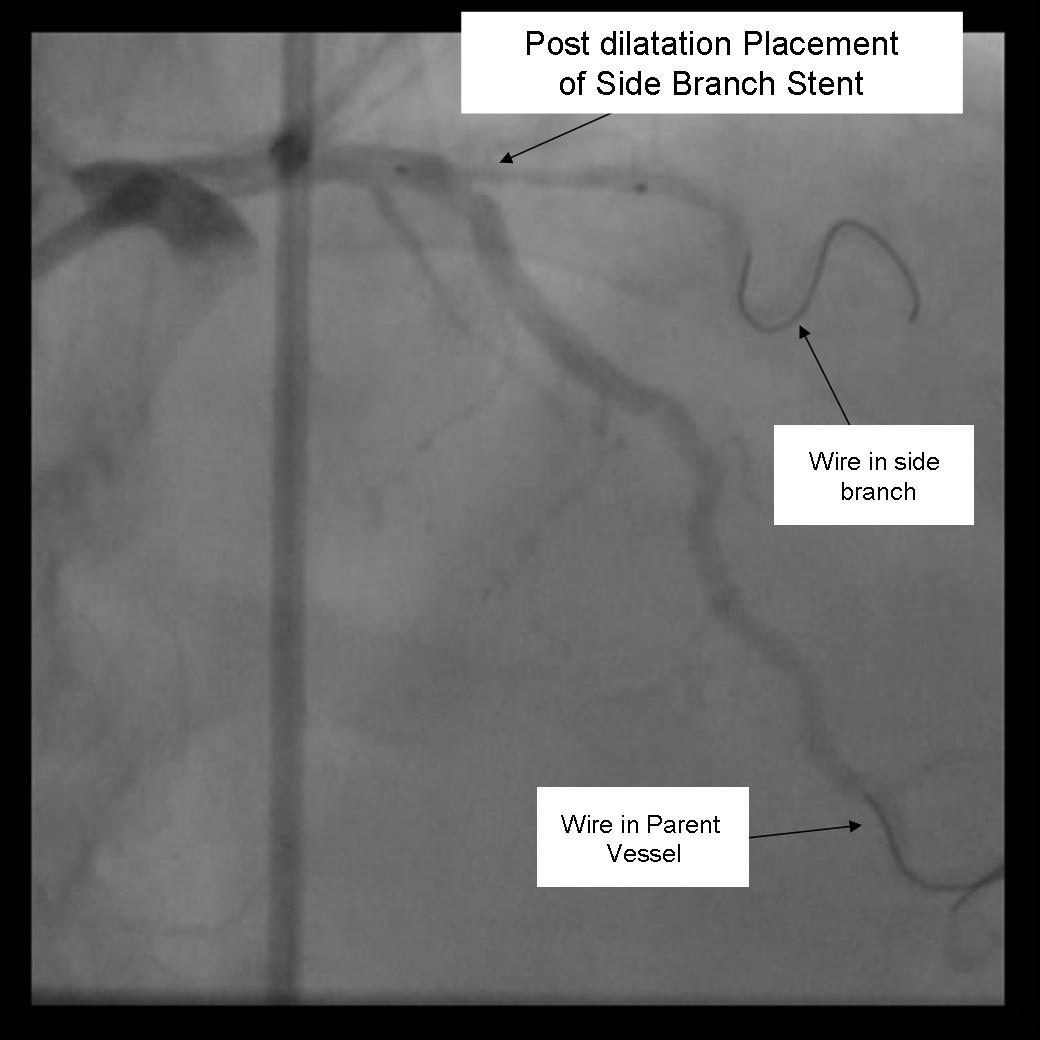
5) Angiography should now be performed to ensure adequate side branch coverage and stent deployment. Distal edge dissections or disease should be addressed before wire removal from the vessels.
 |
<googlevideo>-1540905286545689451&hl=en</googlevideo> |
Variations of this method may be used to stent trifurcation disease. While an 8Fr catheter can be used depending on the stent system, optimally a 9 Fr system should be used in this situation.
2. The Crush Technique
Benefits
Ensures complete coverage of the side branch ostium Immediate patency of parent and side branch Excellent immediate angiographic results Restenosis is usually very focal
Detriments
3 Layers of stent in the main artery Without final kissing balloon inflation high Restenosis rate May be difficult to re-cross side branch Minimal 7Fr guide system required
Technical Considerations
Requires minimum of a 7Fr Guiding system Final Kissing balloon inflation required due to high Restenosis rate
Technique
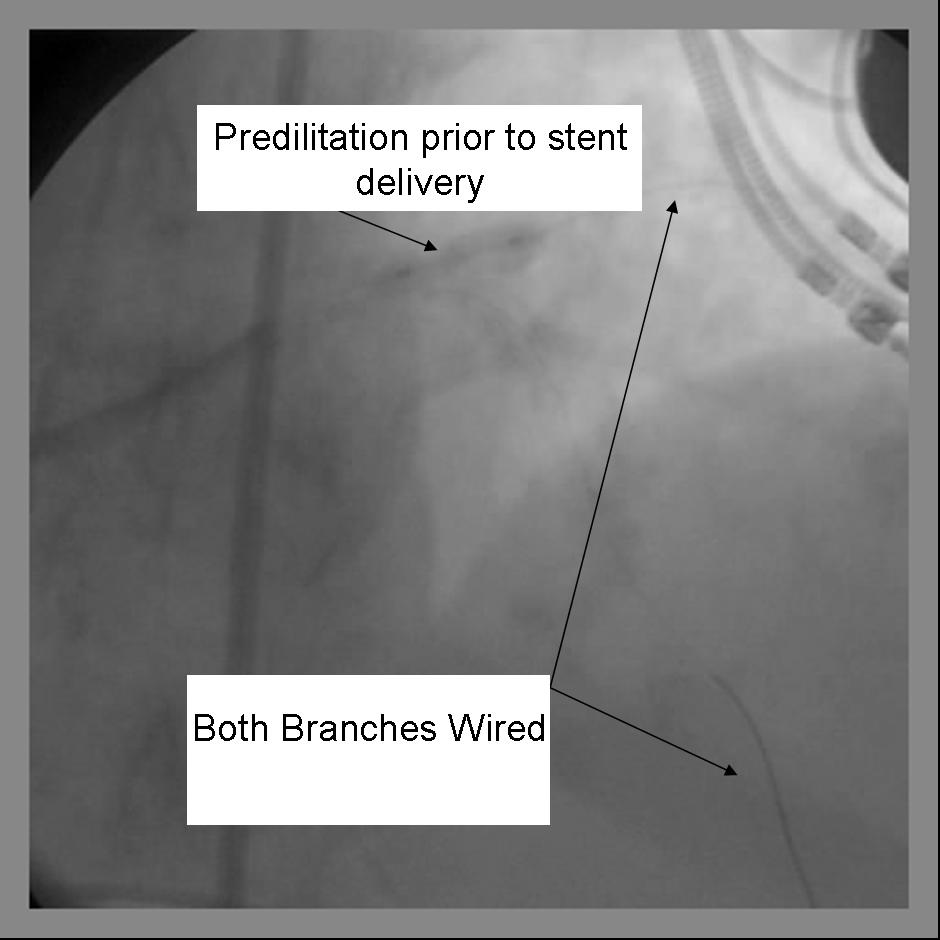
1) Using a minimum 7Fr guide system, both the parent and side branch are wired. Predilation is recommended to ensure optimal balloon expansion and ease stent delivery. It is important to identify which wire is placed in which branch. We recommend either using 2 separate colored guide wires, keeping a marker on 1 wire, or covering a wire with a sterile towel while not in use.
2) Any disease distal to the side branch should optimally be repaired before the final crush step.
3) The 1st stent is advanced into the side branch. This may require further predilitation. Generally, the stent is advanced beyond the delivery point.
 |
<googlevideo>-6644364110521967374&hl=en</googlevideo> |
4) The 2nd stent is advanced into the parent vessel. This is also placed beyond the intended deployment site.
5) The side branch stent is pulled back into the parent vessel about 5 mm. This ensures adequate coverage of the ostium.
6) The parent stent is pulled back crossing the side branch and the proximal end is placed proximal to the proximal end of the side branch stent.
 |
<googlevideo>-2384934812388551194&hl=en</googlevideo> |
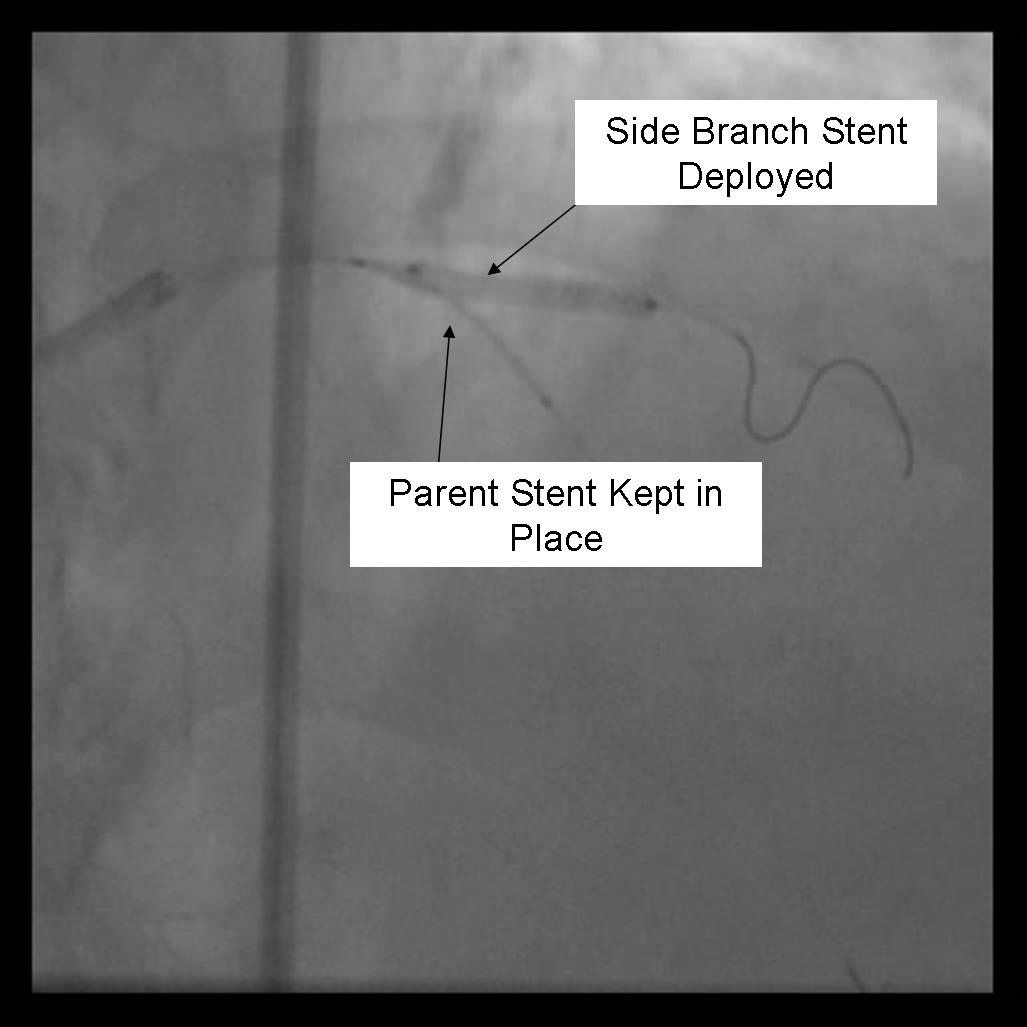
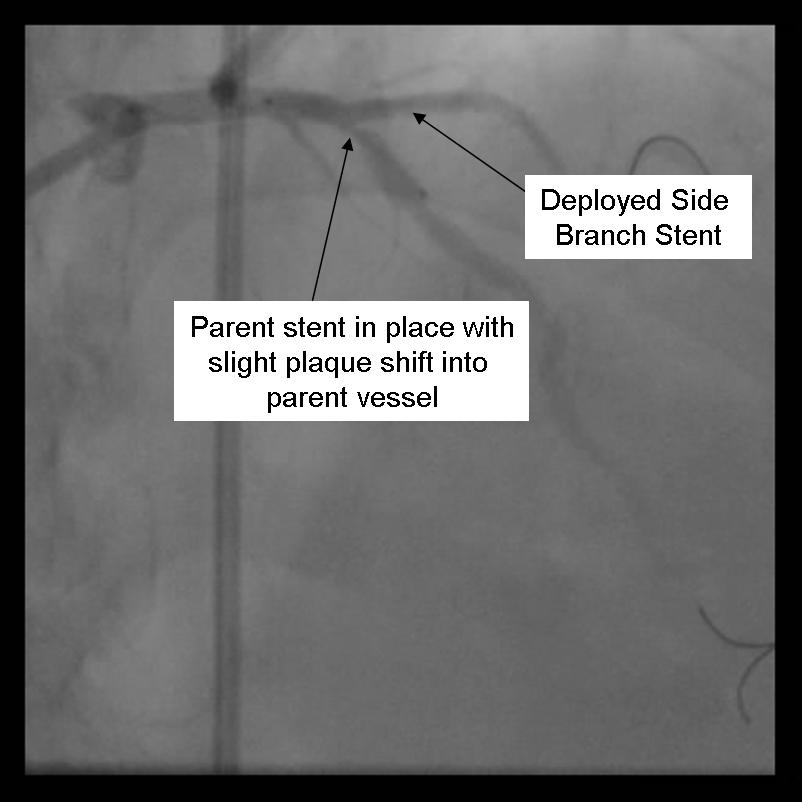
7) The side branch stent is deployed.
 |
<googlevideo>-2225481000332319520&hl=en</googlevideo> |
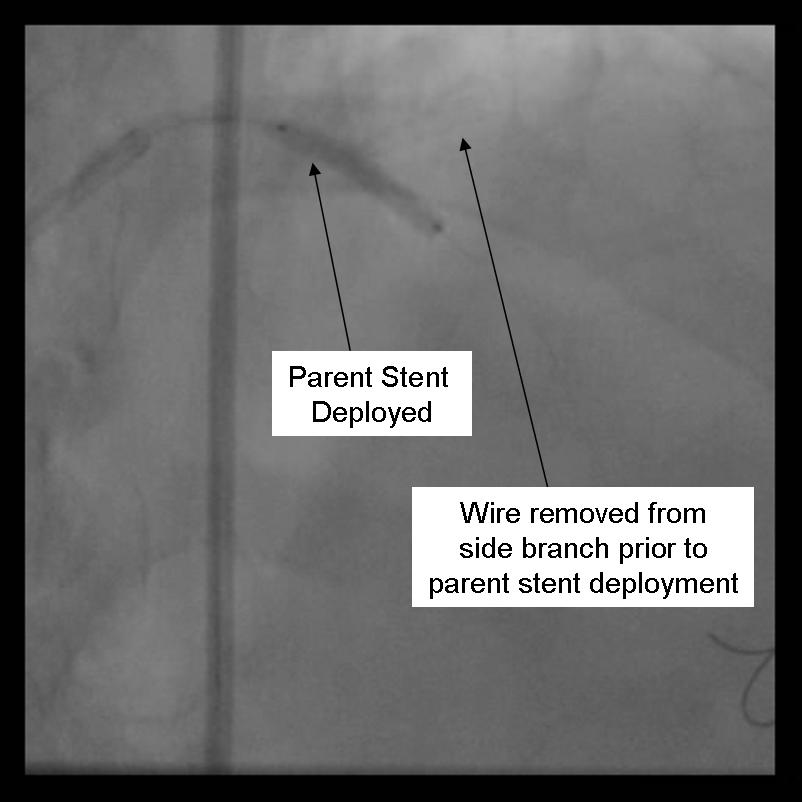
8) Angiography should now be performed to ensure adequate side branch coverage and stent deployment. Distal edge dissections or disease should be addressed before parent stent deployment. Once complete, the side branch wire is removed.
 |
<googlevideo>6608019255966212549&hl=en</googlevideo> |
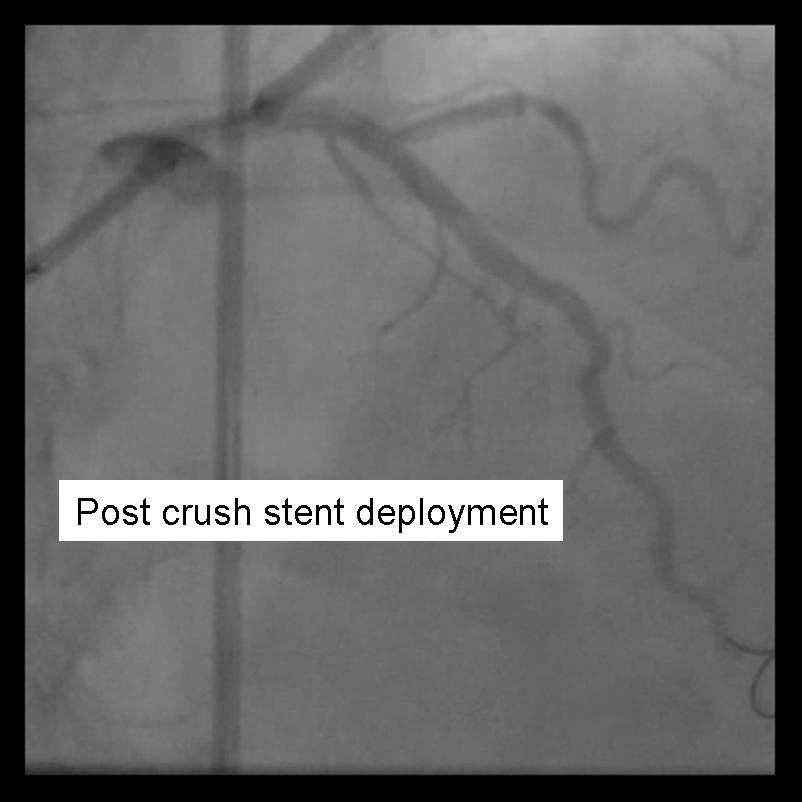
9) The parent stent is deployed.
 |
<googlevideo>5013022603317484197&hl=en</googlevideo> |
 |
<googlevideo>2049938197341162787&hl=en</googlevideo> |
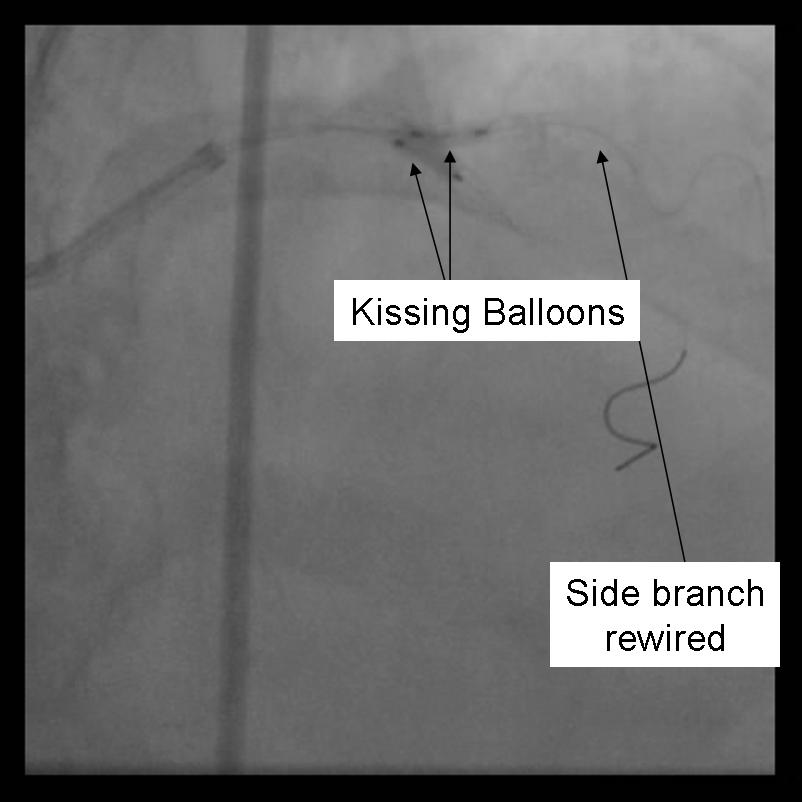
10) The side-branch is rewired. It is sometimes necessary to change wires to either a hydrophilic wire eg. Whisper, (Guidant, Temecula, California) or Pilot 50 or 150 (Guidant, Temecula, California), or ASAHI Fielder (Abbott Vascular Devices, Redwood City, California), one of increasing stiffness eg. ASAHI Miracle Bros 3 (Abbott Vascular Devices, Redwood City, California), or both eg. Shinobi (Guidant, Temecula, California) or Confienza(Abbott Vascular Devices, Redwood City, California).
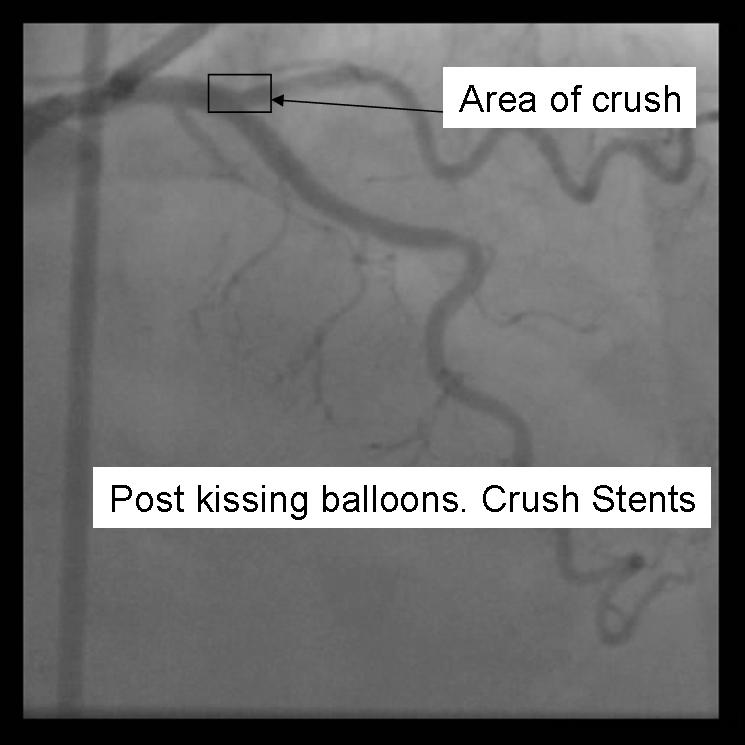
11) Kissing balloons are inflated at the bifurcation. It is sometimes necessary to dilate the sidebranch with a small balloon (1.5 mm middle marker balloon) to facilitate a larger balloon for the kiss.
 |
<googlevideo>-3998349476747507559&hl=en</googlevideo> |
12) Repeat angiography is performed. Wires are removed and final angiography completed.
 |
<googlevideo>9148159160696936306&hl=en</googlevideo> |
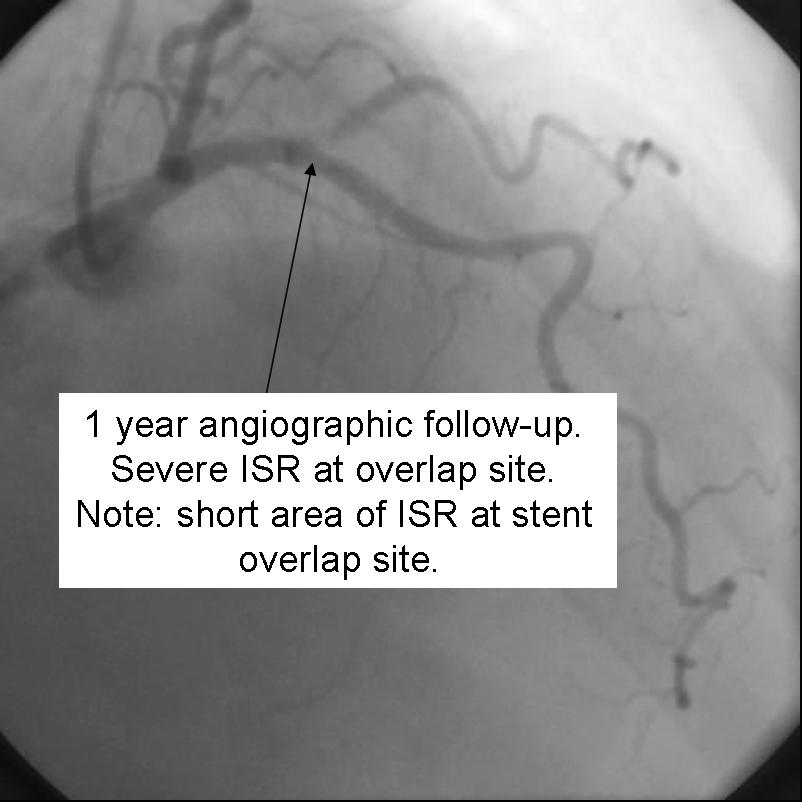
Despite excellent initial angiographic results, side branch restenosis is still a significant problem with Crush stenting(Up to 25% without kissing ballon inflation). However,most of the restenosis is silent. The above example used Cypher drug eluting stents in the Side branch and Parent vessels. The patient returned with positive stress testing 13 months later. Repeat angiography demonstrated a short segment of significant in-stent restenosis.
 |
<googlevideo>-676433419690470542&hl=en</googlevideo> |
3. T-Stenting
Benefits
- May be used for provisional stenting of side branch if angiographic result is poor.
- Can Use 6Fr guide system
- Restenosis is usually very focal
Detriments
- Very difficult, if not impossible to completely cover side branch ostium
- Requires final kissing balloon inflation
- Modified T-stent technique requires 7Fr guide system
Technical Considerations
- May use a 6Fr Guiding system
- Final Kissing balloon inflation required due to high Restenosis rate
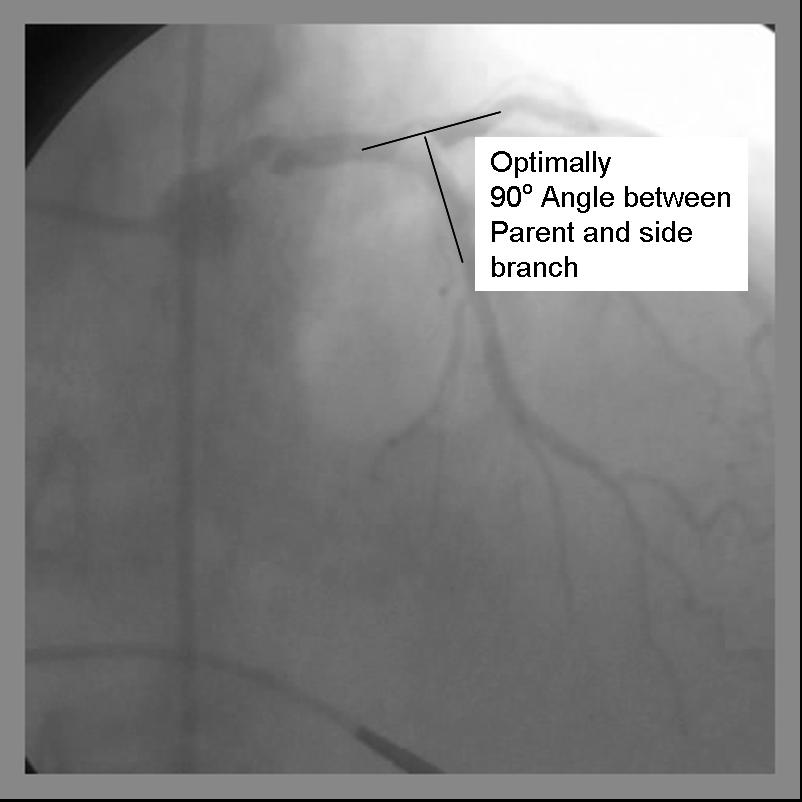
- Ideal angle of bifurcation is at or near 90 degrees.
 |
<googlevideo>7259214304163348609&hl=en</googlevideo> |
Technique (Modified T-Stenting)
1) A 6Fr guide system may be used with standard T-stenting in which the side branch stent is deployed, followed by delivery and deployment of the parent stent. The modified technique, which is preferred by this operator, requires a minimum of 7Fr guide system.
2) Both the parent and side branch are wired. Predilation is recommended to ensure optimal balloon expansion and ease stent delivery. It is important to identify which wire is placed in which branch. We recommend either using 2 separate colored guide wires, keeping a marker on 1 wire, or covering a wire with a sterile towel while not in use.
 |
<googlevideo>-8290939644314628088&hl=en</googlevideo> |
3) Any disease in the distal side branch or parent vessel should optimally be repaired before the bifurcation stents are deployed.
4) The 1st stent is advanced into the side branch. This may require further predilitation. Generally, the stent is advanced beyond the delivery point.
5) The 2nd stent is advanced into the parent vessel and placed across the side branch.
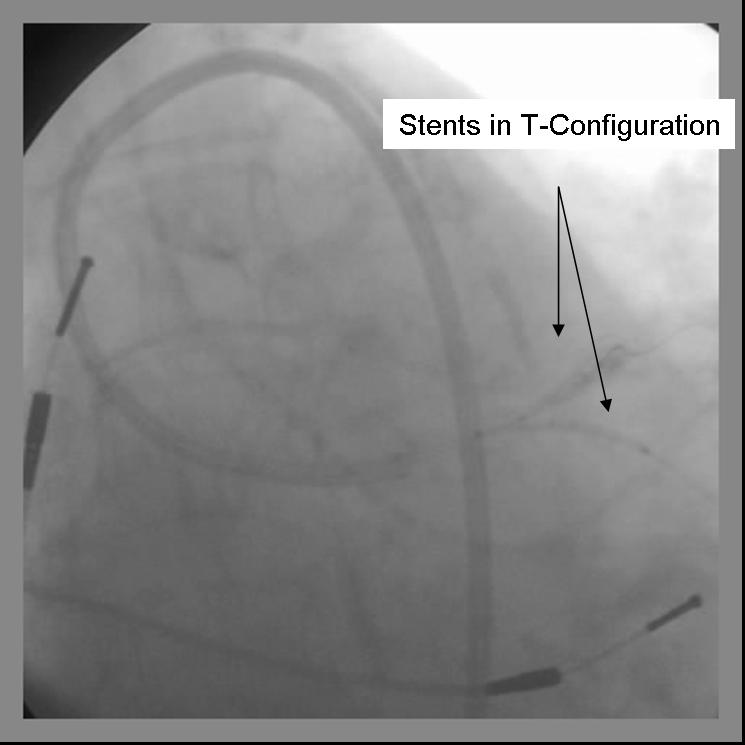 |
<googlevideo>-8176401098564532983&hl=en</googlevideo> |
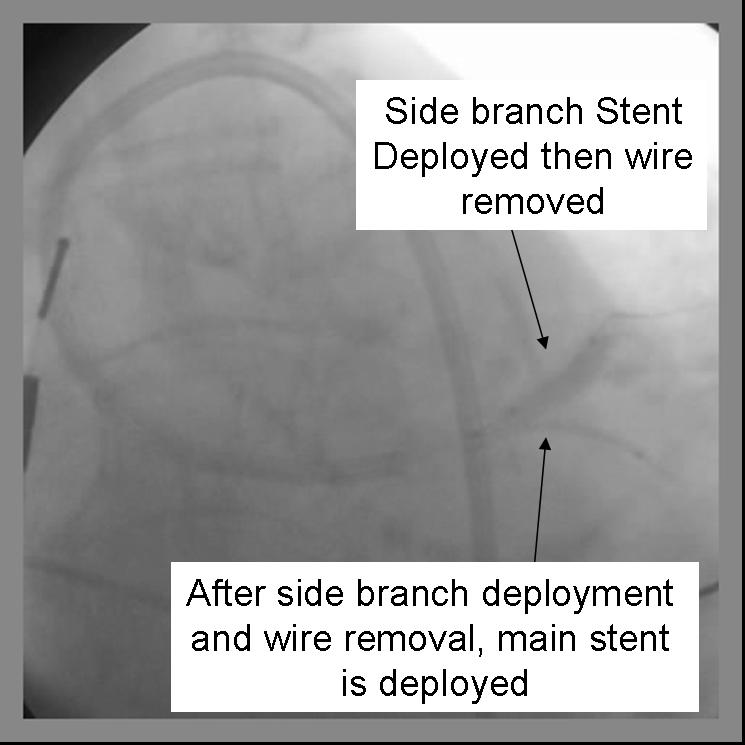
6) The side branch stent is deployed. (Another option is to place a balloon in the parent branch and inflating to low atm while pulling the side branch back. This may help ensure adequate coverage of the ostium.
7) Side branch wire is removed once adequate angiographic result confirmed.
8) The parent stent is deployed across the side branch.
 |
<googlevideo>4485530437540579771&hl=en</googlevideo> |
9) Angiography should now be performed to ensure adequate side branch coverage and stent deployment. The parent stent is deployed.
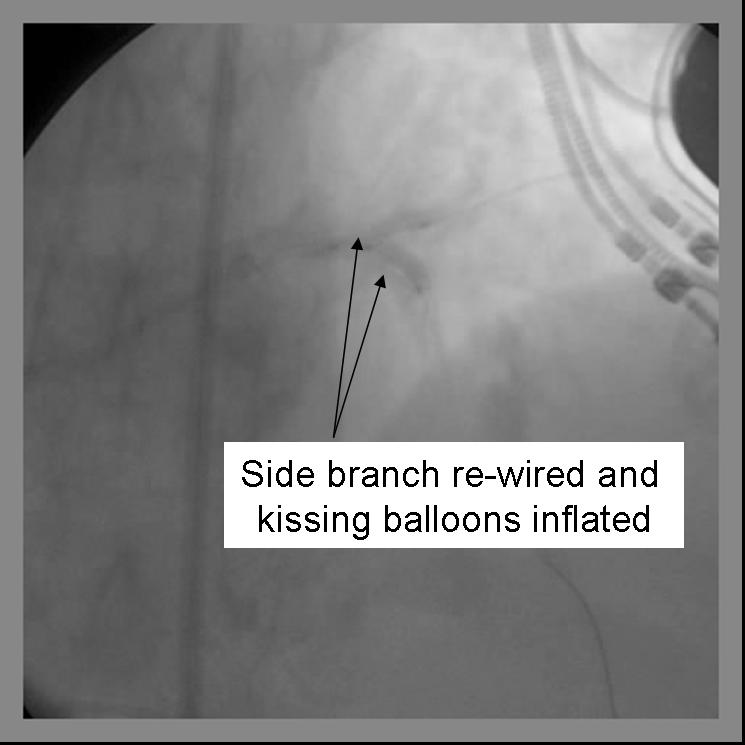
10) The side-branch is rewired. It is sometimes necessary to change wires to either a hydrophilic wire eg. Whisper, (Guidant, Temecula, California) or Pilot 50 or 150 (Guidant, Temecula, California), or Fielder (Abbott Vascular Devices, Redwood City, California), one of increasing stiffness eg. ASAHI Miracle Bros 3 (Abbott Vascular Devices, Redwood City, California), or both eg. Shinobi (Guidant, Temecula, California) or Confienza (Abbott Vascular Devices, Redwood City, California).
11) Kissing balloons are inflated at the bifurcation. It is sometimes necessary to dilate the sidebranch with a small balloon (1.5 mm middle marker balloon) to facilitate a larger balloon for the kiss.
 |
<googlevideo>4382003640399583914&hl=en</googlevideo> |
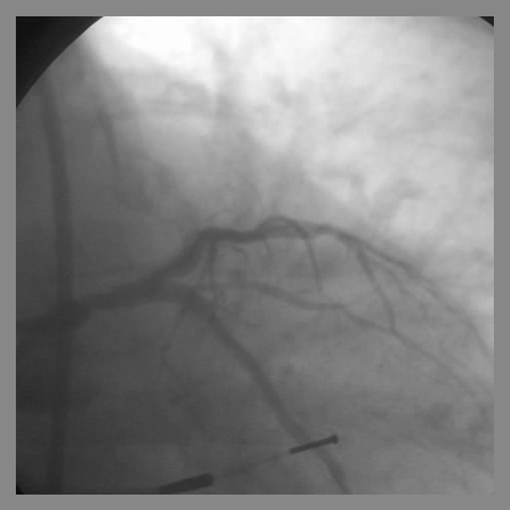
12) Repeat angiography is performed. Wires are removed and final angiography completed.
 |
<googlevideo>-2232340403491043434&hl=en</googlevideo> |
- Provisional T-Stenting involves the stenting the parent vessel and only the side branch if there is less than adequate side branch angiographic result. In this situation, the side branch may need to be serially dilated with up to a 2.5 mm balloon to ensure stent delivery. Final kissing balloons should be repeated.
- Sometimes the side branch stent impinges on the parent lumen making delivery of the parent stent impossible. If this happens, dilation of the parent lumen with a balloon allows for stent delivery. This may create a partial or small area of crushed stent at the bifurcation and should be followed with kissing balloons.
How to Evaluate the post-stent-deployment angiogram?
Following coronary stent implantation, the following set of steps is one way to systematically evaluate the post-stent-deployment angiogram.
- Is there any injury to the proximal vessel from guide catheter manipulation?
- Is the stent well expanded throughout its length, or are there residual stenoses?
- Does the stented segment of the vessel appear hazy?
- Did the stent deployment compromise blood flow in any branch vessels?
- Are there any tears in the vessel such as proximal or distal edge dissection, or dye extravasation to the vessel wall or the pericardium?
- How is the flow in the coronary artery and the myocardium that it supplies?
- Is there any distal microvasculature perforation secondary to the guide wire manipulation?
In addition to the angiographic interpretation, clinical assessment is very important. Chest discomfort, arrhythmia, ischemic ECG changes, and hypotension may all result following stent deployment.
Restenosis
Restenosis is a process of neointimal hyperplasia following PCI.
Incidence of angiographic restenosis at 6 months following balloon angioplasty (without stenting) is about 40%. Up to 75% of these cases (~30% of total cases) present as clinical restenosis. Restenosis which develops after the first year is uncommon. The best treatment for restenosis following balloon angioplasty is stent implantation whenever technically feasible.
Historically, incidence of angiographic and clinical restenosis at 1 year following bare metal stenting has been about 30% and 15%, respectively. A more contemporary study (2000 – 2002) of the Duke database demonstrated a clinical restenosis rate of 9.3%. Correlates of higher risk of in-stent restenosis include longer stent length, smaller stent diameter, diabetes mellitus and stent location at a bifurcation. The preferred therapy for restenosis of a bare metal stent is restenting with a drug-eluting stent.
Drug-eluting stents inhibit neointimal hyperplasia. Incidence of in-stent restenosis within a drug-eluting stent is about 10% angiographic and 6% clinical. The best percutaneous therapy for in-stent restenosis of a drug-eluting stent is probably restenting with yet another drug-eluting stent (perhaps one with a different coated medication). Bypass surgery can also be considered if the patient is a surgical candidate and a distal target is adequate.
With drug-eluting stents, it is important to maintain uninterrupted long-term dual antiplatelet therapy (with aspirin and clopidogrel) to prevent the occurrence of stent thrombosis, an event associated with a high rate of myocardial infarction and death.