Wolff-Parkinson-White syndrome pathophysiology
| https://https://www.youtube.com/watch?v=9MDRKId2d0Q%7C350}} |
|
Wolff-Parkinson-White syndrome Microchapters |
|
Differentiating Wolff-Parkinson-White syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Wolff-Parkinson-White syndrome pathophysiology On the Web |
|
Risk calculators and risk factors for Wolff-Parkinson-White syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
In normal individuals, electrical activity in the heart is initiated in the sinoatrial (SA) node (located in the right atrium), propagates to the atrioventricular (AV) node, and then through the bundle of His to the ventricles of the heart. Individuals with Wolf-parkinson-White (WPW) have an accessory pathway, known as the bundle of Kent, that communicates between the atria and the ventricles. The conduction through the accessory pathway can be bidirectional (most commonly), only retrogarde (less common), or only antegrade (least common). The most common type of tachycardia associated with WPW is atrioventricular reciprocating tachycardia (AVRT). The accessory pathway does not share the rate-slowing properties of the AV node; therefore, the combination of an accessory pathway and cardiac arrhythmia can trigger ventricular fibrillation, a leading cause of sudden cardiac death.
Pathophysiology
Accessory Pathway
Individuals with WPW have a congenital accessory pathway that communicates between the atria and the ventricles, in addition to the AV node. This accessory pathway is known as the bundle of Kent. The bundle of Kent is an abnormal extra or accessory conduction pathway between the atria and ventricles that is present in a small percentage (between 0.1% and 0.3%) of the general population.[1][2] This pathway may communicate between the left atrium and the left ventricle, in which case it is termed a "type A pre-excitation", or between the right atrium and the right ventricle, in which case it is termed a "type B pre-excitation".[3]
The accessory pathway:[4]
- Conducts electrical stimulus faster than the AV node
- Has a longer refractory period compared to the AV node
- Is most commonly characterized by a non-decremental conduction in response to an increased paced rates
Electrical Activity
Normal Electrical Activity
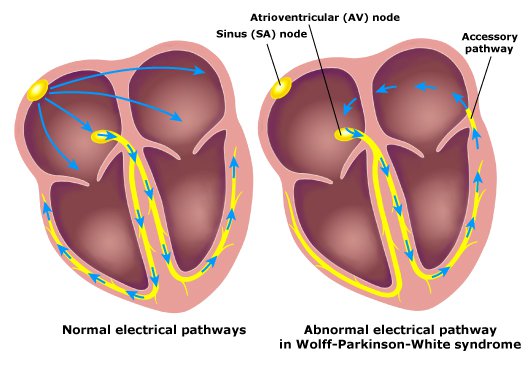
The electrical activity in the normal human heart is initiated when a cardiac action potential arises in the sinoatrial (SA) node, which is located in the right atrium. From there, the electrical stimulus is transmitted via internodal pathways to the atrioventricular (AV) node. After a brief delay at the AV node, the stimulus is conducted through the bundle of His to the left and right bundle branches and then to the Purkinje fibers and the endocardium at the apex of the heart, then finally to the ventricular myocardium.
Shown below is an image depicting the conduction system in the normal heart.

The AV node serves an important function as a "gatekeeper", limiting the electrical activity that reaches the ventricles. In situations where the atria generate excessively rapid electrical activity (such as atrial fibrillation or atrial flutter), the AV node limits the number of signals conducted to the ventricles. For example, if the atria are electrically activated at 300 beats per minute, half those electrical impulses may be blocked by the AV node, so that the ventricles are stimulated at only 150 beats per minute—resulting in a pulse of 150 beats per minute.
Another important property of the AV node is that it slows down individual electrical impulses. This is manifested on the electrocardiogram as the PR interval (the time from electrical activation of the atria to electrical activation of the ventricles), which is usually shortened to less than 120 milliseconds in duration.
Electrical Activity in WPW
The accessory pathway communicates between the atria and ventricle. The accessory pathway can remain a bystander; however, problems may arise when this pathway creates an electrical circuit that bypasses the AV node. When an aberrant electrical connection occurs via the bundle of Kent, tachycardia may therefore result.
Shown below is an image depicting the normal conduction of electrical signals in heart versus that in the presence of an accessory pathway.
The conduction through the accessory pathway can be:
- Bidirectional (most commonly): retrogarde (also known as concealed) as well as antegrade (also known as manifest, responsible for the ECG findings of delta wave and short PR interval)
- Only retrogarde (less common)
- Only antegrade (least common)
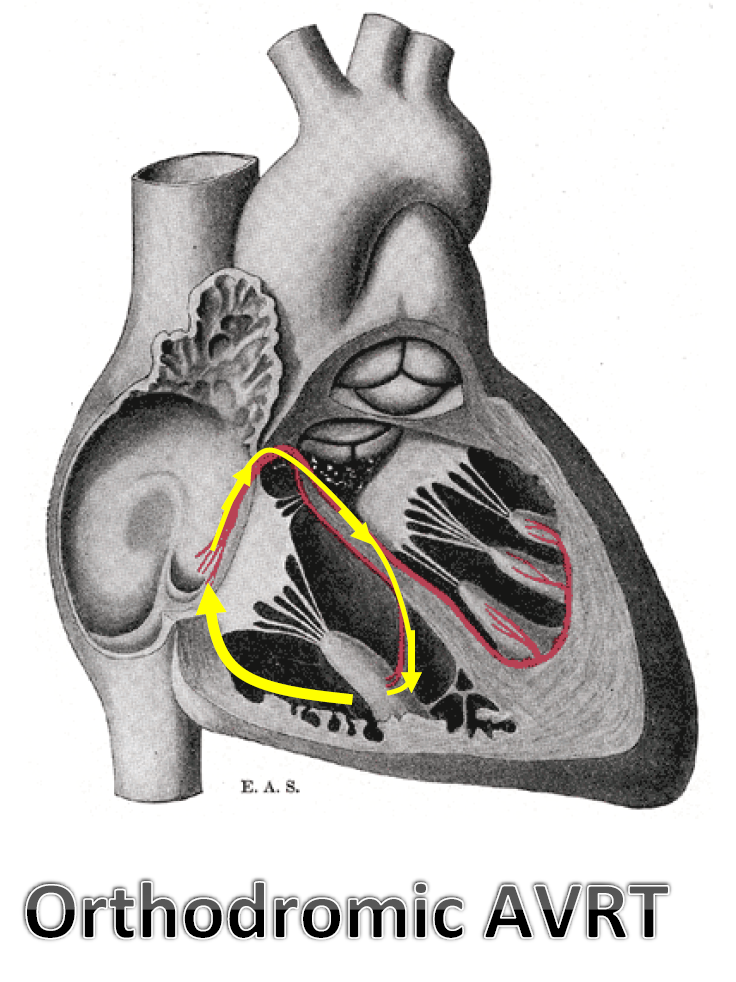
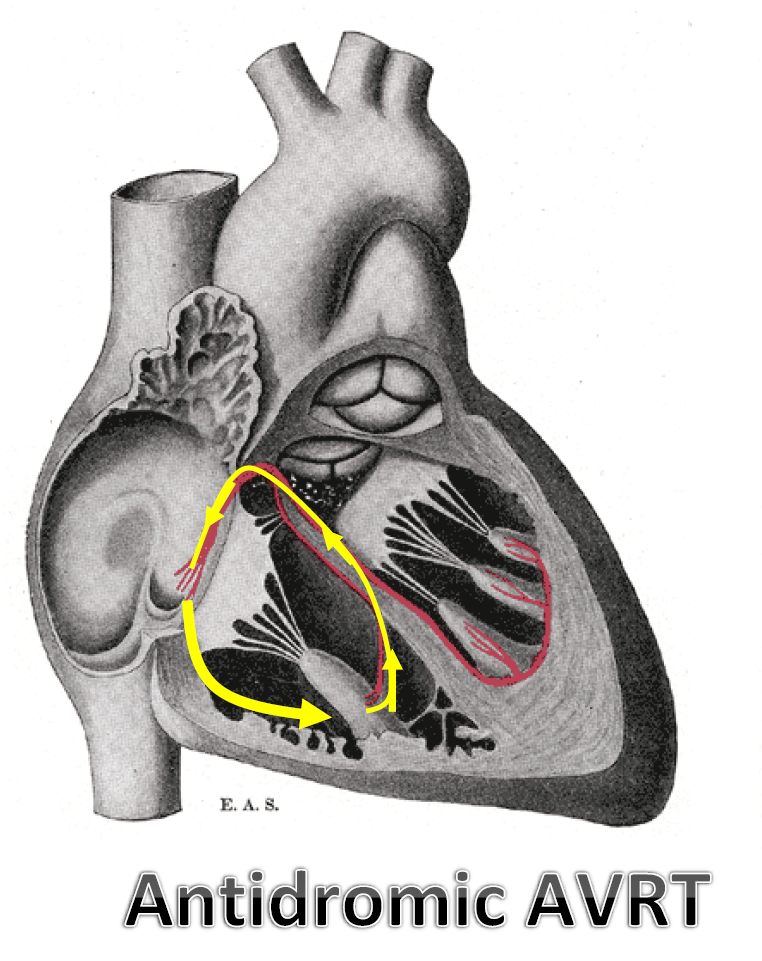
When arrhythmia occurs in a patient with an accessory pathway, the patient is said to have WPW syndrome. The most common type of tachycardia associated with WPW is atrioventricular reciprocating tachycardia (AVRT). AVRT in WPW can be one of two types:
- Orthodromic (~95%): the antegrade electrical signal moves from the atria to the ventricles through the AV node, whereas the retrograde electrical signal moves from the ventricles to the atria through the accessory pathway.
- Antidromic (~5%): the antegrade electrical signal moves from the atria to the ventricles through the accessory pathway, whereas the retrograde electrical signal moves from the ventricles to the atria through either the AV node or a second accessory pathway.
Shown below are two images depicting the difference in the antegrade and retrograde conduction of the electrical signals in orthodromic and antidromic AVRT.
 |
|
Other arrhythmia can occur in patients with WPW, such as atrial tachycardia, atrial flutter, atrial fibrillation, AVNRT. In these arrhythmia, the accessory pathway may act as a bystander. However, since the accessory pathway does not share the rate-slowing properties of the AV node, and may conduct electrical activity at a significantly higher rate than the AV node, the combination of an accessory pathway and cardiac arrhythmia can trigger ventricular fibrillation, a leading cause of sudden cardiac death. For instance, if an individual had an atrial rate of 300 beats per minute, the accessory bundle may conduct all the electrical impulses from the atria to the ventricles, causing the ventricles to contract at 300 beats per minute. Extremely rapid heart rates such as this may result in hemodynamic instability or cardiogenic shock.
Genetics
- Most cases of Wolff-Parkinson-White syndrome occur in people with no apparent family history of the condition. These cases are described as sporadic and are not inherited.
- Familial Wolff-Parkinson-White syndrome accounts for only a small percentage of all cases of this condition. The familial form of the disorder typically has an autosomal dominant pattern of inheritance, which means one copy of the altered gene in each cell is sufficient to cause the condition. In most cases, a person with familial Wolff-Parkinson-White syndrome has inherited the condition from an affected parent.[5]
- While the cause of Wolff-Parkinson-White syndrome is unknown in most cases, a small percentage of all cases of Wolff-Parkinson-White syndrome are caused by mutations in the PRKAG2 gene. Some people with these mutations also have features of hypertrophic cardiomyopathy. The PRKAG2 gene encodes the protein AMP-activated protein kinase (AMPK) gamma-2 subunit. This enzyme helps sense and responds to energy demands within cells. It is likely involved in the development of the heart before birth, although its role in this process is unknown.[5]
- Researchers are uncertain how PRKAG2 mutations lead to the development of Wolff-Parkinson-White syndrome and related heart abnormalities. Research suggests that these mutations alter the activity of AMP-activated protein kinase in the heart, although it is unclear whether the genetic changes overactivate the enzyme or reduce its activity. Studies indicate that changes in AMP-activated protein kinase activity allow glycogen to build up abnormally within cardiac muscle cells. It has been reported that patients with familial WPW usually have increased amounts of glycogen in the myocardial tissue. Other studies have found that altered AMP-activated protein kinase activity is related to changes in the regulation of certain ion channels in the heart. These channels, which transport positively charged atoms (ions) into and out of cardiac muscle cells, play critical roles in maintaining the heart's normal rhythm.[5][6]
Associated Conditions
WPW syndrome is associated with the following disorders:
- Ebstein's anomaly[7][8][9]
- Mitral valve prolapse: This cardiac disorder, if present, is associated with left-sided accessory pathways.[10]
- Hypertrophic cardiomyopathy: This disorder is associated with familial/inherited form of WPW syndrome.[11]
- Hypokalemic periodic paralysis[5]
- Pompe disease[5]
- Tuberous sclerosis[5]
References
- ↑ Sorbo MD, Buja GF, Miorelli M, Nistri S, Perrone C, Manca S, Grasso F, Giordano GM, Nava A (1995). "The prevalence of the Wolff–Parkinson–White syndrome in a population of 116,542 young males". Giornale Italiano di Cardiologia (in Italian). 25 (6): 681–7. PMID 7649416.
- ↑ Munger TM, Packer DL, Hammill SC, Feldman BJ, Bailey KR, Ballard DJ, Holmes DR Jr, Gersh BJ (1993). "A population study of the natural history of Wolff–Parkinson–White syndrome in Olmsted County, Minnesota, 1953–1989". Circulation. 87 (3): 866–73. doi:10.1161/01.CIR.87.3.866. PMID 8443907.
- ↑ americanheart.org Atrial and Ventricular Depolarization Changes Last updated 11/24/2008.
- ↑ Obel OA, Camm AJ (1998). "Accessory pathway reciprocating tachycardia". Eur Heart J. 19 Suppl E: E13–24, E50–1. PMID 9717020.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 "Wolff-Parkinson-White syndrome - Genetics Home Reference". Retrieved 15 April 2014.
- ↑ Sidhu, J.; Roberts, R. (2003). "Genetic basis and pathogenesis of familial WPW syndrome". Indian Pacing Electrophysiol J. 3 (4): 197–201. PMID 16943919.
- ↑ Rao MP, Panduranga P, Al-Mukhaini M, Al-Jufaili M (2012). "Ebstein anomaly in an adult presenting with wide QRS tachycardia: diagnostic and therapeutic dilemmas". Am J Emerg Med. 30 (5): 834.e1–4. doi:10.1016/j.ajem.2011.03.001. PMID 21570234. Unknown parameter
|month=ignored (help) - ↑ Bayar N, Canbay A, Uçar O, Aydoğdu S, Diker E (2010). "[Association of Gerbode-type defect and Wolff-Parkinson-White syndrome with Ebstein's anomaly]". Anadolu Kardiyol Derg (in Turkish). 10 (1): 88–90. PMID 20150013. Unknown parameter
|month=ignored (help) - ↑ Legius B, Van De Bruaene A, Van Deyk K; et al. (2010). "Behavior of Ebstein's anomaly: single-center experience and midterm follow-up". Cardiology. 117 (2): 90–5. doi:10.1159/000318041. PMID 20924185.
- ↑ Savini E, Capone PL (1994). "[Wolff-Parkinson-White, a study on the prevalence of the site of accessory pathways: relations between stability of pre-excitation, symptoms, cardiac arrhythmias and association of mitral valve prolapse with localization of pre-excitation]". Minerva Cardioangiol (in Italian). 42 (7–8): 339–43. PMID 7970027.
- ↑ Kruchina TK, Vasichkina ES, Egorov DF, Tatarskiĭ BA (2012). "[Asymptomatic ventricular pre-excitation in children: a 17 year follow-up study]". Kardiologiia (in Russian). 52 (5): 30–6. PMID 22839583.