WBR0458: Difference between revisions
Rim Halaby (talk | contribs) No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{WBRQuestion | {{WBRQuestion | ||
|QuestionAuthor={{Rim}} | |QuestionAuthor={{Rim}}, {{Alison}} | ||
|ExamType=USMLE Step 1 | |ExamType=USMLE Step 1 | ||
|MainCategory=Pathology | |MainCategory=Pathology | ||
| Line 20: | Line 20: | ||
|MainCategory=Pathology | |MainCategory=Pathology | ||
|SubCategory=Hematology, Oncology | |SubCategory=Hematology, Oncology | ||
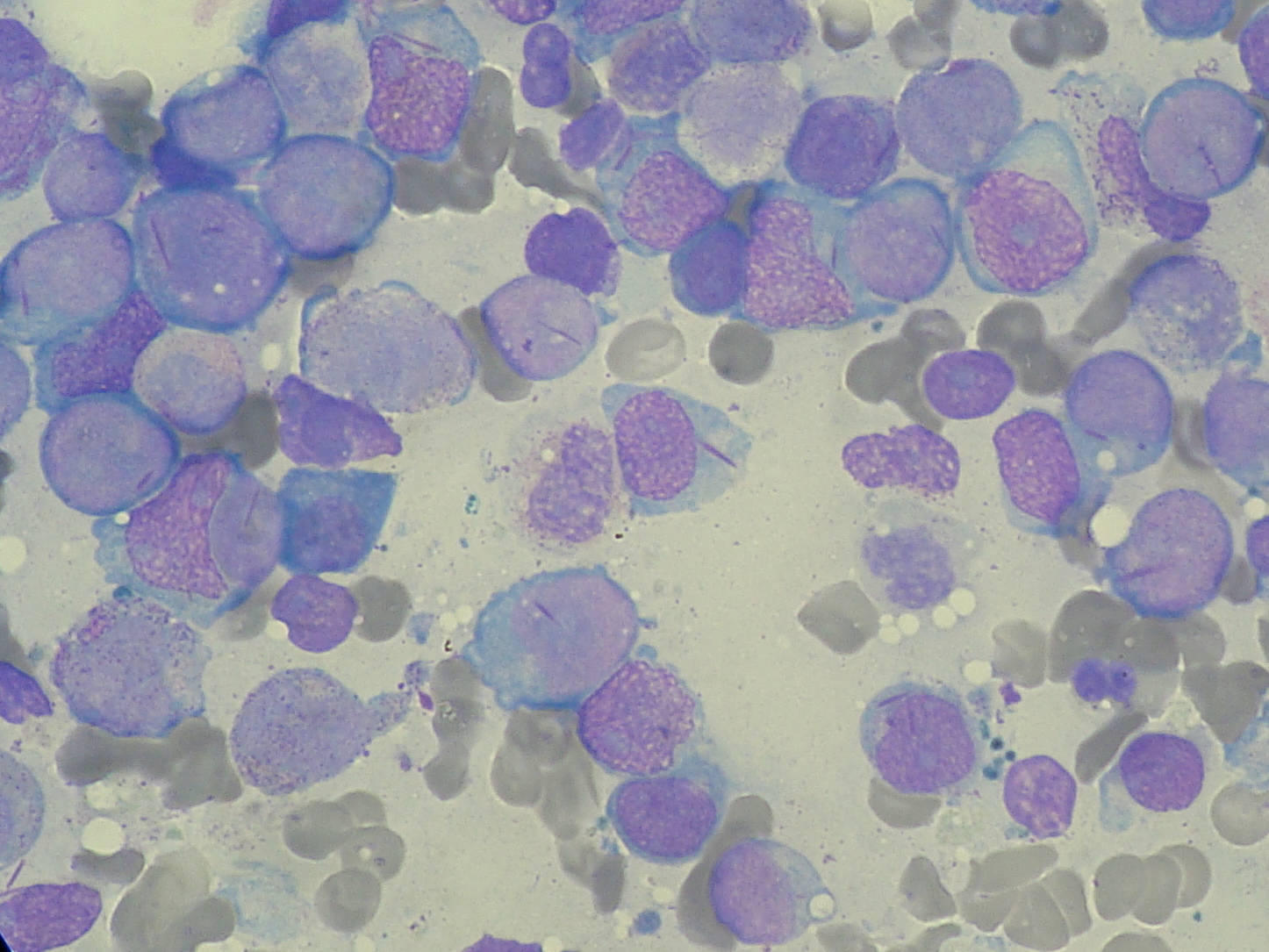
|Prompt=A 24 year old male patient | |Prompt=A 24-year-old male patient to the physician’s office with complaints of fatigue, unremitting fever, and easy bruisability upon minor trauma. His vital signs demonstrate a temperature of 38.6 °C, heart rate of 98 beats per minute, and blood pressure measuring 116/82 mmHg. Upon physical examination, you observe pallor, bleeding gums, and purpura. An image of the patient’s peripheral blood smear is displayed below. Following the initiation of appropriate treatment, the patient suffers a complication. Which of the following best characterizes the patient’s complication? | ||
[[Image:Auer_Rod.JPG|400px]] | [[Image:Auer_Rod.JPG|400px]] | ||
|Explanation=[[Image:WBR Auer Rods Sign.jpg|400px]] | |Explanation=[[Image:WBR Auer Rods Sign.jpg|400px]] | ||
The patient is presenting with [[acute promyelocytic leukemia]] ([[APML]]) or [[AML M3]]. Symptoms of [[AML M3]] are typically unremitting fever with signs of [[pancytopenia]] | The patient in this scenario is likely presenting with [[acute promyelocytic leukemia]] ([[APML]]) or [[AML M3]]. Symptoms of [[AML M3]] are typically unremitting fever with signs of [[pancytopenia]], such as [[anemia]] as manifested by pallor, [[thrombocytopenia]] as manifested by easy bruisibility and [[purpura]], and [[leucopenia]] as manifested by [[sore throat]], [[pneumonia]], or other infections. On peripheral smear, [[AML M3]] is frequently characterized by [[Auer rods]]. The image above displays one circled [[Auer rod]], as well as several others that are not circled. Treatment of [[AML M3]] by [[all-trans retinoic acid]] leads to the release of [[Auer rods]] and potentially results in [[disseminted intravascular coagulation]] ([[DIC]]). | ||
[[DIC]] | [[DIC]], a complication of several diseases including [[AML M3]], occurs following treatment and is characterized by activation of the [[hemostasis]] system, with the release of [[tissue factor]] usually from [[endothelial cells]]. Normally, the inhibitor system compensates for the tissue factor release, but with the eventual consumption of inhibitors more coagulation ensues in a process called “[[consumptive coagulopathy]]”. | ||
As a result, the entire [[hemostasis]] pathway becomes unbalanced and breaks down. | As a result, the entire [[hemostasis]] pathway becomes unbalanced and breaks down. [[DIC]] frequently manifests with profuse bleeding and upon blood work-up, low [[fibrinogen]] levels, elevated levels of [[D-dimer]], and [[fibrinogen split products]] ([[FSP]]), suggesting the generation of [[plasmin]]. [[Consumptive coagulopathy]] is corrected with [[cryoprecipitate]], [[platelet]] concentrations, and [[fresh frozen plasma]] ([[FFP]]), which reduces the tendency to bleed. | ||
|EducationalObjectives= [[AML M3]] is frequently characterized by pancytopenia and fever, with a peripheral blood smear displaying plasma cells containing [[Auer rods]]. [[DIC]] is a common complication following treatment of [[AML M3]], due to the release of [[Auer rods]]. [[DIC]], a consumptive coagulopathy, is caused by the imbalance of the hemostasis and fibrinolytic systems. | |||
AML M3 is characterized by pancytopenia and fever with peripheral blood smear | |References= Mammen EF. Disseminated intravascular coagulation (DIC). Clin Lab Sci. 2000;13(4):239-45 | ||
|AnswerA=Activation of hemostasis and fibrinolysis that leads to formation of thrombin and plasmin | |||
|AnswerAExp=See explanation. | |||
|AnswerA=Activation of hemostasis and fibrinolysis that | |||
|AnswerAExp= | |||
|AnswerB=Autoimmune antibodies against platelets | |AnswerB=Autoimmune antibodies against platelets | ||
|AnswerBExp=Idiopathic thrombocytopenic purpura (ITP) | |AnswerBExp=[[Idiopathic thrombocytopenic purpura]] (ITP), characterized by the presence of autoimmune antibodies against platelets, typically occurs following a viral illness. | ||
|AnswerC=Systemic deposition of platelet thrombi with abundant von Willebrand factor (vWF) in arterioles and capillaries | |AnswerC=Systemic deposition of platelet thrombi with abundant von Willebrand factor (vWF) in arterioles and capillaries | ||
|AnswerCExp=Thrombotic thrombocytopenic purpura (TTP) is characterized by the systemic deposition of platelet thrombi with abundant von Willebrand factor (vWF) in arterioles and capillaries. | |AnswerCExp=[[Thrombotic thrombocytopenic purpura]] (TTP) is characterized by the systemic deposition of [[platelet thrombi]] with abundant [[von Willebrand factor]] (vWF) in arterioles and capillaries. | ||
|AnswerD=Increased ristocetin sensitivity | |AnswerD=Increased ristocetin sensitivity | ||
|AnswerDExp=von | |AnswerDExp=[[von Willebrand disease]] (vWD) is characterized by an increased sensitivity to ristocetin. | ||
|AnswerE=Monoclonal gammopathy of undetermined significance | |AnswerE=Monoclonal gammopathy of undetermined significance | ||
|AnswerEExp=Monoclonal gammopathy of undetermined significance (MGUS) | |AnswerEExp=[[Monoclonal gammopathy of undetermined significance]] (MGUS), a hematologic condition, is characterized by the presence of monoclonal antibodies without clinical symptoms, or radiological and laboratory signs. The disease is similar to multiple myeloma (MM), but the number of monoclonal plasma cells in MGUS is lower, constituting less than 10% of bone marrow biopsy findings. MGUS requires no treatment, but the rate of MM development is approximately 1-2% in patients with MGUS. | ||
|RightAnswer=A | |RightAnswer=A | ||
|WBRKeyword=AML | |WBRKeyword=AML M3, DIC, disseminated intravascular coagulation, acute myelocytic leukemia, acute promyelocytic leukemia, monoclonal, gammopathy, cancer, fibrinogen, | ||
|Approved= | |Approved=Yes | ||
}} | }} | ||
Revision as of 19:04, 23 July 2014
| Author | [[PageAuthor::Rim Halaby, M.D. [1], (Reviewed by Alison Leibowitz)]] |
|---|---|
| Exam Type | ExamType::USMLE Step 1 |
| Main Category | MainCategory::Pathology |
| Sub Category | SubCategory::Hematology, SubCategory::Oncology |
| Prompt | [[Prompt::A 24-year-old male patient to the physician’s office with complaints of fatigue, unremitting fever, and easy bruisability upon minor trauma. His vital signs demonstrate a temperature of 38.6 °C, heart rate of 98 beats per minute, and blood pressure measuring 116/82 mmHg. Upon physical examination, you observe pallor, bleeding gums, and purpura. An image of the patient’s peripheral blood smear is displayed below. Following the initiation of appropriate treatment, the patient suffers a complication. Which of the following best characterizes the patient’s complication? |
| Answer A | AnswerA::Activation of hemostasis and fibrinolysis that leads to formation of thrombin and plasmin |
| Answer A Explanation | AnswerAExp::See explanation. |
| Answer B | AnswerB::Autoimmune antibodies against platelets |
| Answer B Explanation | [[AnswerBExp::Idiopathic thrombocytopenic purpura (ITP), characterized by the presence of autoimmune antibodies against platelets, typically occurs following a viral illness.]] |
| Answer C | AnswerC::Systemic deposition of platelet thrombi with abundant von Willebrand factor (vWF) in arterioles and capillaries |
| Answer C Explanation | [[AnswerCExp::Thrombotic thrombocytopenic purpura (TTP) is characterized by the systemic deposition of platelet thrombi with abundant von Willebrand factor (vWF) in arterioles and capillaries.]] |
| Answer D | AnswerD::Increased ristocetin sensitivity |
| Answer D Explanation | [[AnswerDExp::von Willebrand disease (vWD) is characterized by an increased sensitivity to ristocetin.]] |
| Answer E | AnswerE::Monoclonal gammopathy of undetermined significance |
| Answer E Explanation | [[AnswerEExp::Monoclonal gammopathy of undetermined significance (MGUS), a hematologic condition, is characterized by the presence of monoclonal antibodies without clinical symptoms, or radiological and laboratory signs. The disease is similar to multiple myeloma (MM), but the number of monoclonal plasma cells in MGUS is lower, constituting less than 10% of bone marrow biopsy findings. MGUS requires no treatment, but the rate of MM development is approximately 1-2% in patients with MGUS.]] |
| Right Answer | RightAnswer::A |
| Explanation | [[Explanation::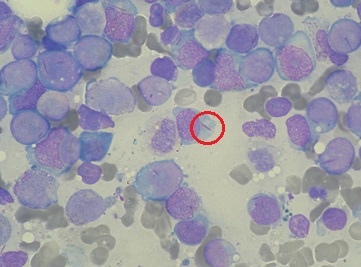
The patient in this scenario is likely presenting with acute promyelocytic leukemia (APML) or AML M3. Symptoms of AML M3 are typically unremitting fever with signs of pancytopenia, such as anemia as manifested by pallor, thrombocytopenia as manifested by easy bruisibility and purpura, and leucopenia as manifested by sore throat, pneumonia, or other infections. On peripheral smear, AML M3 is frequently characterized by Auer rods. The image above displays one circled Auer rod, as well as several others that are not circled. Treatment of AML M3 by all-trans retinoic acid leads to the release of Auer rods and potentially results in disseminted intravascular coagulation (DIC). DIC, a complication of several diseases including AML M3, occurs following treatment and is characterized by activation of the hemostasis system, with the release of tissue factor usually from endothelial cells. Normally, the inhibitor system compensates for the tissue factor release, but with the eventual consumption of inhibitors more coagulation ensues in a process called “consumptive coagulopathy”. As a result, the entire hemostasis pathway becomes unbalanced and breaks down. DIC frequently manifests with profuse bleeding and upon blood work-up, low fibrinogen levels, elevated levels of D-dimer, and fibrinogen split products (FSP), suggesting the generation of plasmin. Consumptive coagulopathy is corrected with cryoprecipitate, platelet concentrations, and fresh frozen plasma (FFP), which reduces the tendency to bleed. |
| Approved | Approved::Yes |
| Keyword | WBRKeyword::AML M3, WBRKeyword::DIC, WBRKeyword::disseminated intravascular coagulation, WBRKeyword::acute myelocytic leukemia, WBRKeyword::acute promyelocytic leukemia, WBRKeyword::monoclonal, WBRKeyword::gammopathy, WBRKeyword::cancer, WBRKeyword::fibrinogen |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |