WBR0088: Difference between revisions
Rim Halaby (talk | contribs) No edit summary |
m (refreshing WBR questions) |
||
| (5 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{WBRQuestion | {{WBRQuestion | ||
|QuestionAuthor={{Ochuko}} (Reviewed by Will Gibson, [[user: Jad Al Danaf|Jad Al Danaf]], {{Rim}}) | |QuestionAuthor= {{Ochuko}} (Reviewed by Yazan Daaboul, Will Gibson, [[user: Jad Al Danaf|Jad Al Danaf]], {{Rim}}) | ||
|ExamType=USMLE Step 1 | |ExamType=USMLE Step 1 | ||
|MainCategory=Microbiology | |MainCategory=Microbiology | ||
| Line 8: | Line 8: | ||
|MainCategory=Microbiology | |MainCategory=Microbiology | ||
|SubCategory=Neurology, Infectious Disease | |SubCategory=Neurology, Infectious Disease | ||
|MainCategory=Microbiology | |||
|MainCategory=Microbiology | |MainCategory=Microbiology | ||
|MainCategory=Microbiology | |MainCategory=Microbiology | ||
| Line 20: | Line 21: | ||
|MainCategory=Microbiology | |MainCategory=Microbiology | ||
|SubCategory=Neurology, Infectious Disease | |SubCategory=Neurology, Infectious Disease | ||
|Prompt=A 38-year old | |Prompt=A 38-year-old man is brought to the emergency department by his wife with complaints of excessive thirst, fear of drinking water, and disorientation. She reports that he also had three episodes of seizures in the past few days. Three days after his admission, the patient experiences vivid visual hallucinations, lapses into a coma, and dies despite appropriate resuscitative measures. Which of the following cell surface molecules is most likely involved in this patient's condition? | ||
|Explanation= | |Explanation=Rabies is a bullet-shaped viral ''zoonosis'' of lyssavirus family that is transmitted via saliva of an infected animal bite. Although classically associated with dog bites, exposure to rabies in USA is mostly due to infected wild animals, such as bats, foxes, raccoons, skunks, and wolves. The incubation period in humans is highly variable (days to years), but is usually between 3-8 weeks. In animals, incubation period is shorter, ranging between 4-7 days. | ||
Rabies virus may manifest as "furious" (encephalitic) rabies or as "paralytic" rabies. Furious rabies is a more common form, characterized by the presence of pain and paresthesia at the site of bite, agitation, fever, muscular spasms of muscles of swallowing due to exposure to water (hydrophobia) and air (aerophobia), hypersalivation, and hallucinations. These symptoms are followed by seizures, impaired consciousness, coma, and death. Both hydrophobia and aerophobia, along with photophobia, autonomic dysfunction and hyperexcitability, suggest the presence of rabies encephalitis. In contrast, paralytic rabies is characterized by symmetric or asymmetric ascending limb and respiratory muscle paralysis, possible hydrophobia/aerophobia, and death but no prior impairment of consciousness. | |||
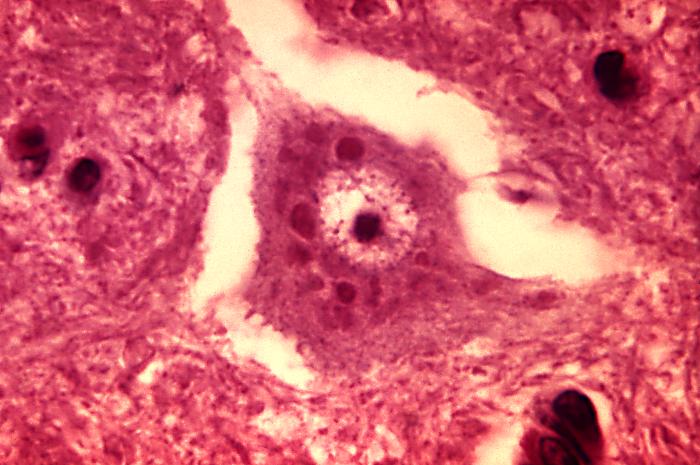
The patient in this vignette has [[rabies]] encephalitis. After the bite from an infected animal, the virus infiltrates peripheral nerves by binding to nicotinic [[acetylcholine receptors]] at the site of inoculation. The virus moves by retrograde axoplasmic transport to dorsal root ganglia and the [[spinal cord]]. The brain becomes rapidly infected when the virus gets to the spinal cord. On autopsy, infected Purkinje cerebellar cells and hippocampal neurons will display cytoplasmic inclusions called [[negri bodies]] (pictured below). Treatment for suspected rabies infection consists of post-exposure prophylaxis, including wound debridement, prophylactic vaccination ([[active immunity]]) and anti-rabies IgG ([[passive immunity]]). Once symptoms develop, rabies is almost invariably fatal. | |||
[[File:Rabies encephalitis Negri bodies PHIL 3377 lores.jpg | 400px |alt= Courtesy of CDC]] | [[File:Rabies encephalitis Negri bodies PHIL 3377 lores.jpg | 400px |alt= Courtesy of CDC]] | ||
|AnswerA=SNARE proteins | |AnswerA=SNARE proteins | ||
|AnswerAExp=[[SNARE]] proteins are responsible for neurotransmitter release at synaptic junctions. [[Clostridium tetani]] and [[ | |AnswerAExp=[[SNARE]] proteins are responsible for neurotransmitter release at synaptic junctions. ''[[Clostridium tetani]]'' and ''[[Clostridium botulinum]]'' produce [[toxins]] that cleave SNARE proteins and thereby cause [[paralysis]]. | ||
|AnswerB=CD4 receptors | |AnswerB=CD4 receptors | ||
|AnswerBExp=[[HIV-1]] binds to [[CD4]] through its viral envelope protein [[gp120]] to gain entry into host T-cells. The number of CD4-positive [[T cells]] in the blood is a marker of disease progression in [[HIV]] infected patients. | |AnswerBExp=[[HIV-1]] binds to [[CD4]] of T-cells through its viral envelope protein [[gp120]] to gain entry into host T-cells. The number of CD4-positive [[T cells]] in the blood is a marker of disease progression in [[HIV]] infected patients. | ||
|AnswerC=LDL receptors | |AnswerC=LDL receptors | ||
|AnswerCExp=[[LDL receptor]] mutations cause [[familial hypercholesterolemia]], an [[autosomal dominant]] lipid disorder. Familial hypercholesterolemia is associated with accelerated [[atherosclerosis]], tendon (Achilles) [[xanthomas]] and [[corneal arcus]]. | |AnswerCExp=[[LDL receptor]] mutations cause [[familial hypercholesterolemia]], an [[autosomal dominant]] lipid disorder. Familial hypercholesterolemia is associated with accelerated [[atherosclerosis]], tendon (Achilles) [[xanthomas]], and [[corneal arcus]]. | ||
|AnswerD=CCR5 receptors | |AnswerD=CCR5 receptors | ||
|AnswerDExp=[[CCR5 receptor]] is a co-receptor for [[HIV]] found on [[macrophages]] and [[Th cells]]. | |AnswerDExp=[[CCR5 receptor]] is a co-receptor for [[HIV]] found on [[macrophages]] and [[Th cells]]. Individuals with CCR5 mutations are protected from [[HIV]] infection. | ||
|AnswerE=Acetylcholine receptors | |AnswerE=Acetylcholine receptors | ||
|AnswerEExp=The [[rabies]] virus binds to nicotinic [[acetylcholine receptors]] to travel from peripheral nerves to the | |AnswerEExp=The [[rabies]] virus binds to nicotinic [[acetylcholine receptors]] to travel from peripheral nerves to the central nervous system. | ||
|EducationalObjectives=The rabies virus binds to [[ | |EducationalObjectives=The rabies virus binds to nicotinic [[acetylcholine receptors]] to travel from [[peripheral nerves]] to the [[brain]]. Symptoms include [[insomnia]], [[anxiety]], [[confusion]], slight or partial paralysis, excitation, [[hallucinations]], [[agitation]], hypersalivation. [[Hydrophobia]] and [[aerophobia]] are specific symptoms of rabies that suggest rabies encephalitis. | ||
|References= | |References=Depani SJ, Kennedy N, Mallewa M, Molyneux EM. Case report: Evidence of rise in rabies cases in Sourther Malawi - Better preventative measures are urgently required. Malawi Medical Journal. 2012;24(3):61-4. | ||
Lentz TL. Rabies virus binding to an acetylcholine receptor alpha-subunit peptide. J Mol Recognit. 1990;3(2):82-8. | |||
Rupprecht CE, Hanlon CA, Hemachudha T. Rabies re-examined. Lancet Infectious Diseases. 2002;2:327-43. | |||
First Aid 2014 page 165 | |||
|RightAnswer=E | |RightAnswer=E | ||
|WBRKeyword=Rabies, Virus, Viruses, Microbiology, Neurodegenerative, Hallucination, Seizure | |WBRKeyword=Rabies, Virus, Viruses, Microbiology, Neurodegenerative, Hallucination, Seizure, hydrophobia, aerophobia, fear, drinking, water, thirst, thirsty, negri, bodies, bullet, shaped, lyssavirus, zoonosis, retrograde, purkinje, cerebellum, hippocampal, hippocampus, neuron, neurons, dog, bat, raccoon, skunk, fox, | ||
|Approved=Yes | |Approved=Yes | ||
}} | }} | ||
Latest revision as of 23:18, 27 October 2020
| Author | [[PageAuthor::Ogheneochuko Ajari, MB.BS, MS [1] (Reviewed by Yazan Daaboul, Will Gibson, Jad Al Danaf, Rim Halaby, M.D. [2])]] |
|---|---|
| Exam Type | ExamType::USMLE Step 1 |
| Main Category | MainCategory::Microbiology |
| Sub Category | SubCategory::Neurology, SubCategory::Infectious Disease |
| Prompt | [[Prompt::A 38-year-old man is brought to the emergency department by his wife with complaints of excessive thirst, fear of drinking water, and disorientation. She reports that he also had three episodes of seizures in the past few days. Three days after his admission, the patient experiences vivid visual hallucinations, lapses into a coma, and dies despite appropriate resuscitative measures. Which of the following cell surface molecules is most likely involved in this patient's condition?]] |
| Answer A | AnswerA::SNARE proteins |
| Answer A Explanation | [[AnswerAExp::SNARE proteins are responsible for neurotransmitter release at synaptic junctions. Clostridium tetani and Clostridium botulinum produce toxins that cleave SNARE proteins and thereby cause paralysis.]] |
| Answer B | AnswerB::CD4 receptors |
| Answer B Explanation | [[AnswerBExp::HIV-1 binds to CD4 of T-cells through its viral envelope protein gp120 to gain entry into host T-cells. The number of CD4-positive T cells in the blood is a marker of disease progression in HIV infected patients.]] |
| Answer C | AnswerC::LDL receptors |
| Answer C Explanation | [[AnswerCExp::LDL receptor mutations cause familial hypercholesterolemia, an autosomal dominant lipid disorder. Familial hypercholesterolemia is associated with accelerated atherosclerosis, tendon (Achilles) xanthomas, and corneal arcus.]] |
| Answer D | AnswerD::CCR5 receptors |
| Answer D Explanation | [[AnswerDExp::CCR5 receptor is a co-receptor for HIV found on macrophages and Th cells. Individuals with CCR5 mutations are protected from HIV infection.]] |
| Answer E | AnswerE::Acetylcholine receptors |
| Answer E Explanation | [[AnswerEExp::The rabies virus binds to nicotinic acetylcholine receptors to travel from peripheral nerves to the central nervous system.]] |
| Right Answer | RightAnswer::E |
| Explanation | [[Explanation::Rabies is a bullet-shaped viral zoonosis of lyssavirus family that is transmitted via saliva of an infected animal bite. Although classically associated with dog bites, exposure to rabies in USA is mostly due to infected wild animals, such as bats, foxes, raccoons, skunks, and wolves. The incubation period in humans is highly variable (days to years), but is usually between 3-8 weeks. In animals, incubation period is shorter, ranging between 4-7 days.
Rabies virus may manifest as "furious" (encephalitic) rabies or as "paralytic" rabies. Furious rabies is a more common form, characterized by the presence of pain and paresthesia at the site of bite, agitation, fever, muscular spasms of muscles of swallowing due to exposure to water (hydrophobia) and air (aerophobia), hypersalivation, and hallucinations. These symptoms are followed by seizures, impaired consciousness, coma, and death. Both hydrophobia and aerophobia, along with photophobia, autonomic dysfunction and hyperexcitability, suggest the presence of rabies encephalitis. In contrast, paralytic rabies is characterized by symmetric or asymmetric ascending limb and respiratory muscle paralysis, possible hydrophobia/aerophobia, and death but no prior impairment of consciousness. The patient in this vignette has rabies encephalitis. After the bite from an infected animal, the virus infiltrates peripheral nerves by binding to nicotinic acetylcholine receptors at the site of inoculation. The virus moves by retrograde axoplasmic transport to dorsal root ganglia and the spinal cord. The brain becomes rapidly infected when the virus gets to the spinal cord. On autopsy, infected Purkinje cerebellar cells and hippocampal neurons will display cytoplasmic inclusions called negri bodies (pictured below). Treatment for suspected rabies infection consists of post-exposure prophylaxis, including wound debridement, prophylactic vaccination (active immunity) and anti-rabies IgG (passive immunity). Once symptoms develop, rabies is almost invariably fatal.
Lentz TL. Rabies virus binding to an acetylcholine receptor alpha-subunit peptide. J Mol Recognit. 1990;3(2):82-8. Rupprecht CE, Hanlon CA, Hemachudha T. Rabies re-examined. Lancet Infectious Diseases. 2002;2:327-43. First Aid 2014 page 165]] |
| Approved | Approved::Yes |
| Keyword | WBRKeyword::Rabies, WBRKeyword::Virus, WBRKeyword::Viruses, WBRKeyword::Microbiology, WBRKeyword::Neurodegenerative, WBRKeyword::Hallucination, WBRKeyword::Seizure, WBRKeyword::hydrophobia, WBRKeyword::aerophobia, WBRKeyword::fear, WBRKeyword::drinking, WBRKeyword::water, WBRKeyword::thirst, WBRKeyword::thirsty, WBRKeyword::negri, WBRKeyword::bodies, WBRKeyword::bullet, WBRKeyword::shaped, WBRKeyword::lyssavirus, WBRKeyword::zoonosis, WBRKeyword::retrograde, WBRKeyword::purkinje, WBRKeyword::cerebellum, WBRKeyword::hippocampal, WBRKeyword::hippocampus, WBRKeyword::neuron, WBRKeyword::neurons, WBRKeyword::dog, WBRKeyword::bat, WBRKeyword::raccoon, WBRKeyword::skunk, WBRKeyword::fox |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |