Von Willebrand disease pathophysiology: Difference between revisions
Prince Djan (talk | contribs) |
Prince Djan (talk | contribs) |
||
| Line 60: | Line 60: | ||
*[[Non-Hodgkin lymphoma]] | *[[Non-Hodgkin lymphoma]] | ||
*[[Polycythemia vera]] | *[[Polycythemia vera]] | ||
====Drugs and other agents==== | ====Drugs and other agents==== | ||
| Line 66: | Line 65: | ||
* [[Ciprofloxacin]] | * [[Ciprofloxacin]] | ||
*[[Griseofulvin]] | *[[Griseofulvin]] | ||
====Autoimmune disorders==== | ====Autoimmune disorders==== | ||
Revision as of 20:35, 29 November 2016
|
Von Willebrand disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Von Willebrand disease pathophysiology On the Web |
|
American Roentgen Ray Society Images of Von Willebrand disease pathophysiology |
|
Risk calculators and risk factors for Von Willebrand disease pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Pathophysiology
In healthy individuals, VWF circulates as high-molecular-weight multimers carrying factor VIII. Some persons have mildly reduced VWF levels, which may contribute to a bleeding phenotype but are not necessarily caused by defects in the VWF gene. Persons with low VWF levels and a bleeding tendency are classified as having low VWF, rather than von Willebrand’s disease (VWD). There is a partial deficiency of functionally normal VWF in type 1 VWD and a complete deficiency in type 3 disease. This deficiency can result from a reduction in protein synthesis, which is often caused by null alleles (large gene deletions, stop codons, frame-shift mutations, or splice-site mutations) but may also be due to mutations in the promotor regions. Homozygosity or compound heterozygosity for these defects results in type 3 VWD. Some heterozygous carriers have mild symptoms and receive a diagnosis of type 1 disease. However, most cases of type 1 VWD are caused by heterozygous missense mutations that exert a dominant-negative effect because the mutant subunits are incorporated into the multimer together with the normal subunits, resulting in a abnormality of the entire multimer.
Deficiency of vWF shows primarily in organs with extensive small vessels, such as the skin, the gastrointestinal tract and the uterus.
In more severe cases of type 1 vWD, genetic changes are common within the vWF gene and are highly penetrant. In milder cases of type 1 vWD there may be a complex spectrum of molecular pathology in addition to polymorphisms of the vWF gene alone.[1] The individual's ABO blood group can influence presentation and pathology of vWD. Those individuals with blood group O have a lower mean level than individuals with other blood groups. Unless ABO group–specific vWF:antigen reference ranges are used, normal group O individuals can be diagnosed as type I vWD, and some individuals of blood group AB with a genetic defect of vWF may have the diagnosis overlooked because vWF levels are elevated due to blood group.[2]
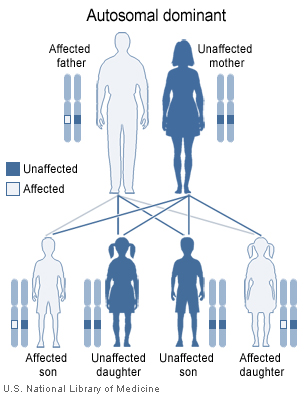
Von Willebrand's Disease is usually inherited in an autosomal dominant manner, although there are recessive forms as well, and it can also be acquired secondary to another disease.[3][4][5][6][7][8][9][10] Acquired VWD is associated with other diseases resulting from different pathological processes.
These pathological processes include:
- Antibody formation resulting in:
- Impaired vWF function
- Increased clearance of VWF
- Enhanced proteolysis
- Decreased synthesis
Genetics
Von Willebrand disease types 1 and 2 (except type 2N which is inherited recessively) are inherited as autosomal dominant traits and type 3 is inherited as autosomal recessive. The diagram below illustrates autosomal dominant inheritance.
 |
- The vWF gene is located on chromosome twelve (12p13.2).
- It has 52 exons spanning 178kbp. *
- VWD Types 1 and 2 are inherited as autosomal dominant traits and type 3 is inherited as autosomal recessive. Occasionally type 2 also inherits recessively.
Associated conditions
Acquired conditions associated with Von Willebrand disease include the following:[11][12][3][4][5][6][7]
- Mitral valve prolapse
- Ventricular assist device
- Ventricular septal defect
- Aortic stenosis
Malignant diseases
- Monoclonal gammopathy of undetermined significance
- Leukemia example chronic myeloid leukemia and chronic lymphocytic leukemia
- Wilms tumor
- Waldenström macroglobulinemia
- Essential thrombocythemia
- Multiple myeloma
- Non-Hodgkin lymphoma
- Polycythemia vera
Drugs and other agents
Autoimmune disorders
Other disorders
References
- ↑ James P, Notley C, Hegadorn C, Leggo J, Tuttle A, Tinlin S, Brown C, Andrews C, Labelle A, Chirinian Y, O'Brien L, Othman M, Rivard G, Rapson D, Hough C, Lillicrap D (2007). "The mutational spectrum of type 1 von Willebrand disease: Results from a Canadian cohort study". Blood. 109 (1): 145–54. doi:10.1182/blood-2006-05-021105. PMID 17190853.
- ↑ Gill, JC (1987). "The effect of ABO blood group on the diagnosis of von Willebrand disease". Blood. 69 (6): 1691–5. PMID 3495304. Unknown parameter
|coauthors=ignored (help) - ↑ 3.0 3.1 Franchini M, Lippi G (2007). "Acquired von Willebrand syndrome: an update". Am J Hematol. 82 (5): 368–75. doi:10.1002/ajh.20830. PMID 17133419.
- ↑ 4.0 4.1 Tiede A, Rand JH, Budde U, Ganser A, Federici AB (2011). "How I treat the acquired von Willebrand syndrome". Blood. 117 (25): 6777–85. doi:10.1182/blood-2010-11-297580. PMID 21540459.
- ↑ 5.0 5.1 Kumar S, Pruthi RK, Nichols WL (2002). "Acquired von Willebrand disease". Mayo Clin Proc. 77 (2): 181–7. doi:10.4065/77.2.181. PMID 11838652.
- ↑ 6.0 6.1 Veyradier A, Jenkins CS, Fressinaud E, Meyer D (2000). "Acquired von Willebrand syndrome: from pathophysiology to management". Thromb Haemost. 84 (2): 175–82. PMID 10959686.
- ↑ 7.0 7.1 Federici AB, Rand JH, Bucciarelli P, Budde U, van Genderen PJ, Mohri H; et al. (2000). "Acquired von Willebrand syndrome: data from an international registry". Thromb Haemost. 84 (2): 345–9. PMID 10959711.
- ↑ Ng et al. Diagnostic Approach to von Willebrand Disease. Blood 2015; 125(13): 2029-2037.
- ↑ Blomback et al. Von Willebrand Disease Biology Hemophilia 2012; 18: 141-147.
- ↑ Favarolo et al. Von Willebrand Disease and Platelet Disorders. Hemophilia 2014; 20: 59-64.
- ↑ Simone JV, Cornet JA, Abildgaard CF (1968). "Acquired von Willebrand's syndrome in systemic lupus erythematosus". Blood. 31 (6): 806–12. PMID 4172730.
- ↑ Wautier JL, Levy-Toledano S, Caen JP (1976). "Acquired von Willebrand's syndrome and thrombopathy in a patient with chronic lymphocytic leukaemia". Scand J Haematol. 16 (2): 128–34. PMID 1083062.