Ventricular tachycardia classification
|
Ventricular tachycardia Microchapters |
|
Differentiating Ventricular Tachycardia from other Disorders |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Ventricular tachycardia classification On the Web |
|
to Hospitals Treating Ventricular tachycardia classification |
|
Risk calculators and risk factors for Ventricular tachycardia classification |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
1. Classification Based Upon Morphology of Complexes
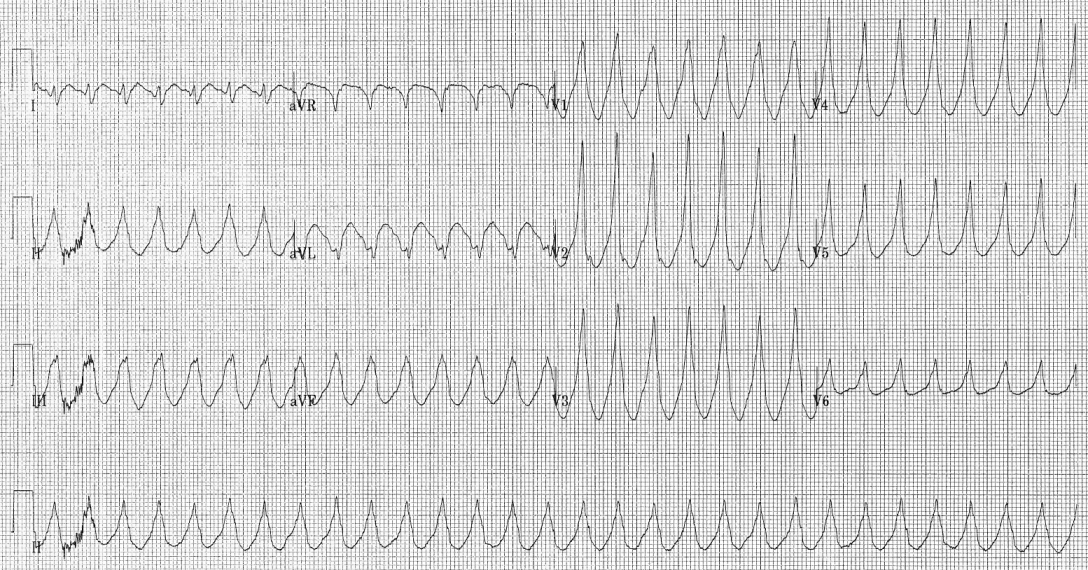
Ventricular tachycardia can be classified based on its morphology: Monomorphic ventricular tachycardia means that the appearance of all the beats match each other in each lead of a surface electrocardiogram (EKG).
Polymorphic ventricular tachycardia, on the other hand, has beat-to-beat variations in morphology. This most commonly appears as a cyclical progressive change in cardiac axis referred to by its French eponym Torsade de pointes (literally twisting of the points).
2. Classification Based Upon Duration of Episode
Another way to classify ventricular tachycardias is the duration of the episodes: Technically, three or more beats in a row on an EKG that originate from the ventricle at a rate of more than 100 beats per minute constitute a ventricular tachycardia. If the fast rhythm self-terminates within 30 seconds, it is considered a non-sustained ventricular tachycardia. If the rhythm lasts more than 30 seconds it is known as a sustained ventricular tachycardia (even if it terminates on its own after 30 seconds).
Sustained Ventricular Tachycardia
- Ventricular tachycardia originates from a ventricular focus
- Lasts more than 30 seconds
- Broad QRS complexes: rate of >90 beats/minute
Paroxysmal Ventricular Tachycardia(Non Sustained Ventricular Tachycardia)
- Rapid succession of three or more ectopic beats.
- Sustained if it lasts longer than 30 seconds.
Incessant Ventricular Tachycardia
- The ventricular tachycardia is recurrent and the episodes are interrupted by only a few sinus beats.
3. Classification Based Upon Symptoms
A third way to classify ventricular tachycardia is on the basis of its symptoms: Pulseless VT is associated with no effective cardiac output, hence, no effective pulse, and is a cause of cardiac arrest. In this circumstance it is best treated the same way as ventricular fibrillation (VF) and is recognized as one of the shockable rhythms on the cardiac arrest protocol. Some VT is associated with reasonable cardiac output and may even be asymptomatic. The heart usually tolerates this rhythm poorly in the medium to long term, and patients may certainly deteriorate to pulseless VT or to VF.