|
|
| (112 intermediate revisions by 2 users not shown) |
| Line 1: |
Line 1: |
| __NOTOC__
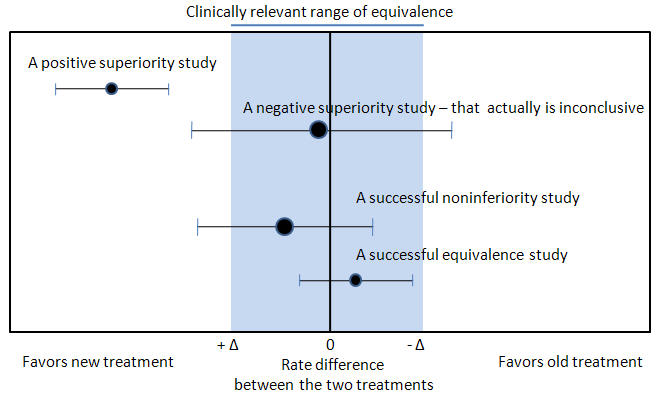
| | {{Image|Noninferiority and equivalency randomized controlled trials.jpg|right|350px|Noninferiority and equivalency randomized controlled trials.}} |
| {{Focal segmental glomerulosclerosis}} | |
| {{CMG}};{{APM}}; '''Associate Editor-In-Chief:’’’ {{CZ}}; {{OO}}
| |
| | |
| ==Overview==
| |
| | |
| ==Pathophysiology==
| |
| The underlying pathogenesis of FSGS clinical signs and symptoms is fusion or effacement of the foot processes ([[podocytes]]) of the [[glomeruli]], with sclerosing of some part of the [[glomeruli]] (hence its name as focal segmental). FSGS is believed to a histological variant of Minimal Change Kidney Disease rather than a clinical disease by itself.
| |
| The clinical hallmark of focal segmental glomerulosclerosis (FSGS) is [[proteinuria]] and [[nephrotic syndrome]]. As such, the involvement of the permselective filtration barrier and effacement of podocyte foot processes are inevitable.<ref name="pmid14712353">{{cite journal| author=Asanuma K, Mundel P| title=The role of podocytes in glomerular pathobiology. | journal=Clin Exp Nephrol | year= 2003 | volume= 7 | issue= 4 | pages= 255-9 | pmid=14712353 | doi=10.1007/s10157-003-0259-6 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14712353 }} </ref>
| |
| According to Asanuma and colleagues,<ref name="pmid14712353">{{cite journal| author=Asanuma K, Mundel P| title=The role of podocytes in glomerular pathobiology. | journal=Clin Exp Nephrol | year= 2003 | volume= 7 | issue= 4 | pages= 255-9 | pmid=14712353 | doi=10.1007/s10157-003-0259-6 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14712353 }} </ref> 4 major causes that lead to the reaction of podocyte foot processes. These changes result in [[apoptosis]], detachment from the glomerular basement membrane (GBM), and subsequent podocytopenia:<ref name="pmid12704576"></ref>
| |
| #Interference with slit diaphragm and its corresponding [[lipid raft]]
| |
| #Interference with [[actin]] cytoskeleton
| |
| #Interference with the [[glomerular basement membrane|GBM]] or with the interaction of the [[glomerular basement membrane|GBM]] and the [[podocytes]]
| |
| #Interference with the negative charge of [[podocytes]]
| |
| | |
| The pathogenesis of Primary or Idiopathic FSGS is not so clear. Many studies had theorized that FSGS occurs as a consequence of effects of circulating immune activating factors on the glomerular epithelium. Indeed, the damaging role of circulating factors like the soluble urokinase plasminogen activating receptor (suPAR) on the glomerular podocytes had been postulated.<ref name="pmidPMID 25168830">{{cite journal| author=Reiser J, Nast CC, Alachkar N| title=Permeability factors in focal and segmental glomerulosclerosis. | journal=Adv Chronic Kidney Dis | year= 2014 | volume= 21 | issue= 5 | pages= 417-21 | pmid=PMID 25168830 | doi=10.1053/j.ackd.2014.05.010 | pmc=4149759 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25168830 }} </ref> However, there are not enough clinical data to support this pathogenic theory probably because of the several other physiologic forms of suPAR that can be identified by [[ELISA]].<ref name="pmid23138488">{{cite journal| author=Wei C, Trachtman H, Li J, Dong C, Friedman AL, Gassman JJ et al.| title=Circulating suPAR in two cohorts of primary FSGS. | journal=J Am Soc Nephrol | year= 2012 | volume= 23 | issue= 12 | pages= 2051-9 | pmid=23138488 | doi=10.1681/ASN.2012030302 | pmc=3507361 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23138488 }} </ref>
| |
| ===Role of "Circulating Permeability Factor"===
| |
| The initial insult that causes effacement of foot processes is yet to be discovered. Circulating factors implicated in the [[pathogenesis]] of Primary FSGS include the Soluble Urokinase Plasminogen Activating Receptor (suPAR) and [[MicroRNAs]]. [[MicroRNAs]] are small endogenous (18 to 24 [[nucleotides]] long) noncoding single-stranded RNAs that regulate [[gene expression]] at the post-transcriptional level. Specifically, [[microRNAs]] bind to the messenger RNAs of various genes and lead to their breakdown. <ref name="pmidPMID 25168830">{{cite journal| author=Reiser J, Nast CC, Alachkar N| title=Permeability factors in focal and segmental glomerulosclerosis. | journal=Adv Chronic Kidney Dis | year= 2014 | volume= 21 | issue= 5 | pages= 417-21 | pmid=PMID 25168830 | doi=10.1053/j.ackd.2014.05.010 | pmc=4149759 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25168830 }} </ref>Expression of a specific microRNA called miR-193a produced FSGS in mice but its implication in human podocytopathy has not been clearly defined.
| |
| | |
| suPAR is a heavily glycosylated protein that can be found in several places. It can be present as different fragments and also with various degrees of glycosylation. Both fragmentation and glycosylation of suPAR determine its function and the way it is measured (mainly by ELISA). The most pathogenic form of suPAR for podocytes is still not well defined but there are laboratory evidences of suPAR causing FSGS in lab mice<ref name="pmid23138488">{{cite journal| author=Wei C, Trachtman H, Li J, Dong C, Friedman AL, Gassman JJ et al.| title=Circulating suPAR in two cohorts of primary FSGS. | journal=J Am Soc Nephrol | year= 2012 | volume= 23 | issue= 12 | pages= 2051-9 | pmid=23138488 | doi=10.1681/ASN.2012030302 | pmc=3507361 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23138488 }} </ref> and several cohort studies linking high level of suPAR to FSGS.<ref name="pmid23447064">{{cite journal| author=Huang J, Liu G, Zhang YM, Cui Z, Wang F, Liu XJ et al.| title=Plasma soluble urokinase receptor levels are increased but do not distinguish primary from secondary focal segmental glomerulosclerosis. | journal=Kidney Int | year= 2013 | volume= 84 | issue= 2 | pages= 366-72 | pmid=23447064 | doi=10.1038/ki.2013.55 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23447064 }} </ref>
| |
| | |
| Nonetheless, Shalhoub and colleagues hypothesized in 1974 the involvement of "circulating permeability factor."<ref name="pmid4140273">{{cite journal| author=Shalhoub RJ| title=Pathogenesis of lipoid nephrosis: a disorder of T-cell function. | journal=Lancet | year= 1974 | volume= 2 | issue= 7880 | pages= 556-60 | pmid=4140273 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4140273 }} </ref> In fact, several elements favor the pathological role of "circulating permeability factor" in FSGS:
| |
| *Recurrence of [[proteinuria]] following [[renal transplantation]]<ref name="pmid1994534">{{cite journal| author=Ingulli E, Tejani A| title=Incidence, treatment, and outcome of recurrent focal segmental glomerulosclerosis posttransplantation in 42 allografts in children--a single-center experience. | journal=Transplantation | year= 1991 | volume= 51 | issue= 2 | pages= 401-5 | pmid=1994534 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1994534 }} </ref>
| |
| | |
| *Absence of [[proteinuria]] in patients following [[renal transplantation|transplantation]] in recipients of kidneys from donors with FSGS<ref name="pmid11158426">{{cite journal| author=Rea R, Smith C, Sandhu K, Kwan J, Tomson C| title=Successful transplant of a kidney with focal segmental glomerulosclerosis. | journal=Nephrol Dial Transplant | year= 2001 | volume= 16 | issue= 2 | pages= 416-7 | pmid=11158426 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11158426 }} </ref>
| |
| | |
| *Effectiveness of extracorporeal [[plasmapheresis]] in decreasing the degree of [[proteinuria]]<ref name="pmid11328888">{{cite journal| author=Ghiggeri GM, Artero M, Carraro M, Perfumo F| title=Permeability plasma factors in nephrotic syndrome: more than one factor, more than one inhibitor. | journal=Nephrol Dial Transplant | year= 2001 | volume= 16 | issue= 5 | pages= 882-5 | pmid=11328888 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11328888 }} </ref>
| |
| | |
| *''In vitro'' studies showing permeability alterations by FSGS serum on isolated [[glomeruli]]<ref name="pmid12704575">{{cite journal| author=Savin VJ, McCarthy ET, Sharma M| title=Permeability factors in focal segmental glomerulosclerosis. | journal=Semin Nephrol | year= 2003 | volume= 23 | issue= 2 | pages= 147-60 | pmid=12704575 | doi=10.1053/snep.2003.50024 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12704575 }} </ref>
| |
| | |
| *Transmissibility of glomerular permeability factor from the mother to her infant during [[gestation]]<ref name="pmid11195803">{{cite journal| author=Kemper MJ, Wolf G, Müller-Wiefel DE| title=Transmission of glomerular permeability factor from a mother to her child. | journal=N Engl J Med | year= 2001 | volume= 344 | issue= 5 | pages= 386-7 | pmid=11195803 | doi=10.1056/NEJM200102013440517 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11195803 }} </ref>
| |
| | |
| ===Role of Proteinuria===
| |
| [[Proteinuria]], an important predictor of prognosis, further exacerbates [[renal disease]] by inducing [[tubulointerstitial diseases of the kidney|tubulointerstitial injury]]. [[Proteinuria]] induces the activation of [[immune cells]], such as [[macrophages]] and [[T-cells]], and [[cytokines]], such as tumor growth factor-beta ([[TGF-beta]]), [[interleukin 1|interleukin (IL) 1]], and tumor necrosis factor-alpha ([[TNF-alpha]]).<ref name="pmid11158854">{{cite journal| author=Walls J| title=Relationship between proteinuria and progressive renal disease. | journal=Am J Kidney Dis | year= 2001 | volume= 37 | issue= 1 Suppl 2 | pages= S13-6 | pmid=11158854 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11158854 }} </ref>
| |
| | |
| ===Role of Inflammatory Mediators===
| |
| | |
| The progression of FSGS is highly dependent on the presence of pro-inflammatory cytokines and vasoactive factors that also play a major role in renal fibrosis. Overexpression of tumor growth factor-beta ([[TGF-beta]]), [[platelet-derived growth factor]] (PDGF), and [[vascular endothelial growth factor]] (VEGF) contributes to the progression of disease and is associated with the extent of [[glomerulosclerosis]].<ref name="pmid11423572">{{cite journal| author=Kang DH, Joly AH, Oh SW, Hugo C, Kerjaschki D, Gordon KL et al.| title=Impaired angiogenesis in the remnant kidney model: I. Potential role of vascular endothelial growth factor and thrombospondin-1. | journal=J Am Soc Nephrol | year= 2001 | volume= 12 | issue= 7 | pages= 1434-47 | pmid=11423572 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11423572 }} </ref><ref name="pmid16409155">{{cite journal| author=Harris RC, Neilson EG| title=Toward a unified theory of renal progression. | journal=Annu Rev Med | year= 2006 | volume= 57 | issue= | pages= 365-80 | pmid=16409155 | doi=10.1146/annurev.med.57.121304.131342 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16409155 }} </ref> Activated [[cytokines]] promote cellular infiltration and desposition of [[collagen]] along the mesangial matrix.<ref name="pmid16409155">{{cite journal| author=Harris RC, Neilson EG| title=Toward a unified theory of renal progression. | journal=Annu Rev Med | year= 2006 | volume= 57 | issue= | pages= 365-80 | pmid=16409155 | doi=10.1146/annurev.med.57.121304.131342 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16409155 }} </ref>
| |
| | |
| ===Maladaptive Interactions===
| |
| | |
| Following the loss of [[podocytes]], maladaptive interactions occur between the [[glomerular basement membrane|GBM]] and the renal epithelial cells, leading to proliferation of epithelial, endothelial, and mesangial cells.<ref name="pmid12704576">{{cite journal| author=Fogo AB| title=Animal models of FSGS: lessons for pathogenesis and treatment. | journal=Semin Nephrol | year= 2003 | volume= 23 | issue= 2 | pages= 161-71 | pmid=12704576 | doi=10.1053/snep.2003.50015 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12704576 }}</ref> The resultant collagen deposition then contributes to the scarring of the glomerular tufts that appear as focal and segmental regions of glomerulosclerosis as seen on pathology. The diseased regions then progress to involve larger areas of the kidneys and eventually become diffusely sclerotic, causing end-stage renal disease (ESRD).<ref name="pmid12704576"></ref>
| |
| | |
| ===Role of Mechanical Stresses===
| |
| Defects of the [[glomerular filtration]] barrier leads to an overwhelmingly increased single nephron [[glomerular filtration rate]] (SNGFR). This [[mechanical stress]] helps in the progression of FSGS by creating a state of hypertrophy that worsens the lack of balance between the GBM and the podocytopenia, and thus worsens the extent of injury.<ref name="pmid18039119">{{cite journal| author=Kwoh C, Shannon MB, Miner JH, Shaw A| title=Pathogenesis of nonimmune glomerulopathies. | journal=Annu Rev Pathol | year= 2006 | volume= 1 | issue= | pages= 349-74 | pmid=18039119 | doi=10.1146/annurev.pathol.1.110304.100119 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18039119 }} </ref><ref name="pmid12704579">{{cite journal| author=Hostetter TH| title=Hyperfiltration and glomerulosclerosis. | journal=Semin Nephrol | year= 2003 | volume= 23 | issue= 2 | pages= 194-9 | pmid=12704579 | doi=10.1053/anep.2003.50017 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12704579 }} </ref>
| |
| | |
| ===Role of Genetics===
| |
| There are currently several mutations in cytoskeletal and membrane proteins that lead to familial FSGS:
| |
| *''Nephrin'' gene in congenital Finnish-type nephrotic syndrome - ''NPHS1''<ref name="pmid9660941">{{cite journal| author=Kestilä M, Lenkkeri U, Männikkö M, Lamerdin J, McCready P, Putaala H et al.| title=Positionally cloned gene for a novel glomerular protein--nephrin--is mutated in congenital nephrotic syndrome. | journal=Mol Cell | year= 1998 | volume= 1 | issue= 4 | pages= 575-82 | pmid=9660941 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9660941 }} </ref><ref name="pmid18039119">{{cite journal| author=Kwoh C, Shannon MB, Miner JH, Shaw A| title=Pathogenesis of nonimmune glomerulopathies. | journal=Annu Rev Pathol | year= 2006 | volume= 1 | issue= | pages= 349-74 | pmid=18039119 | doi=10.1146/annurev.pathol.1.110304.100119 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18039119 }} </ref>
| |
| *''Nephrin-like transmembrane'' gene - ''NEPH1''<ref name="pmid14712353">{{cite journal| author=Asanuma K, Mundel P| title=The role of podocytes in glomerular pathobiology. | journal=Clin Exp Nephrol | year= 2003 | volume= 7 | issue= 4 | pages= 255-9 | pmid=14712353 | doi=10.1007/s10157-003-0259-6 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14712353 }} </ref>
| |
| *''Podocin'' gene - ''NPHS2''<ref name="pmid16571882">{{cite journal| author=Tryggvason K, Patrakka J, Wartiovaara J| title=Hereditary proteinuria syndromes and mechanisms of proteinuria. | journal=N Engl J Med | year= 2006 | volume= 354 | issue= 13 | pages= 1387-401 | pmid=16571882 | doi=10.1056/NEJMra052131 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16571882 }} </ref>
| |
| *CD2-associated protein (CD2AP)<ref name="pmid10514378">{{cite journal| author=Shih NY, Li J, Karpitskii V, Nguyen A, Dustin ML, Kanagawa O et al.| title=Congenital nephrotic syndrome in mice lacking CD2-associated protein. | journal=Science | year= 1999 | volume= 286 | issue= 5438 | pages= 312-5 | pmid=10514378 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10514378 }} </ref><ref name="pmid12764198">{{cite journal| author=Kim JM, Wu H, Green G, Winkler CA, Kopp JB, Miner JH et al.| title=CD2-associated protein haploinsufficiency is linked to glomerular disease susceptibility. | journal=Science | year= 2003 | volume= 300 | issue= 5623 | pages= 1298-300 | pmid=12764198 | doi=10.1126/science.1081068 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12764198 }} </ref>
| |
| *''Alpha-actinin-4'' gene <ref name="pmid10700177">{{cite journal| author=Kaplan JM, Kim SH, North KN, Rennke H, Correia LA, Tong HQ et al.| title=Mutations in ACTN4, encoding alpha-actinin-4, cause familial focal segmental glomerulosclerosis. | journal=Nat Genet | year= 2000 | volume= 24 | issue= 3 | pages= 251-6 | pmid=10700177 | doi=10.1038/73456 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10700177 }} </ref>
| |
| *Transient receptor potential cation channel - TRPC6<ref name="pmid12953036">{{cite journal| author=Winn MP| title=Approach to the evaluation of heritable diseases and update on familial focal segmental glomerulosclerosis. | journal=Nephrol Dial Transplant | year= 2003 | volume= 18 Suppl 6 | issue= | pages= vi14-20 | pmid=12953036 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12953036 }} </ref>
| |
| *Mutation in ''wilms tumor'' gene - ''WT1''<ref name="pmid23871408">{{cite journal| author=Beck L, Bomback AS, Choi MJ, Holzman LB, Langford C, Mariani LH et al.| title=KDOQI US commentary on the 2012 KDIGO clinical practice guideline for glomerulonephritis. | journal=Am J Kidney Dis | year= 2013 | volume= 62 | issue= 3 | pages= 403-41 | pmid=23871408 | doi=10.1053/j.ajkd.2013.06.002 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23871408 }} </ref>
| |
| | |
| *Mutation in ''SCARB2 (LIMP2)'' gene<ref name="pmid23871408">{{cite journal| author=Beck L, Bomback AS, Choi MJ, Holzman LB, Langford C, Mariani LH et al.| title=KDOQI US commentary on the 2012 KDIGO clinical practice guideline for glomerulonephritis. | journal=Am J Kidney Dis | year= 2013 | volume= 62 | issue= 3 | pages= 403-41 | pmid=23871408 | doi=10.1053/j.ajkd.2013.06.002 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23871408 }} </ref>
| |
| | |
| *Mutation in ''formin'' gene - ''INF2''<ref name="pmid23871408">{{cite journal| author=Beck L, Bomback AS, Choi MJ, Holzman LB, Langford C, Mariani LH et al.| title=KDOQI US commentary on the 2012 KDIGO clinical practice guideline for glomerulonephritis. | journal=Am J Kidney Dis | year= 2013 | volume= 62 | issue= 3 | pages= 403-41 | pmid=23871408 | doi=10.1053/j.ajkd.2013.06.002 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23871408 }} </ref>
| |
| | |
| *Mitochondrial cytopathies<ref name="pmid23871408">{{cite journal| author=Beck L, Bomback AS, Choi MJ, Holzman LB, Langford C, Mariani LH et al.| title=KDOQI US commentary on the 2012 KDIGO clinical practice guideline for glomerulonephritis. | journal=Am J Kidney Dis | year= 2013 | volume= 62 | issue= 3 | pages= 403-41 | pmid=23871408 | doi=10.1053/j.ajkd.2013.06.002 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23871408 }} </ref>
| |
| | |
| ==References==
| |
| {{Reflist|2}}
| |
| | |
| | |
| {{WH}}
| |
| {{WS}}
| |