Uremic pericarditis pathophysiology
|
Uremic pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Uremic pericarditis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Uremic pericarditis pathophysiology |
|
Risk calculators and risk factors for Uremic pericarditis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Varun Kumar, M.B.B.S.; Lakshmi Gopalakrishnan, M.B.B.S.
Overview
The pathophysiology of uremic pericarditis is not fully understood. However, there is a correlation observed with levels of blood urea nitrogen(usually >60 mg/dL) and creatinine. In renal failure, the absence or inadequate dialysis can lead to accumulation of these toxins in the body which may cause inflammation of pericardium and development of adhesions between the two pericardial layers. This could lead to loculation of effusion in pericardial cavity. Patients undergoing dialysis may also develop pericarditis. In a series, 13% of patients undergoing hemodialysis developed pericarditis.
Pathophysiology
- The pathophysiology of uremic pericarditis is not fully understood. However, there is a correlation observed with levels of blood urea nitrogen(usually >60 mg/dL) and creatinine.
- In renal failure, the absence or inadequate dialysis can lead to accumulation of these toxins in the body which may cause inflammation of pericardium and development of adhesions between the two pericardial layers. This could lead to loculation of effusion in pericardial cavity.
- Patients undergoing dialysis may also develop pericarditis. In a series, 13% of patients undergoing hemodialysis developed pericarditis[1]
- Uremic pericarditis can occur as a serous or a hemorrhagic effusion with considerable overlapping. Hemorrhagic effusions are more common secondary to uremia induced platelet dysfunction and the use of anticoagulation during hemodialysis.
- Dialysis associated pericarditis may also be secondary to volume overload and bacterial or viral infections.[2]
- Presence of a large pericardial effusion that persists for >10 days after intensive dialysis has a high likelihood of development of cardiac tamponade.
Gross Pathology
-
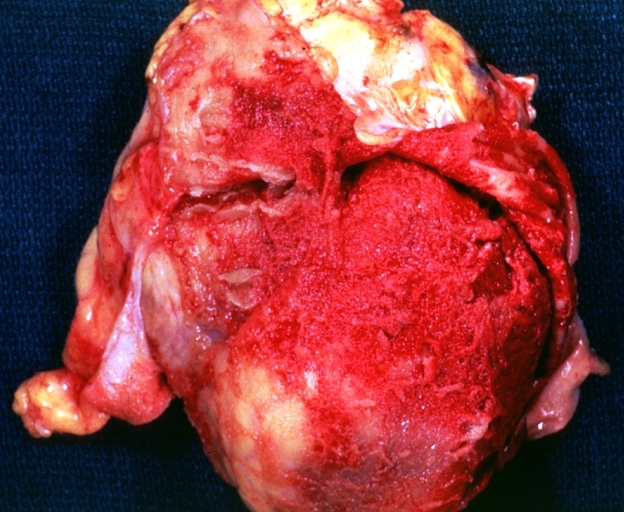
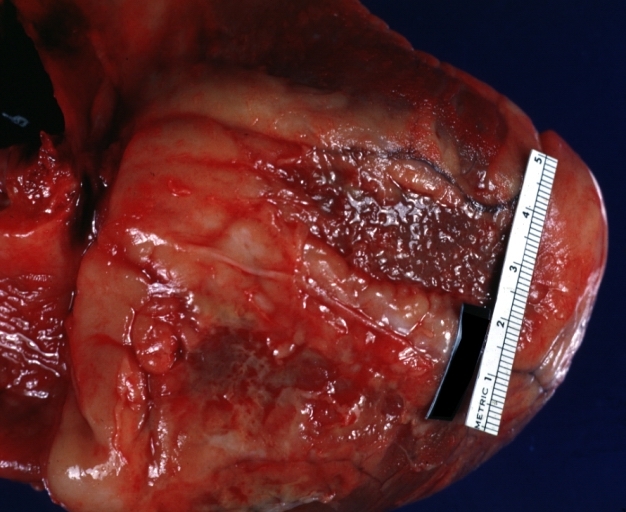
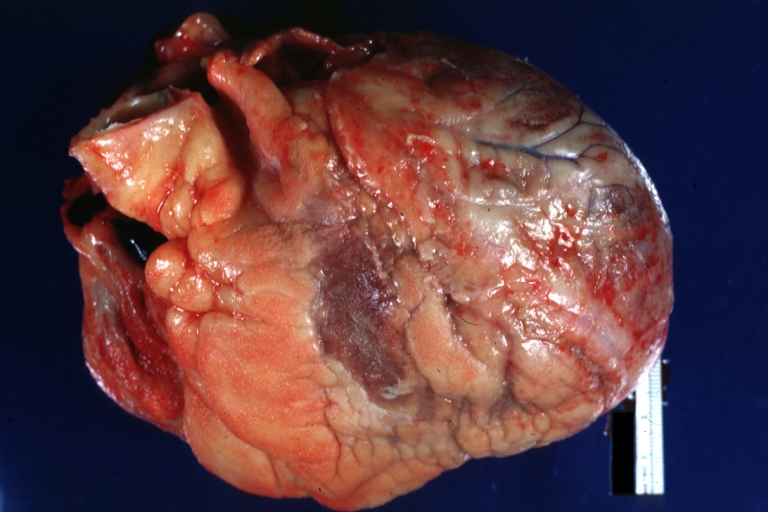
Pericarditis in uremia
-
Fibrinous pericarditis: Gross, natural color, an excellent example of bread and butter appearance. Uremia, chronic glomerulonephritis and sepsis.
-
Fibrinous pericarditis: Gross, natural color, close-up view of minimal fibrinous exudate on epicardial surface due to terminal renal failure
-
Fibrinous pericarditis: Gross, natural color, anterior view of heart with mild fibrinous exudate over epicardium due to terminal renal failure
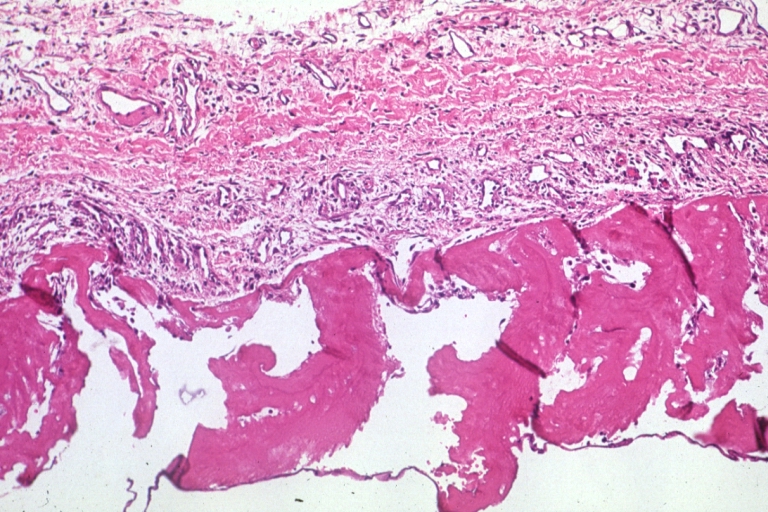
Microscopic Pathology
References
- ↑ Rutsky EA, Rostand SG (1987). "Treatment of uremic pericarditis and pericardial effusion". Am J Kidney Dis. 10 (1): 2–8. PMID 3605080.
- ↑ Gunukula SR, Spodick DH (2001). "Pericardial disease in renal patients". Semin Nephrol. 21 (1): 52–6. PMID 11172559.