Uremic pericarditis: Difference between revisions
No edit summary |
Varun Kumar (talk | contribs) No edit summary |
||
| Line 16: | Line 16: | ||
==Pathophysiology== | ==Pathophysiology== | ||
The pathophysiology of uremic pericarditis is not fully understood. However, there is a correlation observed with levels of [[blood urea nitrogen]](usually >60 mg/dL) and [[creatinine]]. In [[renal failure]], the absence or inadequate [[dialysis]] can lead to accumulation of these toxins in the body which may cause inflammation of [[pericardium]] and development of adhesions between the two pericardial layers. | The pathophysiology of uremic pericarditis is not fully understood. However, there is a correlation observed with levels of [[blood urea nitrogen]](usually >60 mg/dL) and [[creatinine]]. In [[renal failure]], the absence or inadequate [[dialysis]] can lead to accumulation of these toxins in the body which may cause inflammation of [[pericardium]] and development of adhesions between the two pericardial layers. This could lead to loculation of effusion in pericardial cavity. | ||
Patients undergoing dialysis may also develop [[pericarditis]]. In a series, 13% of patients undergoing hemodialysis developed pericarditis<ref name="pmid3605080">{{cite journal| author=Rutsky EA, Rostand SG| title=Treatment of uremic pericarditis and pericardial effusion. | journal=Am J Kidney Dis | year= 1987 | volume= 10 | issue= 1 | pages= 2-8 | pmid=3605080 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3605080 }} </ref> | Patients undergoing dialysis may also develop [[pericarditis]]. In a series, 13% of patients undergoing hemodialysis developed pericarditis<ref name="pmid3605080">{{cite journal| author=Rutsky EA, Rostand SG| title=Treatment of uremic pericarditis and pericardial effusion. | journal=Am J Kidney Dis | year= 1987 | volume= 10 | issue= 1 | pages= 2-8 | pmid=3605080 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3605080 }} </ref> | ||
| Line 26: | Line 26: | ||
Presence of a large pericardial effusion that persists for >10 days after intensive dialysis has a high likelihood of development of [[cardiac tamponade]] | Presence of a large pericardial effusion that persists for >10 days after intensive dialysis has a high likelihood of development of [[cardiac tamponade]] | ||
==History and symptoms== | ==Diagnosis== | ||
===History and symptoms=== | |||
Patients may present with the following symptoms: | Patients may present with the following symptoms: | ||
*[[Fever]] | *[[Fever]] | ||
| Line 35: | Line 36: | ||
*[[Ankle edema]] | *[[Ankle edema]] | ||
==Physical examination== | Patients with uremic pericarditis may also present without any symptoms<ref name="pmid16805885">{{cite journal| author=Banerjee A, Davenport A| title=Changing patterns of pericardial disease in patients with end-stage renal disease. | journal=Hemodial Int | year= 2006 | volume= 10 | issue= 3 | pages= 249-55 | pmid=16805885 | doi=10.1111/j.1542-4758.2006.00104.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16805885 }} </ref>. | ||
===Physical examination=== | |||
Patients may present with [[fever]], [[cachexia]] and varying levels of [[consciousness]]. | Patients may present with [[fever]], [[cachexia]] and varying levels of [[consciousness]]. | ||
| Line 47: | Line 51: | ||
'''Extremities:''' [[Ankle edema]] | '''Extremities:''' [[Ankle edema]] | ||
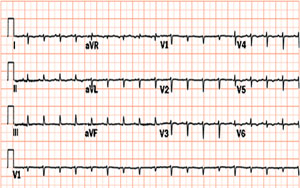
===Electrocardiogram=== | |||
Typical [[ECG]] changes of acute pericarditis such as ST and T wave elevations may not be seen in uremic pericarditis. This could be due to non-involvement of myocardium<ref name="pmid11172559">{{cite journal| author=Gunukula SR, Spodick DH| title=Pericardial disease in renal patients. | journal=Semin Nephrol | year= 2001 | volume= 21 | issue= 1 | pages= 52-6 | pmid=11172559 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11172559 }} </ref>. | |||
However, [[electrical alternans]] may be seen in presence of [[cardiac tamponade]] and other [[ECG]] changes related to [[electrolyte]]s abnormalities due to poor renal function may be noted. | |||
[[Image:Tamponade-with-alternans.jpg|thumb|left|400px|Electrical alternans]] | |||
<br clear="left"/> | |||
===Chest X ray=== | |||
Enlargement of cardiac shadow related to myocardial dysfunction, volume overload, or [[pericardial effusion]] may be observed on chest x-ray. | |||
[[Image:Pericardial effusion 4.jpg|thumb|400px|left|Pericardial effusion]] | |||
<br clear="left"/> | |||
===Echocardiography=== | |||
Echocardiogram may show presence of fluid surrounding the heart in pericardial effusion. Loculated effusions secondary to adhesions in pericardial cavity may also be visualized as shown in the video below. | |||
Swinging motion of the heart may be seen in patients with [[cardiac tamponade]]. | |||
'''Echocardiography of heart with loculated pericardial effusion compressing the left ventricle''' | |||
<youtube v=unnmmlCyyZM/> | |||
===Cardiac catheterization=== | |||
In presence '''Cardiac tamponade''', there is equalization of pressures in all four chambers of heart. The right atrial pressure equals the right ventricular end diastolic pressure equals the pulmonary artery diastolic pressure. | |||
==References== | ==References== | ||
Revision as of 20:50, 29 June 2011
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Uremic pericarditis On the Web |
|
American Roentgen Ray Society Images of Uremic pericarditis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Varun Kumar, M.B.B.S.
Overview
Renal failure can be associated with the development of a pericardial effusion and pericarditis, a condition known as uremic pericarditis. The underlying pathophysiology is not entirely clear, but it is hypothesized that uremic pericarditis is due to a build up of metabolic toxins such as urea, creatinine, methylguanidine which cause inflammation of pericardium. With the introduction of dialysis, the incidence of uremic pericarditis has dropped[1]. Uremic pericaritis can be further divided as:
- Uremic pericarditis in patients not undergoing dialysis.
- Uremic pericarditis in patients on maintenance dialysis.
Etiology
- Absence of dialysis in renal failure
- Inadequate dialysis in renal failure
- Volume overload during dialysis
- Infections
Pathophysiology
The pathophysiology of uremic pericarditis is not fully understood. However, there is a correlation observed with levels of blood urea nitrogen(usually >60 mg/dL) and creatinine. In renal failure, the absence or inadequate dialysis can lead to accumulation of these toxins in the body which may cause inflammation of pericardium and development of adhesions between the two pericardial layers. This could lead to loculation of effusion in pericardial cavity.
Patients undergoing dialysis may also develop pericarditis. In a series, 13% of patients undergoing hemodialysis developed pericarditis[2]
Uremic pericarditis can occur as a serous or a hemorrhagic effusion with considerable overlapping. Hemorrhagic effusions are more common secondary to uremia induced platelet dysfunction and the use of anticoagulation during hemodialysis.
Dialysis associated pericarditis may also be secondary to volume overload and bacterial or viral infections[3].
Presence of a large pericardial effusion that persists for >10 days after intensive dialysis has a high likelihood of development of cardiac tamponade
Diagnosis
History and symptoms
Patients may present with the following symptoms:
- Fever
- Chest pain that improves on leaning forward and worsens on inspiration
- Breathlessness
- Dizziness
- Malaise
- Ankle edema
Patients with uremic pericarditis may also present without any symptoms[4].
Physical examination
Patients may present with fever, cachexia and varying levels of consciousness.
Vitals: Hypotensionand pulsus paradoxus are present in cardiac tamponade. The heart rate may be slow due to autonomic impairment or an arrhythmia such as atrial fibrillation, atrial flutter, heart block or a ventricular arrhythmia may be present due to an electrolyte imbalance.
Neck: Jugular venous distension with a prominent Y descent and Kussmaul's sign
Chest: Ewart's sign may be present. This includes a pericardial knock, pericardial rub(heard best while leaning forwards) and distant heart sounds
Abdomen: Hepatomegaly, ascites
Extremities: Ankle edema
Electrocardiogram
Typical ECG changes of acute pericarditis such as ST and T wave elevations may not be seen in uremic pericarditis. This could be due to non-involvement of myocardium[3].
However, electrical alternans may be seen in presence of cardiac tamponade and other ECG changes related to electrolytes abnormalities due to poor renal function may be noted.
Chest X ray
Enlargement of cardiac shadow related to myocardial dysfunction, volume overload, or pericardial effusion may be observed on chest x-ray.

Echocardiography
Echocardiogram may show presence of fluid surrounding the heart in pericardial effusion. Loculated effusions secondary to adhesions in pericardial cavity may also be visualized as shown in the video below. Swinging motion of the heart may be seen in patients with cardiac tamponade.
Echocardiography of heart with loculated pericardial effusion compressing the left ventricle <youtube v=unnmmlCyyZM/>
Cardiac catheterization
In presence Cardiac tamponade, there is equalization of pressures in all four chambers of heart. The right atrial pressure equals the right ventricular end diastolic pressure equals the pulmonary artery diastolic pressure.
References
- ↑ Bailey GL, Hampers CL, Hager EB, Merrill JP (1968). "Uremic pericarditis. Clinical features and management". Circulation. 38 (3): 582–91. PMID 5673609.
- ↑ Rutsky EA, Rostand SG (1987). "Treatment of uremic pericarditis and pericardial effusion". Am J Kidney Dis. 10 (1): 2–8. PMID 3605080.
- ↑ 3.0 3.1 Gunukula SR, Spodick DH (2001). "Pericardial disease in renal patients". Semin Nephrol. 21 (1): 52–6. PMID 11172559.
- ↑ Banerjee A, Davenport A (2006). "Changing patterns of pericardial disease in patients with end-stage renal disease". Hemodial Int. 10 (3): 249–55. doi:10.1111/j.1542-4758.2006.00104.x. PMID 16805885.