|
|
| (15 intermediate revisions by 7 users not shown) |
| Line 1: |
Line 1: |
| __NOTOC__ | | __NOTOC__ |
| | {| class="infobox" style="float:right;" |
| | |- |
| | | <figure-inline>[[File:Siren.gif|link=Upper gastrointestinal bleeding resident survival guide|41x41px]]</figure-inline>|| <br> || <br> |
| | | [[Upper gastrointestinal bleeding resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] |
| | |} |
| | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' |
| | |
| {{Infobox_Disease | | | {{Infobox_Disease | |
| Name = {{PAGENAME}} | | | Name = {{PAGENAME}} | |
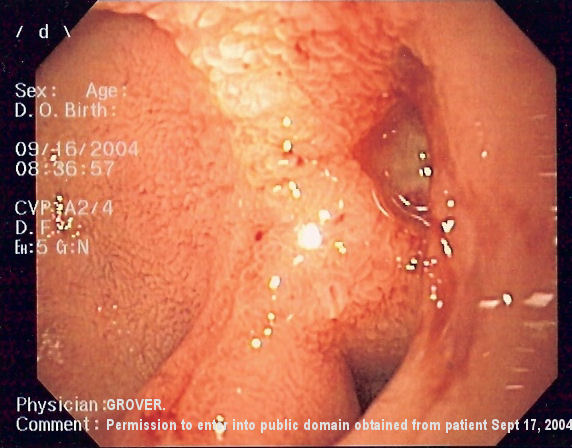
| Image = DU 2.jpg | | | Image = DU 2.jpg | |
| Caption = Endoscopic image of a posterior wall [[ulcer|duodenal ulcer]] with a clean base, which is a common cause of '''upper GI hemorrhage'''. | | | Caption = Endoscopic image of a posterior wall [[ulcer|duodenal ulcer]] with a clean base, which is a common cause of '''upper GI hemorrhage'''. | |
| DiseasesDB = |
| |
| ICD10 = {{ICD10|K|92|2|k|90}} |
| |
| ICD9 = {{ICD9|578.9}} |
| |
| ICDO = |
| |
| OMIM = |
| |
| MedlinePlus = |
| |
| eMedicineSubj = med |
| |
| eMedicineTopic = 3565 |
| |
| MeshID = |
| |
| }} | | }} |
| {{Search infobox}}
| |
| {{CMG}}
| |
| ==Overview==
| |
| '''Upper gastrointestinal (GI) bleeding''' refers to [[hemorrhage]] in the [[upper gastrointestinal tract]]. The anatomic cut-off for upper GI bleeding is the [[ligament of Treitz]], which connects the fourth portion of the [[duodenum]] to the [[Thoracic diaphragm|diaphragm]] near the [[splenic flexure]] of the [[colon (anatomy)|colon]].
| |
|
| |
|
| Upper GI bleeds are considered [[medical emergencies]], and require admission to [[hospital]] for urgent diagnosis and management. Due to advances in [[proton pump inhibitors|medications]] and [[endoscopy]], upper GI hemorrhage is now usually treated without surgery. | | {{Upper gastrointestinal bleeding}} |
|
| |
|
| ==Clinical presentation==
| | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} ; {{ADG}} |
| Patients with upper GI hemorrhage often present with [[hematemesis]], [[coffee ground vomiting]], [[melena]], maroon stool, or [[hematochezia]] if the hemorrhage is severe. The presentation of bleeding depends on the amount and location of hemorrhage.
| |
|
| |
|
| Patients may also present with complications of [[anemia]], including chest pain, [[syncope]], [[fatigue (physical)|fatigue]] and shortness of breath.
| | {{SK}} Gastrointestinal bleeding, Gastric bleeding, Esophageal bleeding, Esophageal tears, Bleeding vomit, Upper GI bleeding. |
|
| |
|
| The [[physical examination]] performed by the [[physician]] concentrates on the following things:
| | ==[[Upper gastrointestinal bleeding overview|Overview]]== |
| *[[Vital signs]], in order to determine the severity of bleeding and the timing of intervention
| |
| *[[Abdomen|Abdominal]] and [[rectum|rectal]] examination, in order to determine possible causes of hemorrhage
| |
| *Assessment for [[portal hypertension]] and [[cirrhosis|stigmata of chronic liver disease]] in order to determine if the bleeding is from a variceal source.
| |
|
| |
|
| Laboratory findings include [[anemia]], [[coagulopathy]], and an elevated [[BUN-to-creatinine ratio]].
| | ==[[Upper gastrointestinal bleeding historical perspective|Historical Perspective]]== |
|
| |
|
| ==Causes== | | ==[[Upper gastrointestinal bleeding classification|Classification]]== |
| There are many causes for upper GI hemorrhage. Causes are usually anatomically divided into their location in the upper gastrointestinal tract.
| |
|
| |
|
| Patients are usually stratified into having either '''[[esophageal varices|variceal]]''' or '''non-variceal''' sources of upper GI hemorrhage, as the two have different treatment algorithms and prognosis.
| | ==[[Upper gastrointestinal bleeding pathophysiology|Pathophysiology]]== |
|
| |
|
| The causes for upper GI hemorrhage include the following:
| | ==[[Upper gastrointestinal bleeding causes|Causes]]== |
| *[[Esophagus|Esophageal]] causes:
| |
| ** [[Esophageal varices]]
| |
| ** [[Esophagitis]]
| |
| ** [[Esophageal cancer]]
| |
| **Esophageal ulcers
| |
|
| |
|
| *[[Stomach|Gastric]] causes:
| | ==[[Upper gastrointestinal bleeding differential diagnosis|Differentiating Upper Gastrointestinal Bleeding from other Diseases]]== |
| ** [[Gastric ulcer]]
| |
| ** [[Gastric cancer]]
| |
| ** [[Gastritis]]
| |
| ** [[Gastric varices]]
| |
| ** [[Gastric antral vascular ectasia]], or watermelon stomach
| |
| ** [[Dieulafoy's lesion]]s
| |
|
| |
|
| *[[Duodenum|Duodenal]] causes:
| | ==[[Upper gastrointestinal bleeding epidemiology and demographics|Epidemiology and Demographics]]== |
| **[[Duodenal ulcer]]
| |
| ** Vascular malformations, including aorto-enteric fistulae. Fistulae are usually secondary to prior vascular surgery and usually occur at the proximal anastomosis at the third or fourth portion of the duodenum where it is retroperitoneal and near the aorta.<ref name="pmidpending">{{cite journal |author=Graber CJ et al |title=A Stitch in Time — A 64-year-old man with a history of coronary artery disease and peripheral vascular disease was admitted to the hospital with a several-month history of fevers, chills, and fatigue |journal=New Engl J Med |volume=357 |issue= |pages=1029-1034 |year=2007 |pmid= |doi=|url=http://content.nejm.org/cgi/content/full/357/10/1029}}</ref><ref name="pmid12704326">{{cite journal |author=Sierra J, Kalangos A, Faidutti B, Christenson JT |title=Aorto-enteric fistula is a serious complication to aortic surgery. Modern trends in diagnosis and therapy |journal=Cardiovascular surgery (London, England) |volume=11 |issue=3 |pages=185-8 |year=2003 |pmid=12704326 |doi=}}</ref><ref name="pmid15279179">{{cite journal |author=Cendan JC, Thomas JB, Seeger JM |title=Twenty-one cases of aortoenteric fistula: lessons for the general surgeon |journal=The American surgeon |volume=70 |issue=7 |pages=583-7; discussion 587 |year=2004 |pmid=15279179 |doi=}}</ref>
| |
| ** Hematobilia, or bleeding from the biliary tree
| |
| **[[Hemosuccus pancreaticus]], or bleeding from the [[pancreatic duct]]
| |
|
| |
|
| ==Diagnosis== | | ==[[Upper gastrointestinal bleeding risk factors|Risk Factors]]== |
| ===Summary===
| |
| The diagnosis of upper GI bleeding is assumed when hematemesis is documented. In the absence of hematemesis, an upper source for GI bleeding is likely in the presence of at least two factors among: black stool, age < 50 years, and blood urea nitrogen/creatinine ratio 30 or more. In the absence of these findings, consider a nasogastric aspirate to determine the source of bleeding. If the aspirate is positive, an upper GI bleed is greater than 50%, but not high enough to be certain. If the aspirate is negative, the source of a GI bleed is likely lower. The accuracy of the aspirate is improved by using the Gastroccult test.
| |
|
| |
|
| <div align="center">
| | ==[[Upper gastrointestinal bleeding screening|Screening]]== |
| <gallery heights="175" widths="175">
| |
| Image:MALT 4.jpg|'''Gastric ulcer''' in [[antrum]] of [[stomach]] with overlying clot. Pathology was consistent with [[gastric lymphoma]]. Reproduced with permission of patient]]
| |
| Image:Gastric ulcer 2.jpg|[[Esophagogastroduodenoscopy|Endoscopic]] image of small [[gastric ulcer]] with visible vessel]]
| |
| Image:GU with clip.jpg|Same ulcer seen after endoscopic clipping]]
| |
| </gallery>
| |
| </div>
| |
|
| |
|
| ===Details=== | | ==[[Upper gastrointestinal bleeding natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| ====Prevalence of upper GI bleeding====
| |
| About 75% of patients presenting to the emergency room with GI bleeding have an upper source {{ref|1}}. The diagnosis is easier when the patient has hematemesis. In the absence of hematemesis, 40% to 50% of patients in the emergency room with GI bleeding have an upper source{{ref|2}} {{ref|3}} {{ref|4}}. Determining whether a patient truly has an upper GI bleed versus [[lower gastrointestinal bleeding]] is difficult.
| |
|
| |
|
| ====Diagnostic testing==== | | ==Diagnosis== |
| Whiting studied a cohort of 325 patients and found the odds ratios for the strongest predictors were: black stool, 16.6 (95% confidence interval [CI], 7.7-35.7); age < 50 years, 8.4 (95% CI, 3.2-22.1); and blood urea nitrogen/creatinine ratio 30 or more, 10.0 (95% CI, 4.0-25.6){{ref|2}} . Seven (5%) of 151 with none of these factors had an upper GI tract bleed, versus 63 (93%) of 68 with 2 or 3 factors. Ernst found similar results{{ref|1}}.
| |
| | |
| The nasogastric aspirate can help determine the location of bleeding and thus direct initial diagnostic and treatment plans. Witting found that nasogastric aspirate has sensitivity 42%, specificity 91%, [[negative predictive value]] 64%, positive predictive value 92% and overall accuracy of 66% in differentiating upper GI bleeding from bleeding distal to the [[ligament of Treitz]]{{ref|3}}. Thus, in this study a positive aspirate is more helpful than a negative aspirate. In a smaller study, Cuellar found a sensitivity of 79% and specificity of 55%{{ref|4}}, somewhat opposite results from Witting. Cuellar also studied the appearance of the aspirate and a [http://www.eboncall.org/CATs/2190.html summary of these results] is available at the Evidence-Based On-Call database. Although the website lists these results as expired, they were available as of Oct, 16, 2006. These results are also available through the [http://web.archive.org/web/*/http://www.eboncall.org/CATs/2190.html Wayback Archive] and readers may consult the Archive if the original page is removed.
| |
| | |
| Determining whether blood is in gastric contents, either vomited or aspirated specimens, is surprisingly difficult. Slide tests are based on orthotolidine (Hematest reagent tablets and Bili-Labstix) or guaiac (Hemoccult and Gastroccult). Rosenthal found orthotolidine-based tests more sensitive than specific; the Hemoccult test's sensitivity reduced by the acidic environment; and the Gastroccult test be the most accurate{{ref|5}}. Cuellar found the following results:
| |
| | |
| {| class="wikitable" style="text-align:center"
| |
| |+ Determining whether blood is in the gastric aspirate{{ref|4}}
| |
| ! Finding !! Sensitivity !! Specificity !! Positive predictive value<br>(prevalence of 39%)!! Negative predictive value<br>(prevalence of 39%)
| |
| |-
| |
| ! Gastroccult
| |
| | 95% || 82% || 77% || 96%
| |
| |-
| |
| ! Physician assessment
| |
| | 79% || 55% || 53% || 20%
| |
| |}
| |
| | |
| Holman used simulated gastric specimens and found the Hemoccult test to have significant problems with non-specificy and false-positive results, whereas the Gastroccult test was very accurate{{ref|6}}. Holman found that by 120 seconds after the developer was applied, the Hemoccult test was positive on ''all'' control samples.
| |
| | |
| ====A note on Bayesian calculations====
| |
| The predictive values cited are based on the prevalences of upper GI bleeding in the corresponding studies. A [http://medinformatics.uthscsa.edu/calculator/ clinical calculator] can be used to generate predictive values for other prevalences such as those listed above under '''Prevalences'''.
| |
| | |
| == Treatment ==
| |
| | |
| Emergency treatment for upper GI bleeds includes aggressive replacement of volume with [[intravenous]] solutions, and [[blood]] products if required. As patients with [[esophageal varices]] typically have coagulopathy, [[fresh frozen plasma|plasma]] products may have to be administered. Vitals signs are continuously monitored.
| |
| | |
| Early [[esophagogastroduodenoscopy|endoscopy]] is recommended, both as a diagnostic and therapeutic approach, as endoscopic treatment can be performed through the endoscope. Therapy depends on the lesion identifies, and can include:
| |
|
| |
|
| *[[Injection (medicine)|injection]] of [[adrenaline]] or other [[sclerotherapy]]
| | [[Upper gastrointestinal bleeding diagnostic criteria|Diagnostic Criteria]] | [[Upper gastrointestinal bleeding history and symptoms|History and Symptoms]] | [[Upper gastrointestinal bleeding physical examination|Physical Examination]] | [[Upper gastrointestinal bleeding laboratory findings|Laboratory Findings]] | [[Upper gastrointestinal bleeding other diagnostic studies|Other Diagnostic Studies]] |
| *electrocautery
| |
| *endoscopic clipping
| |
| *or banding of [[esophageal varices|varices]]
| |
|
| |
|
| Stigmata of high risk include active bleeding, oozing, visible vessels and red spots. Clots that are present on the bleeding lesion are usually removed in order to determine the underlying pathology, and to determine the risk for rebleeding.
| | ==Treatment== |
| | [[Upper gastrointestinal bleeding medical therapy|Medical Therapy]] | [[Upper gastrointestinal bleeding surgery|Surgery]] | [[Upper gastrointestinal bleeding primary prevention|Primary Prevention]] | [[Upper gastrointestinal bleeding secondary prevention|Secondary Prevention]] | [[Upper gastrointestinal bleeding cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Upper gastrointestinal bleeding future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| | ==Case Studies== |
| | [[Upper gastrointestinal bleeding case study one|Case #1]] |
|
| |
|
| Pharmacotherapy includes the following:
| | ==Related Chapter== |
| * [[Proton pump inhibitors]] (PPIs), which reduce [[gastric acid]] production and accelerate healing of certain gastric, duodenal and esophageal sources of hemorrhage. These can be administered orally or intravenously as an infusion depending on the risk of rebleeding.
| |
| * [[Octreotide]] is a [[somatostatin]] analog believed to shunt blood away from the splanchnic circulation. It has found to be a useful adjunct in management of both variceal and non-variceal upper GI hemorrhage. It is the somatostatin analog most commonly used in North America.
| |
| * [[Terlipressin]] is a [[somatostatin]] analog most commonly used in Europe for variceal upper GI hemorrhage.
| |
| * Antibiotics are prescribed in upper GI bleeds associated with [[portal hypertension]]
| |
| | |
| If ''[[Helicobacter pylori]]'' is identified as a contributant to the source of hemorrhage, then therapy with antibiotics and a PPI is suggested.
| |
| | |
| ==Refractory bleeding== | |
| | |
| Refractory cases of upper GI hemorrhage may require:
| |
| * Repeat [[endoscopy|esophagogastroduodenoscopy]]
| |
| * Anti-fibrinolytics, such as [[tranexamic acid]]
| |
| * [[Angiography]] to identify and possibly occlude the feeder vessel
| |
| * Recombinant [[Factor VII]] is sometimes used as an adjunct in refractory bleeding, but its utility has only been tested for variceal hemorrhage
| |
| * [[Balloon tamponade]]
| |
| * [[Surgery]], to oversew or remove the area of hemorrhage
| |
| | |
| Certain causes of upper GI hemorrhage (including [[gastric ulcer]]s require repeat [[endoscopy]] after the episode of bleeding to ascertain healing of the causative lesion.
| |
| | |
| ==References==
| |
| {{Reflist}}
| |
| *{{note|1}} Ernst AA, Haynes ML, Nick TG, Weiss SJ. Usefulness of the blood urea nitrogen/creatinine ratio in gastrointestinal bleeding. Am J Emerg Med. 1999 Jan;17(1):70-2. PMID 9928705 [http://dx.doi.org/10.1016/S0735-6757(99)90021-9 full text]
| |
| *{{note|2}} Witting MD, Magder L, Heins AE, Mattu A, Granja CA, Baumgarten M. ED predictors of upper gastrointestinal tract bleeding in patients without hematemesis. Am J Emerg Med. 2006 May;24(3):280-5. PMID 16635697 [http://dx.doi.org/10.1016/j.ajem.2005.11.005 full text]
| |
| *{{note|3}} Witting MD, Magder L, Heins AE, Mattu A, Granja CA, Baumgarten M. Usefulness and validity of diagnostic nasogastric aspiration in patients without hematemesis. Ann Emerg Med. 2004 Apr;43(4):525-32. PMID 15039700 [http://dx.doi.org/10.1016/j.annemergmed.2003.09.002 full text]
| |
| *{{note|4}} Cuellar RE, Gavaler JS, Alexander JA, Brouillette DE, Chien MC, Yoo YK, Rabinovitz M, Stone BG, Van Thiel DH. Gastrointestinal tract hemorrhage. The value of a nasogastric aspirate. Arch Intern Med. 1990 Jul;150(7):1381-4. PMID 2196022
| |
| *{{note|5}} Rosenthal P, Thompson J, Singh M. Detection of occult blood in gastric juice. J Clin Gastroenterol. 1984 Apr;6(2):119-21. PMID 6715849
| |
| *{{note|6}} Holman JS, Shwed JA. Influence of sucralfate on the detection of occult blood in simulated gastric fluid by two screening tests. Clin Pharm. 1992 Jul;11(7):625-7. PMID 1617913
| |
| | |
| ==See also==
| |
| * [[Lower gastrointestinal bleeding]] | | * [[Lower gastrointestinal bleeding]] |
| * [[Rockall score]] | | * [[Rockall score]] |
|
| |
|
| ==External links==
| | [[Category:Disease]] |
| * {{FPnotebook|GI267}}
| |
| * [http://www.patient.co.uk/showdoc/40000851/ Patient.uk]
| |
| | |
| | |
| {{Gastroenterology}}
| |
| | |
| [[Category:Gastroenterology]] | | [[Category:Gastroenterology]] |
| [[Category:Medical emergencies]] | | [[Category:Medical emergencies]] |
| [[Category:Emergency medicine]] | | [[Category:Emergency medicine]] |
| [[Category:Needs patient information]]
| | |
| [[Category:Mature chapter]]
| |
|
| |
|
| [[de:Obere Gastrointestinale Blutung]] | | [[de:Obere Gastrointestinale Blutung]] |