Transjugular intrahepatic portosystemic shunt
| Transjugular intrahepatic portosystemic shunt | |
 | |
|---|---|
| TIPS Procedure |
| https://www.youtube.com/watch?v=O2u4_hF3234%7C350}} |
|
Transjugular intrahepatic portosystemic shunt Microchapters |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Umar Ahmad, M.D.[2]
Overview
A transjugular intrahepatic portosystemic shunt, also TIPS, is an artificial channel in the liver from the portal vein to a hepatic vein (for blood). It is created endovascularly (via the blood vessels) by physicians via the jugular vein.
It is used to treat portal hypertension (which often is due to scarring of the liver (liver cirrhosis) which frequently leads to intestinal bleeding (esophageal varices) or the buildup of fluid within the abdomen (ascites).
History
Transjugular intrahepatic portosystemic shunt (TIPS) creation is the percutaneous formation of a tract between the hepatic vein and the intrahepatic segment of the portal vein in order to reduce the portal venous pressure. The blood is shunted away from the liver parenchymal sinusoids, thus reducing the portal pressure. [[null 1], [null 2], [null 3]]TIPS, therefore, represents a first-line treatment for complications of portal hypertension, typically in patients with decompensated liver cirrhosis.
Indications
Accepted indications for TIPS include the following:
- Uncontrolled variceal hemorrhage from esophageal, gastric, and intestinal varices that do not respond to endoscopic and medical management null 4
- Refractory ascites
- Hepatic pleural effusion (hydrothorax)
Controversial indications for TIPS include the following:
- Bridge to transplantation and retransplantation [[null 5], [null 6]]
- Budd-Chiari syndrome
- Hepatorenal syndrome (HRS)
- Veno-occlusive disease (VOD)
Contraindications
Absolute contraindications for TIPS include the following:
- Severe and progressive liver failure (on the basis of the Child-Pugh score; scores A and B have a better outcome than score C)
- Severe encephalopathy
- Polycystic liver disease
- Severe right-heart failure
Relative contraindications for TIPS include the following:
- Portal and hepatic vein thrombosis
- Pulmonary hypertension
- Hepatopulmonary syndrome
- Active infection
- Tumor within the expected path of the shunt
Preprocedure
•Equipment
Equipment used for transjugular intrahepatic portosystemic shunt (TIPS) creation includes the following:
- Good ultrasound machine with linear-array probe
- Fluoroscopy
- Chlorhexidine or povidone-iodine solution for skin disinfection
- Heparinized saline (1000-2000 U heparin in 1000 mL of 0.9% NaCl)
- Basic angiography set
- Sheath, 5 French, and curved catheter
- Guide wires - 0.035-in. Terumo Glidewire and exchange-length 0.035-in. Amplatz wire
- Pressure transducer
- TIPS kit (Cook Medical, Bloomington, IN; see the first image below) - Sheath, 10 French, 40 cm; guide catheter, 51 cm, with metal stiffener; portal venous access needle, 60 cm
- Medical CO 2 and its kit null 12 (if available)
- Angioplasty balloons, typically 8 mm × 40 mm
- Covered stent - Gore Viatorr (WL Gore, Flagstaff, AZ) or another brand, such as Wallgraft (Boston Scientific, Natick, MA; the advantage of the Gore Viatorr is the design, which consists of a distal 2-cm-long unlined segment that is deployed in the portal vein and therefore gives better anchorage without obstructing the flow and allows for nutrient portal perfusion (see the second image below)
- Bare stents may be used, if needed, to extend to the right atrium null 13
Typical TIPS kit.
[null View Media Gallery]
•Patient Prep
Anesthesia
General anesthesia is usually required for pediatric patients and is preferred in many institutions for adults as well. Procedural sedation may be used, depending on local practices. Midazolam with fentanyl citrate is a reasonable combination for achieving procedural sedation. Local anesthesia is achieved with approximately 5 mL of lidocaine 1% at the jugular puncture site.
Positioning
Position the patient supine, with the neck turned away from the side of vein puncture. Avoid pillows unless they are needed.
Procedure
Creation of Transjugular Intrahepatic Portosystemic Shunt
Transjugular intrahepatic portosystemic shunt (TIPS) creation proceeds as follows.[[null 14], [null 15], [null 7]]
Preparation
Review preprocedural vascular ultrasound studies or computed tomography (CT) scans of the abdomen to confirm the patency of the portal vein and assess for anatomic limitations. Determine the Model for End-stage Liver Disease (MELD) score; this helps predict TIPS mortality, which is higher with a MELD score of 18 or above. null 16 (See the MELD Score for End-Stage Liver Disease calculator.) Addition of sodium assessment to the MELD score may further enhance prediction of TIPS mortality. null 17
Obtain informed consent.
Ensure that the patient has no contrast allergy, has a platelet count higher than 50,000/μL, and has a relatively normal international normalized ratio (INR). Consider broad-spectrum antibiotic prophylaxis.
Procedure
If the patient has ascites with significant volume, perform paracentesis first. Clean the skin on the neck with chlorhexidine or povidone-iodine solution. Use ultrasonographic guidance to choose a point on the skin above the vein.
Make a small (≤1 cm) horizontal skin incision. Using ultrasonographic guidance and a micropuncture or an 18-gauge access needle, puncture the anterior wall of the vein, and enter the vein (see the video below). Aspirate venous blood to confirm the needle position. Ultrasound-guided puncture. [null View Media Gallery]
Advance the 0.035-in. guide wire, and insert the accompanying 5-French sheath over the wire. Use a curved catheter and Terumo hydrophilic wire to access the right hepatic vein. Wedge the catheter in the hepatic vein. Obtain wedged hepatic and inferior vena cava (IVC)/right atrial pressure measurements, and calculate the gradient.
Perform portal angiography (if available), using medical CO2 (see the image below). Because the catheter is wedged, an indirect portogram along with a hepatic venogram can be obtained. Use the images to confirm the patency of both veins.null 15 Use the image as a fluoroscopic fade/roadmap, or mark the portal vein and hepatic veins on screen. Either way, lock the table in position.
CO2 angiography.
[null View Media Gallery]
Insert an Amplatz wire, and then exchange the Cobra-2 catheter and 5-French sheath for the 10-French sheath with dilator. Remove the dilator, and introduce the inner sheath, loaded together with the metal stiffener. Insert the system up to 1 cm from the point of intersection of the two veins.
Remove the wire, and insert the catheter with the needle. Turn the system, using the metal arrow on the stiffener anteriorly (on the assumption of placement in the right hepatic vein), and advance the needle with the catheter in an anteroinferior direction parallel to the spine, aiming for the portal vein. Start the throw approximately 2 cm from the confluence of the right hepatic vein and the IVC. The right portal vein is typically accessed 0.5-1.5 vertebral body widths lateral to the spine between T10 and T12.
Remove the needle, and attach a small syringe with 1 mL of contrast to the catheter. Aspirate while gently withdrawing. A loss of resistance is felt when in the portal vein. Confirm by aspiration and then injection of contrast.
Once in the portal vein, insert a Terumo Glidewire. Advance the wire into the superior mesenteric vein or the splenic vein, and advance the catheter.
Obtain portal and central pressure measurements to confirm the gradient.
Exchange the Terumo wire for an 180-cm Amplatz wire. Perform angioplasty of the tract (with a 6- or 8-mm balloon). Advance a 10-French sheath into the portal vein; replacing the dilator is likely to be helpful.
Exchange the catheter for a calibrated pigtail catheter (see the first image below). Perform a double-flush angiogram via both the pigtail and the side arm of the sheath (with the inner metal stiffener removed and sheath pulled back into the hepatic vein) to obtain images of hepatic and portal veins (see the second image below). Use these images to calculate the length of stent required. Measure from the portal vein to the confluence of the hepatic vein and the IVC. To correctly size a Viatorr stent, add 1-2 cm to the measured length.
Pigtail for calibration.
[null View Media Gallery]
Pre-stent portal and right atrial pressures.
[null View Media Gallery]
Reinsert the Amplatz wire, and advance the sheath back into the portal vein. Remove the pigtail catheter. Insert the stent over the wire into position; be careful to keep the Viatorr stent confined by the packaging sheath until it is fully introduced into the 10-French sheath, and do not advance the stent beyond the sheath tip in the portal vein. Sheath and stent should extend approximately 3 cm into the portal vein.
Withdraw the outer TIPS sheath, and then deploy the stent as per its prescribed mechanism. With the Viatorr, an upstream 2-cm-long uncovered segment is deployed by withdrawing the sheath (see the images below). Positioning may be fine-tuned at this point to achieve the goal of placing the uncovered portion in the portal vein and the covered portion in the tract/hepatic vein. Undersizing the initial tract angioplasty may help give a tactile sense of the junction of the portal vein and the tract.
Deploying of stent.
[null View Media Gallery]
Deploying.
[null View Media Gallery]
Perform a portogram to assess flow through stent and any waisting. Measure pressures to ensure a typical goal portohepatic gradient of less than 12 mm Hg. If necessary, dilate the stent with an 8-mm balloon. If the stent does not reach the confluence of the hepatic vein and the IVC, it may be extended with an additional uncovered stent. The images below depict poststent dilatation.
Poststent dilatation.
[null View Media Gallery]
Dilatation.
[null View Media Gallery]
Postprocedure
Monitoring and Follow-up
The high frequency of shunt stenosis warrants close surveillance with Doppler ultrasonography or portography. Patients undergo a baseline Doppler study within 24 hours of the procedure to document functional parameters, including the direction of portal vein flow and flow velocities throughout the shunt and within the hepatic vein. Although TIPS venography with direct portal and right atrial pressure measurements is the criterion standard for stent assessment, high sensitivity and specificity for shunt function has been reported with certain Doppler criteria, as follows:
- Absent flow
- Low peak shunt velocity (<50 to 90 cm/s)
- High peak shunt velocity (190 cm/s)
- Low mean PV velocity (<30 cm/s)
- Return of antegrade flow in the intrahepatic PVs
- Significant change in shunt velocity (>50 cm/s) as compared with the immediate postprocedural result
In the acute phase, the stent can thrombose. To treat this, the stent can be lysed, or mechanical thrombectomy can be performed. If later in-stent stenosis occurs, perform angioplasty or insert another stent, as required.
Postprocedural follow-up for TIPS placement is important to ensure patency. Post-TIPS Doppler ultrasonography may be performed at 24 hours, 3 months, 6 months, 12 months, and annually thereafter.
Outcome
The technical success of TIPS placement is related to the experience and skill of the interventional radiologist. Data from three large centers (University of California, San Francisco; University of Pennsylvania; and the Freiberg group) demonstrated technical success rates of more than 90%.
Successful TIPS placement results in a portosystemic gradient of less than 12 mm Hg and immediate control of variceal-related bleeding. A target portosystemic gradient of 12 mm Hg is used as varices tend not to bleed when the gradient is less than 12 mm Hg. When technical failure occurs, it is usually due to an anatomic situation that prevents acceptable portal venous puncture. Significant reduction in ascites usually occurs within 1 month of the procedure, and this is estimated to occur in 50-90% of cases. [[null 7], [null 8], [null 9], [null 10]]
Late stenosis and occlusion are usually related to pseudointimal hyperplasia within the stent or, more commonly, intimal hyperplasia within the hepatic vein. In most cases, the stenotic stent can be crossed with a guide wire and recanalized with balloon dilation (see the image below) or repeat stent placement to improve long-term patency rates. Primary patency after TIPS placement has been reported to be 66% and 42% after 1 and 2 years. Primary-assisted patency rates at 1 and 2 years are reported to be 83% and 79%, respectively, and secondary patency rates at 1 and 2 years are reported to be 96% and 90%. null 8
Balloon angioplasty used to treat hyperplasia.
[null View Media Gallery]
Reported figures for 30-day mortality vary among centers, and nearly all centers report few or no deaths directly related to the procedure itself. Early mortality has been shown to be related to the Acute Physiology and Chronic Health Evaluation (APACHE) II score. Patients with severe systemic disease with an APACHE II score higher than 20 have a greater risk for early mortality, compared with others.
Patients with active bleeding during the procedure also have increased early mortality. The 30-day mortality is in the range of 3-30%; the variation within this range is related to the preprocedural Child classification and whether the procedure was performed on an emergency basis or an elective basis. null 11 In 1995, LaBerge et al reported that cumulative survival rates in patients with Child grades of A, B, and C, respectively, were 75%, 68%, and 49% at 1 year and 75%, 55%, and 43% at 2 years.
Complications
Immediate complications of TIPS placement include the following:
- Inability to place stent
- Bleeding (hemoperitoneum; 3%)
- Trauma to liver and heart [[null 18], [null 8]]
- Stent infection null 11
- Bile leak and peritonitis
- Encephalopathy (15%) - This may be amenable to medical therapy null 19 ; if it is severe, the shunt may have to be narrowed or embolized null 20
- Heart failure
- Stent thrombosis
- Death (1%)
- Stent malposition null 21
- Nephropathy
Delayed complications of TIPS placement include the following [[null 22], [null 23], [null 24]] :
- Encephalopathy [[null 23], [null 24]]
- In-stent stenosis - Greater than 50% stenosis is seen in 25% of TIPS cases; this can be addressed with angioplasty
- Stent thrombosis
- Stent occlusion
- Hemolytic anemia
- Severe hyperbilirubinemia
- Radiation injury
Various endovascular and percutaneous approaches to managing TIPS dysfunction have been described. null 25
Pearls
Pearls
Always perform Doppler ultrasonography to assess the portal vein before starting the TIPS procedure to confirm that the portal vein is not thrombosed.
If the middle hepatic vein is used, remember to rotate the TIPS sheath and stiffener posteriorly because the middle portal vein lies posterior and inferior to the hepatic vein.
To confirm entry into portal vein, inject contrast material. Contrast flowing toward the right atrium indicates hepatic vein location. Static contrast likely indicates biliary system location. Contrast flowing to liver periphery can indicate location in the hepatic artery or portal vein; however, the portal radicals are larger in size.
If insertion is unsuccessful, pull the catheter back into the sheath, reinsert the needle, and try again.
When using Amplatz wires, always keep the tip of the wire under control. If the wire tip is not properly controlled, it can easily perforate the liver or the mesentery.
If covered shunt patency is difficult to assess on follow-up Doppler ultrasonography, CT may be performed.
Mechanism of action
A TIPS decreases the effective vascular resistance of the liver. The result is a reduced pressure drop over the liver and a decreased portal venous pressure. This, in turn, lessens the pressure on the blood vessels in the intestine so that future bleeding is less likely to occur. The reduced pressure also makes less fluid develop, although this benefit may take weeks or months to occur.
Implantation
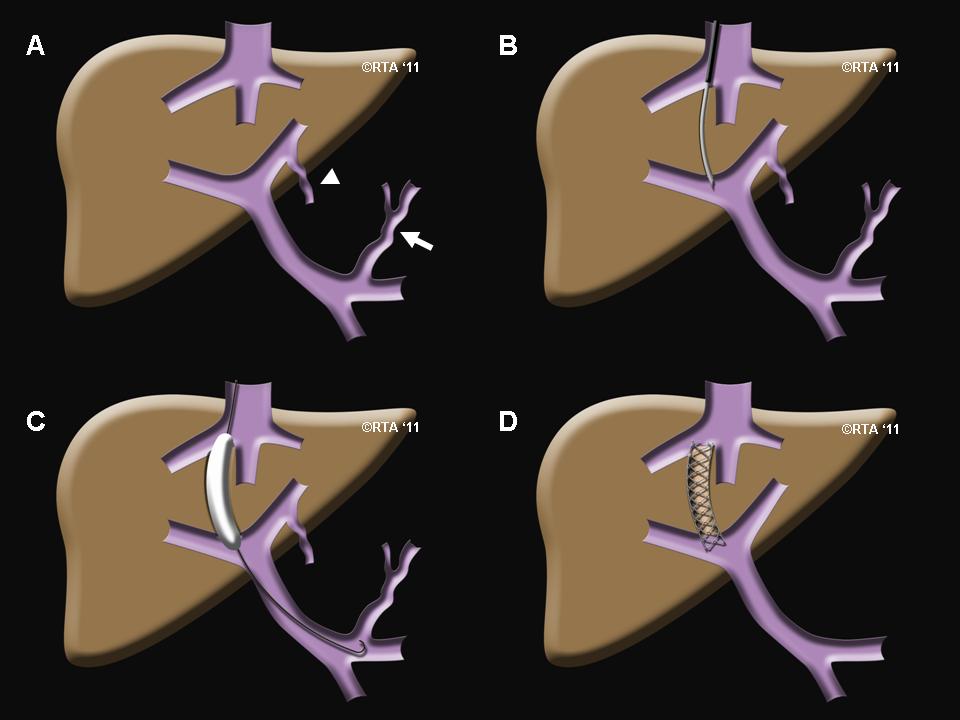
Transjugular intrahepatic portosystemic shunts are typically placed by interventional radiologists under fluoroscopic guidance.[1] Access to the liver, as the name transjugular suggests, is gained via the jugular vein in the neck. Once access to the jugular vein is confirmed, a guidewire and introducer sheath is typically placed to facilitate the shunt's placement. This enables the interventional radiologist to gain access to the patient's liver vein (hepatic vein) by passing through the heart. The shunt is created by advancing a special needle through the sheath system to connect the hepatic vein to the large vein near the center of the liver, the portal vein. The channel for the shunt is next created by inflating an angioplasty balloon within the liver along the tract of created by the needle. The shunt is completed by placing a special mesh tube known as a stent or endograft to establish the connection between the high pressure portal vein with the lower pressure hepatic vein. After the procedure, fluoroscopic images are made to show placement and pressure measurements in the portal vein and inferior vena cava are often done.
Use in hepatorenal syndrome
TIPS has shown some promise for patients with hepatorenal syndrome.[2]
Complications
A complication of umbilical hernia has been recently reported.[3]
Related Chapters
Reference
- ↑ What You Need to Know about the Transjugular Intrahepatic Portosystemic Shunt (TIPS). Cleveland Clinic. URL: http://www.clevelandclinic.org/health/health-info/docs/0200/0237.asp?index=4956. Accessed: February 19, 2007.
- ↑ Guevara M, Rodes J. Hepatorenal syndrome. Int J Biochem Cell Biol. 2005 Jan;37(1):22-6. PMID 15381144.
- ↑ Mallavarapu RK, Grimsley EW (2007). "Incarcerated umbilical hernia after transjugular intrahepatic portosystemic shunt procedure for refractory ascites". Clin. Gastroenterol. Hepatol. 5 (9): A26. doi:10.1016/j.cgh.2007.07.018. PMID 17825762.