Transitional cell carcinoma CT: Difference between revisions
(Mahshid) |
|||
| Line 6: | Line 6: | ||
==CT Scan== | ==CT Scan== | ||
* CT, with and without contrast, is the preferred study for all patients with bladder cancer, regardless of stage.<ref name="pmid28456635">{{cite journal| author=Chang SS, Bochner BH, Chou R, Dreicer R, Kamat AM, Lerner SP et al.| title=Treatment of Non-Metastatic Muscle-Invasive Bladder Cancer: AUA/ASCO/ASTRO/SUO Guideline. | journal=J Urol | year= 2017 | volume= 198 | issue= 3 | pages= 552-559 | pmid=28456635 | doi=10.1016/j.juro.2017.04.086 | pmc=5626446 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28456635 }} </ref> | |||
Abdominal and pelvic CT scans may be helpful in the diagnosis and staging of transitional cell carcinoma: | Abdominal and pelvic CT scans may be helpful in the diagnosis and staging of transitional cell carcinoma: | ||
===Transitional cell carcinoma of bladder=== | ===Transitional cell carcinoma of bladder=== | ||
Revision as of 15:58, 15 July 2019
|
Transitional cell carcinoma Microchapters |
|
Differentiating Transitional cell carcinoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Transitional cell carcinoma CT On the Web |
|
American Roentgen Ray Society Images of Transitional cell carcinoma CT |
|
Directions to Hospitals Treating Transitional cell carcinoma |
|
Risk calculators and risk factors for Transitional cell carcinoma CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Suveenkrishna Pothuru, M.B,B.S. [2]
Overview
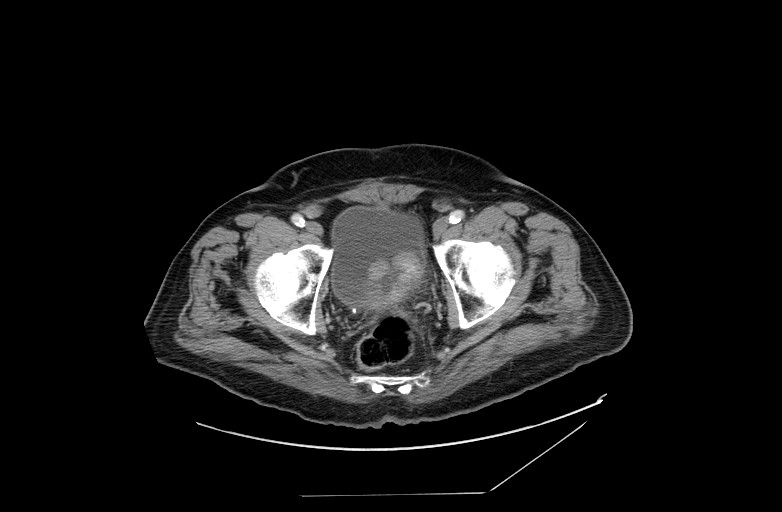
Abdominal and pelvic CT scans may be helpful in the diagnosis and staging of transitional cell carcinoma. On CT scan, transitional cell carcinoma of bladder is characterized by either focal regions of thickening of the bladder wall, or as masses protruding into the bladder lumen, or in advanced cases, extending into adjacent tissues.[1] On CT scan, transitional cell carcinoma of upper urinary tract is characterized by homogenously enhancing mass that centered on the renal pelvis and extend towards pelviureteric junction, preserved renal contour, and focal pelvicalyceal filling defect.[2]
CT Scan
- CT, with and without contrast, is the preferred study for all patients with bladder cancer, regardless of stage.[3]
Abdominal and pelvic CT scans may be helpful in the diagnosis and staging of transitional cell carcinoma:
Transitional cell carcinoma of bladder
- Transitional cell carcinoma of bladder appear as either focal regions of thickening of the bladder wall, or as masses protruding into the bladder lumen, or in advanced cases, extending into adjacent tissues.[1]
- Care should be taken in assessing bladder wall thickness as this changes with the degree of bladder distension and varies from patient to patient, e.g. patients with bladder outlet obstruction due to benign prostatic hypertrophy. In general, however, asymmetric mural thickening should be viewed with suspicion.
- The masses are of soft tissue attenuation and may be encrusted with small calcifications.
- Although unable to distinguish between T1, T2, and T3a (microscopic extravesical spread), CT is able to distinguish T3b tumors (stranding/nodules in perivesical fat) and T4 tumors (direct extension into adjacent structures/loss of normal fat plane).
- Care should be exercised when interpreting stranding or nodularity following transurethral resection or even biopsy, as these changes may be postoperative.
- Nodal metastases are common, observed in 30% of T2 tumors and 60% of T3 and T4 tumors.
Transitional cell carcinoma of renal pelvis
- CT scan may be helpful in the diagnosis of transitional cell carcinoma of renal pelvis. Findings on CT scan diagnostic of intrarenal transitional cell carcinoma include:[2][4][5]
| Intrarenal transitional cell carcinoma CT findings |
|---|
| Homogenously enhancing mass |
| Mass centered on the renal pelvis and extend towards pelviureteric junction |
| Preserved renal contour |
| Focal pelvicalyceal filling defect |
| Obliteration of the renal sinus fat |
- Transitional cell carcinomas are typically of soft tissue density with only mild enhancement, usually significantly less enhancing than renal parenchyma or renal cell carcinoma (although the the distinction cannot always be made).
- They are usually centred on the renal pelvis (rather than the renal parenchyma as is the case with renal cell carcinoma).
- Range in size from small filling defects (difficult to see without distension or collecting system contrast) to large masses which obliterate the renal sinus fat (transitional cell carcinoma is one of the causes of the so-called faceless kidney).
- Unlike renal cell carcinoma that tend to distort the renal outline, even large infiltrating transitional cell carcinoma maintain a normal renal shape.
- Larger tumors may have areas of necrosis.
- In cases of the tumor being small and located at the pelviureteric junction with resultant hydronephrosis, a small soft tissue mass should be sought.
- In contrast to congenital pelviureteric junction obstruction, the calices are typically dilated, and the renal pelvis wall may be thickened.
- Occasionally numerous small calcification may be present, located on the surface of papillary projections.
Patient #1
Patient#2
References
- ↑ 1.0 1.1 Transitional cell carcinoma of the bladder. Dr Ian Bickle and Dr Frank Gaillard et al. Radiopaedia.org 2015.http://radiopaedia.org/articles/transitional-cell-carcinoma-of-the-bladder Accessed on February, 18 2015
- ↑ 2.0 2.1 Raza SA, Sohaib SA, Sahdev A, Bharwani N, Heenan S, Verma H; et al. (2012). "Centrally infiltrating renal masses on CT: differentiating intrarenal transitional cell carcinoma from centrally located renal cell carcinoma". AJR Am J Roentgenol. 198 (4): 846–53. doi:10.2214/AJR.11.7376. PMID 22451550.
- ↑ Chang SS, Bochner BH, Chou R, Dreicer R, Kamat AM, Lerner SP; et al. (2017). "Treatment of Non-Metastatic Muscle-Invasive Bladder Cancer: AUA/ASCO/ASTRO/SUO Guideline". J Urol. 198 (3): 552–559. doi:10.1016/j.juro.2017.04.086. PMC 5626446. PMID 28456635.
- ↑ Fukuya T, Honda H, Nakata H, Egashira K, Watanabe H, Naitou S; et al. (1994). "Computed tomographic findings of invasive transitional cell carcinoma in the kidney". Radiat Med. 12 (1): 6–10. PMID 8016405.
- ↑ Browne, Ronan F. J.; Meehan, Conor P.; Colville, Jane; Power, Raymond; Torreggiani, William C. (2005). "Transitional Cell Carcinoma of the Upper Urinary Tract: Spectrum of Imaging Findings1". RadioGraphics. 25 (6): 1609–1627. doi:10.1148/rg.256045517. ISSN 0271-5333.