Transcatheter aortic valve replacement
| Resident Survival Guide |
|
Aortic Stenosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Percutaneous Aortic Balloon Valvotomy (PABV) or Aortic Valvuloplasty |
|
Transcatheter Aortic Valve Replacement (TAVR) |
|
Case Studies |
|
Transcatheter aortic valve replacement On the Web |
|
American Roentgen Ray Society Images of Transcatheter aortic valve replacement |
|
Directions to Hospitals Treating Transcatheter aortic valve replacement |
|
Risk calculators and risk factors for Transcatheter aortic valve replacement |
Editor(s)-In-Chief: Roger Laham, M.D., C. Michael Gibson, M.S., M.D.; Associate Editor(s)-in-Chief: Saleh El Dassouki, MD [1]; Seyedmahdi Pahlavani, M.D. [2]; Tarek Nafee, M.D. [3]; Arzu Kalayci, M.D. [4]
Synonyms and keywords: TAVI; Edward's valve; Edward's SAPIEN transcatheter heart valve; CoreValve; percutaneous aortic valve replacement; PAVR
Overview
Until recently, aortic valve replacement (AVR) was the only effective treatment for severe symptomatic aortic stenosis. However, over the past decade percutaneous treatment of aortic valve disease with implantation of a stent-based valve prosthesis has been introduced as a new treatment in patients considered inoperable because of severe co-morbidities.[1] In Transcatheter Aortic Valve Implantation (TAVI) also known as Percutaneous Aortic Valve Replacement (PAVR), a synthetic valve is advanced to the heart through a small hole made in groin. This procedure is similar in its mechanism to the insertion of a stent, or performing balloon angioplasty albeit with much larger equipment. Traditional aortic valve replacement is an invasive surgical procedure, with considerable mortality and morbidity, especially in more fragile patients. In the newly developed TAVI procedure, the dysfunctional aortic valve is replaced percutaneously, which obviates the need for open heart surgery.[2]
Comparing TAVR and SAVR
Surgical Aortic Valve Repair (SAVR) is the traditional way of treating a stenotic aortic valve. In the last decade TAVR has emerged as a viable option for patients at high surgical risk or at high risk for post-surgical complications. The most current 2014 AHA/ACC guideline for management of patients with valvular heart disease recommends the following:[2]
| Class of Recommendation | Recommendation | Evidence Level |
|---|---|---|
| Class I | "SAVR is recommended in patients who meet an indication for AVR with low or intermediate surgical risk" | A |
| Class I | "For patients in whom TAVR or high-risk SAVR is being considered, members of a Heart Valve Team should collaborate to provide optimal patient care" | C |
| Class I | "TAVR is recommended in patients who meet an indication for AVR for AS who have a prohibitive surgical risk and a predicted post-TAVR survival >12 months" | B |
| Class IIa | "TAVR is a reasonable alternative to SAVR in patients who meet an indication for AVR and who have high surgical risk" | B |
| Class IIb | "Percutaneous aortic balloon dilation may be considered as a bridge to SAVR or TAVR in severely symptomatic patients with severe AS" | C |
| Class III: No Benefit | "TAVR is not recommended in patients in whom existing comorbidities would preclude the expected benefit from correction of AS" | B |
In recent years, terminology has arose to define patients who qualify for TAVR as "inoperable patients" who are at >50% risk of mortality at 30 days after a potential SAVR procedure. There is much debate regarding the subjective nature of defining a patient as "inoperable"; however, the heart valve team should collaborate to determine the optimal procedure for the patient.
TAVR has demonstrated up to a 20% risk reduction in all-cause-mortality at 12 months which is sustained for up to 5 years post-procedure, when compared to SAVR. In high risk patients such as the elderly and those with a NYHA III or IV functional status, TAVR showed non-inferiority to the traditional SAVR procedure and regardless of the procedure undertaken, patients maintained a NYHA I or II functionality for up to 5 years post-procedure.
It is noteworthy to say that TAVR is associated with a significant and sustained reduction in risk of ischemic stroke for 30 days and up to 2 years after the procedure compared to surgery. Nevertheless, SAVR continues to play a role in patients who require an aortic valve replacement with lower surgical risk.
Patient Selection
Patient selection is critical prior to performance of transcatheter aortic valve implant (TAVI). TAVI candidates must have severe aortic stenosis with a contraindication(s) to surgery. The patients selected for this procedure should have a potential for functional improvement after valve replacement.[3] Selection criteria depend on thorough evaluation of the aortic valve, mitral valve, ejection fraction, vascular access and coronary angiography. A thorough echocardiographic evaluation of the aortic valve is necessary to determine the valve area, calcification, peak velocity, the transvalvular gradient and aortic annulus size. Aortic incompetence should be assessed as well since more than moderate aortic incompetence before the procedure is a contraindication for TAVI. Tortuosity, calcification and minimal luminal diameter of the aorta, iliac and femoral arteries would also influence patient selection and the technical approach used during the procedure.
Valve Types
- There are currently 8 prosthetic transcatheter valve types which are available. Two of these are FDA approved in the United States.[2]
- The CHOICE trial is a small study which compared the most prominent two valves (CORE and SAPIEN) and no major significant differences were found in primary clinical endpoints between both valves. Nevertheless, there are situations, anatomical variability, and operator preferences that continue to make one valve more preferable to the other, depending on the situation. There are currently three ongoing major trials comparing newer generation valves to the aforementioned devices.
Synopsis
| Valve | Type of Expansion | Device Placement | Year of Introduction | FDA approval | Available Sizes (in mm) |
|---|---|---|---|---|---|
| Core valve | Self expanding | TF | 2005 | Yes | 23, 26, 29 |
| Edwards Sapien valves | Balloon expandable | TF | 2007 | Yes | 20, 23, 26, 29 |
| Acurate neo valve[4] | Self expanding | TF, TA | 2011 | No | S, M, L † |
| Jena Valve | Self expanding | TF, TA | 2011 | No | 23, 25, 27 |
| St. Jude Medical Portico | Self expanding | TF | 2014 | No | 23, 25, 27, 29 |
| Direct Flow Medical Valve | Self expanding | TF | 2013 | No | 23, 25, 27, 29 |
| Medtronic Engager Valve | Self expanding | TF | 2013 | No | 23, 26 |
| Boston Scientific Lotus Valve | Mechanically Expanded | TF | 2013 | No | 23,25,27 |
TF: Trasfemoral, TA: Transapical
† They claimed that can cover aortic annulus diameters from 21 to 27 mm.
Description of Valves
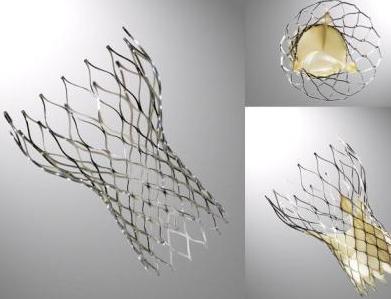
Core Valve
The Core-Valve device was first inserted in 2005.[1][5] It consists of three leaflets of bioprosthetic pericardial valve tissue mounted on a self-expendable nitinol stent, which expands from the left ventricular outflow tract (LVOT) to the ascending aorta. The Core Valve frame is currently available in 3 sizes (23 mm, 26 mm and 29 mm). The multilevel nitinol frame was designed for optimal functionality,stability,and durability. The inflow portion of the frame exerts high radial expansive force to provide proper support of the frame within the annular location.[6] The design of this portion of the frame with its radial strength prevents annular recoil, allowing the frame to partially conform to the non circular shape of the aortic annulus. The center portion of the frame has very high hoop strength that resists size and shape deformation which is a very important part of the device since it contains the valve leaflets, which are supra-annular. This center portion of the frame is concave to allow normal flow of blood through the coronary arteries and coronary cannulation after implantation. The largest part of the frame is the outflow portion that exerts low radial forces and allow optimal flow of blood through the valve. For the tissue in the valves, porcine (pig) pericardium was selected due to its lower profile (compared with bovine (cow) pericardium) and its durability. The trileaflet valve is made of six individual pieces of porcine pericardium, with three pieces used to make a skirt at the inflow section of the valve thus preventing aortic regurgitation and three leaflet elements that are constructed with long commissures to distribute the aortic pressure load to the valve leaflets and the commissural posts.
The Edwards SAPIEN Valves
SAPIEN XT
This prosthesis is considered the second generation of the Cribier-Edwards valve.[7] It is a balloon-expendable valve made of a stainless steel frame covered by a Dacron skirt where three leaflets of pericardium are sutured. The device is placed in a subcoronary position during rapid ventricular pacing, via anterograde, transapical or a retrograde transfemoral approach. It is available in two sizes (23mm and 26 mm). In the first generation the leaflets were made of equine (horse) pericardium; in the second generation they are made of bovine (cow) pericardium with improvements made in the frame suture and an increase in the skirt length to decrease the risk of aortic regurgitation.
SAPIEN 3
The Edwards SAPIEN 3 Transcatheter Heart Valve is comprised of a balloon-expandable, radiopaque, cobalt-chromium frame, trileaflet bovine pericardial tissue valve, and polyethylene terephthalate (PET) fabric skirt. The leaflets are treated according to the Carpentier-Edwards ThermaFix process. It is available in 4 sizes (20mm, 23mm, 26mm and 29mm).
-
The Edwards SAPIEN XT
-
The Edwards SAPIEN 3
St. Jude Portico valve
The valve stent is made from nitinol, a nickel-titanium alloy that has self-expanding properties and is radiopaque. The valve cuff is made from porcine pericardium that is sutured to the stent frame. The cuff provides the sealing area for implantation. The valve orifice is made by suturing three valve leaflets, each made from a single layer of bovine pericardium, into a tri-leaflet configuration on the stent frame. It is available in 4 sizes (23mm, 25mm, 27mm and 29mm).

Direct Flow Medical valve
It features a metal-free frame. The Direct Flow Medical System incorporates a polymer frame, which is expanded using pressurized saline and contrast for placement, assessment and repositioning. The saline/contrast solution is exchanged for a quick-curing polymer that solidifies and secures the valve in place once optimal positioning is reached. It is available in 4 sizes(23 mm, 25 mm, 27 mm, 29 mm).

Symetis Acurate neo valve
Acurate neo is composed of a porcine pericardial tissue valve sutured within a self-expanding nitinol stent covered by a pericardial skirt on the outer and inner surface of the stent body.It is a nitinol-based valve that incorporate features that facilitate positioning and anatomic orientation in relation to the native valve commissures and coronaries. The valve is currently implanted only transapically. It is available in three sizes (S, M, L) and its delivery system boasts an 18F outer diameter and it cover the aortic annulus diameters from 21 to 27 mm.

Medtronic Engager valve
It has a self expanding nitinol frame and polyester skirt and bovine pericardial tissue. It is available in 2 sizes(23 mm, 26 mm)

Lotus edge valve
Lotus valve consisting of a pre-attached, stent-mounted tissue valve prosthesis and catheter delivery system for guidance and percutaneous placement of the valve. It is the first device of its kind that offers controlled mechanical expansion, which allows the valve to be fully deployed, assessed and then released, providing unparalleled control during the procedure. It is available in 3 sizes (23 mm, 25 mm and 27 mm).

Jena valve
The transapical JenaValve prosthesis consists of a natural aortic porcine root bioprosthesis fitted with an outer porcine pericardial patch, a so-called skirt. The JenaValve is available in 3 sizes, 23mm, 25mm and 27mm. It is not commercially available now and is waiting for approval.

Valve Sizing and Positioning
Valve sizing and positioning is of utmost importance in the success of the TAVR procedure and the risk of paraprocedural compications. The utilization of 2D echocardiography was initially used to estimate the annulus size. Currently, the gold standard for estimating the size of the aortic outlet is CT angiography focussing on the area of the valve or the perimeter of the annulus to estimate the required device size. Furthermore, the positioning of the valve must be estimated by an experienced operator as every valve type presents advantages and disadvantages according to the variability in the anatomy. Examining the left ventricular outflow tract, the origin of the coronary arteries, and the sinotubular junction constitute some of the considerations the operator must entertain. Additionally, the positioning of the aorta and the degree of calcification of the valve and the proximal aorta must be assessed in planning a successful procedure.[2]
Contraindications
General contraindications for transcatheter aortic valve implant (TAVI) through every approach include:
- Aortic annulus size <18 mm or >25 mm for balloon expandable devices and <20 mm or >27 mm for self expandable devices.
- Severe mitral regurgitation.
- Presence of apical left ventricle thrombus.
- Aortic root dimension > 45 mm at the sino-tubular junction for self-expandable prostheses.
- Low position of the coronary ostia (<8 mm from the aortic annulus)
- Asymmetric heavy valvular calcification which may compress the coronary arteries during the procedure of TAVI.
- Bicuspid valves - because of the risk of incomplete placement of the prosthesis.
- Intracardiac mass
- Presence of vegetations is an absolute contraindication for TAVI.
- Severe aortic regurgitation
- Serum creatinine >3.0 mg/dL or patient on dialysis
- Left ventricular ejection fraction <20%
- Untreated coronary heart disease requiring revascularization.
- Hemodynamic instability
- Upper gastrointestinal bleed within the past 3 months.
- Cerebrovascular accident (CVA) or transient ischemic attack (TIA) within the last 6 months.
- Aortic aneurysm or severe ilio-femoral insufficiency disease
- Hypertrophic cardiomyopathy
- Bleeding disorders
- Active infective endocarditis
The transfemoral approach has a few specific contraindications which include:
- Severe tortuosity, calcification and narrowing of the iliac arteries
- Previous aorta-femoral bypass
- Abdominal aortic aneurysm
- Severe angulation of the aorta
- Severe atherosclerosis of the ascending aorta and arch of the aorta[8].
Contraindications for transapical approach include:
- Previous surgery to the heart
- Severe respiratory insufficiency
- Chest deformity
Procedure
The diseased valve is first moved aside by aortic balloon valvuloplasty. The Corevalve prosthesis, which is loaded on a specialized delivery catheter, is advanced to the stenosed aortic valve. Once correctly positioned, the external part of the delivery system (the sheath) is progressively retracted, deploying the Corevalve Prosthesis. The delivery catheter is then closed and retrieved. {{#ev:youtube|7EhoUbWHW2A}}
Techniques
Two major catheter based techniques for replacing the aortic valve have been investigated:[9] retrograde percutaneous implantation and direct apical puncture. An antegrade transseptal approach has also been studied but not fully adopted.
Retrograde Approach[10]
After a routine aortic balloon valvuloplasty, a 22F or 24F sheath is advanced from the femoral artery to the aorta. The manipulation of the prosthesis around the aortic arch and through the stenotic valve is facilitated by a steerable, deflectable catheter. Rapid ventricular pacing is used to decrease cardiac output while the delivery balloon is inflated to deploy the prosthesis within the annulus.
Transapical Antegrade Approach[11]
An alternate catheter based method consists of a direct left ventricular apical puncture and antegrade aortic valve implantation via a small anterolateral thoracotomy without the need of cardiopulmonary bypass or sternotomy. This technique is used in patients with severe peripheral arterial disease and heavily calcified ascending aorta and arch (porcelain aorta) who have an increased risk of stroke and other embolic events using other approaches.
Alternative Vascular Access
In some patients, the peripheral vascular anatomy is unsuitable for a transfemoral approach; for such reason a number of other vascular access have been suggested. The Subclavian (ie,axillary) or Transaortic access may be useful in solving such problems.[12] In a series of 54 cases treated via the Subclavian approach in the Italian National Registry, procedural success was achieved in 100% of cases.[13] No specific complications such as vessel rupture or vertebral or internal mammary ischemia associated with Subclavian access were found. No deaths at 30 days in this series, and the 6-month mortality rate was 9.4% and was no different from those who underwent a transfemoral approach.
Complications
Strokes and Transient Ischemic Attacks
The etiology of cerebrovascular events after TAVI is thought to be related to the embolization of atherothrombotic material during advancement of the device to and across the aortic valve.[14] Magnetic resonance imaging have shown that microembolization is common with both balloon-expandable and self-expanding percutaneous valves, as well with surgical aortic valve repair (SAVR), but the presence of clinical strokes are infrequent (2.9%-5.1%)
Aortic Regurgitation
Significant aortic regurgitation caused by paravalvular leak after CoreValve percutaneous implantation is usually an uncommon complication that relates more frequently to low positioning of the CoreValve frame, incomplete expansion of the frame into the eccentrically shaped annulus, rigidity of the underlying aortic annulus due to calcium, or undersizing of the valve relative to the aortic annular size.[15]
Vascular Access Complications
The relatively large-caliber sheath (18F) required for placement of the percutaneous valve may be the cause of various vascular complications. One of the most common vascular events encountered are incomplete arteriotomy closure.[14] Avoiding such complications is possible; preprocedural screening using computed tomographic angiography, vascular ultrasound guidance for arterial access, and alternative (eg, subclavian) access have allowed better selection to avoid those vascular complications.
Coronary Artery Occlusion
Coronary occlusion after TAVI is usually rare but may occur in some cases due to expansion of the native aortic valve across the orifice of the coronary ostium. This complication can be prevented with careful preprocedural screening to ensure adequate sinus of valsava width (30 mm) and height (15 mm).[16]
Conduction Abnormalities
Worsening or new conduction abnormalities are frequently observed with TAVI; more often when self-expandable CoreValve device is used[17][18]. Conduction abnormalities may be due to compression of superficially running left bundle branch (in the uppermost part of ventricular septum) by the lower one third of prosthesis which exerts radial forces for secure anchoring of the stent against the native annulus and outflow septum. Hence, deeper the implantation of the prosthesis into the left ventricular outflow tract, greater is the risk of development of severe conduction defect requiring pacemaker implantation.
A study in Italy reported that 77% of the patients post TAVI developed new onset or worsening of per-existing conduction abnormalities. 44% of the patients developed left bundle branch block (LBBB) and subsequently 39% of the patients underwent implantation of pacemaker. After TAVI, 6 (75%) of 8 patients with right bundle branch block (RBBB) at baseline required pacemaker implantation versus 19 (34%) of 56 patients, who had not had RBBB before TAVI. It was concluded that the RBBB was the only baseline conduction abnormality that significantly affected the occurrence of pacemaker implantation after TAVI because if patients already have a right bundle branch block, then a procedure-induced left bundle branch block will result in a complete atrioventricular block requiring a pacemaker.[19][20]
Other CoreValve implantation complications are:[21]
- QRS duration: In one observational study of 270 patients, the QRS duration increased from 105±23 milliseconds at baseline to 135±29 milliseconds following TAVI. (P<0.01).
- Left Bundle Branch Block (LBBB): The incidence of left bundle-branch block increased from 13% at baseline to 61% following TAVI (P<0.001).
- Permanent pacemaker implantation: Approximately one third of patients will require a permanent pacemaker be implanted by 30 days with a median time to insertion of 4 days (interquartile range, 2.0 to 7.75 days).
- Multivariate predictors of permanent pacemaker implantation included:
- Periprocedural atrioventricular block (odds ratio, 6.29; 95% confidence interval, 3.55 to 11.15)
- Balloon pre-dilatation (odds ratio, 2.68; 95% confidence interval, 2.00 to 3.47)
- Use of a larger 29 mm CoreValve prosthesis (odds ratio, 2.50; 95% confidence interval, 1.22 to 5.11)
- The interventricular septum diameter (odds ratio, 1.18; 95% confidence interval, 1.10 to 3.06)
- A prolonged QRS duration (odds ratio, 3.45; 95% confidence interval, 1.61 to 7.40)
Future Perspectives
TAVR has transformed the treatment and the way of dealing with symptomatic patients suffering from aortic stenosis, particularly in those who are high risk or inoperable for surgical aortic valve replacement (SAVR).[22] When it successfully performed it will It returns the patient to a good prognosis and good life style. It is estimated that 25,000 TAVR done in the U.S in 2015 and an increase in this number is anticipated because of increase in the number of the elderly population. In the United States, the elderly population will reach 50 million by 2019 [23]and this old population are highly vulnerable to degenerative valve disease.
The future of TAVR will be focusing on more technical aspects; trying to reduce the device profile, enhancing it's positioning, retrievability and promoting valve durability with anticalcification treatments. In the last decade, clinicians remained focused on demonstrating efficacy and safety of the procedure. In latter years, the minimalist approach to the deployment of the valves has become the mainstay of advancements in the TAVR procedure. Examples include the avoidance of general anesthesia and the utilization of conscious sedation whenever possible, the reduction of reliance or use of transesophageal echocardiography (TEE), the reduction or elimination of balloon pre-dilatation of the stenosed valve, as well as early discharge programs. With ongoing clinical trials and further advancements in valve technology, TAVR will establish an expanded indication in patients with moderate to severe aortic stenosis.
2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease (VHD) [24][25]
Choice of Intervention
| COR | LOE | RECOMMENDATION | COMMENT/RATIONALE |
|---|---|---|---|
| I | C | For patients in whom TAVR or high-risk surgical AVR is being considered, a heart valve team consisting of an integrated, multidisciplinary group of healthcare professionals with expertise in VHD, cardiac imaging, interventional cardiology, cardiac anesthesia, and cardiac surgery should collaborate to provide optimal patient care. | 2014 recommendation remains current. |
| I | B-NR | Surgical AR is recommended for symptomatic patients with severe AS (Stage D) and asymptomatic patients with severe AS (Stage C) who meet an indication for AVR when surgical risk is low or intermediate. | MODIFIED: LOE updated from A to B-NR. Prior recommendations for intervention choice did not specify patient symptoms. The patient population recommended for surgical AVR encompasses both symptomatic and asymptomatic patients who meet an indication for AVR with low-to-intermediate surgical risk. This is opposed to the patient population recommended for TAVR, in whom symptoms are required to be present. Thus, all recommendations for type of intervention now specify the symptomatic status of the patient. |
| I | A | Surgical AVR or TAVR is recommended for symptomatic patients with severe AS (Stage D) and high risk for surgical AVR, depending on patient specific procedural risks, values, and preferences. | MODIFIED: COR updated from IIa to I, LOE updated from B to A. Longer-term follow-up and additional RCTs have demonstrated that TAVR is equivalent to surgical AVR for severe symptomatic AS when surgical risk is high. |
| I | A | TAVR is recommended for symptomatic patients with severe AS (Stage D) and a prohibitive risk for surgical AVR who have a predicted post-TAVR survival greater than 12 months. | MODIFIED:LOE updated from B to A. Longer-term follow-up from RCTs and additional observational studies has demonstrated the benefit of TAVR in patients with a prohibitive surgical risk. |
| IIa | B-R | TAVR is a reasonable alternative to surgical AVR for symptomatic patients with severe AS (Stage D) and an intermediate surgical risk, depending on patient-specific procedural risks, values, and preferences. | NEW: New RCT showed noninferiority of TAVR to surgical AVR in symptomatic patients with severe AS at intermediate surgical risk. |
| IIb | C | Percutaneous aortic balloon dilation may be considered as a bridge to surgical AVR or TAVR for symptomatic patients with severe AS. | 2014 recommendation remains current. |
| III: No Benefit | C | TAVR is not recommended in patients in whom existing comorbidities would preclude the expected benefit from correction of AS. | 2014 recommendation remains current. |
2017 ESC/EACTS Guidelines for the management of valvular heart disease [26]
Aspects to be considered by the Heart Team for decision between SAVR and TAVI in patients at increased surgical risk
| FAVOURS TAVI | FAVOURS SAVR | |
|---|---|---|
| Clinical Characteristics | ||
| STS/EuroSCORE II <4% (logistic EuroSCORE I <10%) | + | |
| STS/EuroSCORE II ≥4% (logistic EuroSCORE I ≥10%) | + | |
| Presence of severe comorbidity (not adequately reflected by scores) | + | |
| Age <75 | + | |
| Age ≥75 | + | |
| Previous cardiac surgery | + | |
| Frailty | + | |
| Restricted mobility and conditions that may affect the rehabilitation process after the procedure | + | |
| Suspicion of endocarditis | + | |
| Anatomical and technical aspects | ||
| Favourable access for transferral TAVI | + | |
| Sequelae of chest radiation | + | |
| Porcelain aorta | + | |
| Presence of intact coronary bypass grafts at risk when sternotomy is performed | + | |
| Expected patients-Prosthesis mismatch | + | |
| Severe chest deformation or scoliosis | + | |
| Short distance between coronary ostia and aortic valve annulus | + | |
| Size of aortic valve annulus out of range for TAVI | + | |
| Valve morphology (bicuspid, degree of calcification, calcification pattern) unfavourable for TAVI | + | |
| Presence of thrombi in aorta or LV | + | |
| Cardiac conditions in addition to aortic stenosis that require consideration for concomitant intervention | ||
| Severe CAD requiring revascularisation by CABG | + | |
| Severe primary mitral valve disease, which could be treated surgically | + | |
| Severe tricuspid valve disease | + | |
| Aneurysm of the ascending aorta | + | |
| Septal hypertrophy requiring myectomy | + | |
Changes in Recommendations
Indications for Intervention in Symptomatic Aortic Stenosis
| 2012 | 2017 |
|---|---|
| IIb C | NEW: IIa C |
| Intervention may be considered in symptomatic patients with low-flow, low-gradient aortic stenosis and reduced ejection fraction without flow (contractile) reserve. | Intervention should be considered in symptomatic patients with low-flow, low-gradient aortic stenosis and reduced ejection fraction without flow (contractile) reserve, particularly when CT calcium scoring confirms severe aortic stenosis. |
Indications for Surgery in Asymptomatic Aortic Stenosis
| 2012 | 2017 | |
|---|---|---|
| IIb C | NEW: IIa C | |
| Markedly elevated BNP levels. | Markedly elevated BNP levels (>threefold age- and sex-corrected normal range) confirmed by repeated measurements without other explanations. | |
| IIb C | TAKEN OUT | |
| Increase of mean pressure gradient with exercise by >20 mmHg. | ||
| IIb C | TAKEN OUT | |
| Excessive LV hypertrophy in the absence of hypertension. | ||
| NEW: IIa C Recommendation: | ||
| Severe pulmonary hypertension (systolic pulmonary artery pressure at rest >60 mmHg confirmed by invasive measurement) without other explanation. | ||
Indications for Surgery in Severe Aortic Regurgitation and Aortic Root Disease
| 2017 New Recommendations |
|---|
| NEW: I C Recommendations: |
| Patients with pliable non-calcified tricuspid or bicuspid valves who have a type I (enlargement of the aortic root with normal cusp motion) or type-II (cusp prolapse) mechanism of aortic regurgitation. |
| Aortic valve repair, using the reimplantation or remodelling with aortic annuloplasty technique, is recommended in young patients with aortic root dilationand tricuspid aortic valves, when performed by experienced surgeons. |
| NEW: IIa C Recommendations: |
| Surgery should be considered in patients who have aortic root disease with maximal ascending aortic diameter: ≥45 mmin patients with a TGFBR1 orTGFBR2 mutation (including Loeys-Dietz syndrome). |
| A lower threshold of 40 mm may be considered in women with low BSA, in patients with a TGFBR2 mutation, or in patients with severe extra-aortic features. |
AHA/ACC 2014 Guideline for the Management of Patients With Valvular Heart Diseases
Timing of Intervention
| Class I |
| "1. AVR is recommended with severe high-gradient AS who have symptoms by history or on exercise testing (stage D1)(Level of Evidence: B)" |
| "2. AVR is recommended for asymptomatic patients with severe AS (stage C2)and LVEF <50% (Level of Evidence: B)" |
| "3. AVR is indicated for patients with severe AS (stage C or D) when undergoing other cardiac surgery (Level of Evidence: B)" |
| Class IIa |
| "1. AVR is reasonable for asymptomatic patients with very severe AS (stage C1, aortic velocity ≥5.0 m/s) and low surgical risk (Level of Evidence: B)" |
| "2. AVR is reasonable in asymptomatic patients (stage C1) with severe AS and decreased exercise tolerance or an exercise fall in BP (Level of Evidence: B)" |
| "3. AVR is reasonable in symptomatic patients with low-flow/low-gradient severe AS with reduced LVEF (stage D2) with a low-dose dobutamine stress study that shows an aortic velocity ≥ 4.0 m/s (or mean pressure gradient ≥ 40 mm Hg) with a valve area ≤ 1.0 cm2 at any dobutamine dose (Level of Evidence: B)" |
| "4. AVR is reasonable in symptomatic patients who have low-flow/low-gradient severe AS (stage D3) who are normotensive and have an LVEF ≥50% if clinical, hemodynamic, and anatomic data support valve obstruction as the most likely cause of symptoms (Level of Evidence: C)" |
| "5. AVR is reasonable for patients with moderate AS (stage B) (aortic velocity 3.0–3.9 m/s) who are undergoing other cardiac surgery (Level of Evidence: C)" |
| Class IIb |
| "1. AVR may be considered for asymptomatic patients with severe AS (stage C1) and rapid disease progression and low surgical risk (Level of Evidence: C)" |
Choice of Surgical or Transcatheter Intervention
| Class I |
| "1. Surgical AVR is recommended in patients who meet an indication for AVR with low or intermediate surgical risk. (Level of Evidence: A)" |
| "2. For patients in whom [TAVR or high-risk surgical AVR is being considered, members of a Heart Valve Team should collaborate to provide optimal patient care (Level of Evidence: C)" |
| "3. TAVR is recommended in patients who meet an indication for AVR for AS who have a prohibitive surgical risk and a predicted post-TAVR survival >12 months (Level of Evidence: B)" |
| Class IIa |
| "1. TAVR is a reasonable alternative to surgical AVR in patients who meet an indication for AVR and who have high surgical risk (Level of Evidence: B)" |
| Class IIb |
| "1. Percutaneous aortic balloon dilation may be considered as a bridge to surgical or transcatheter AVR in severely symptomatic patients with severe AS. (Level of Evidence: C)" |
| Class III |
| "1. TAVR is not recommended in patients in whom existing comorbidities would preclude the expected benefit from correction of AS. (Level of Evidence: B)" |
References
- ↑ 1.0 1.1 Grube E, Laborde JC, Gerckens U, Felderhoff T, Sauren B, Buellesfeld L, Mueller R, Menichelli M, Schmidt T, Zickmann B, Iversen S, Stone GW (2006). "Percutaneous implantation of the CoreValve self-expanding valve prosthesis in high-risk patients with aortic valve disease: the Siegburg first-in-man study". Circulation. 114 (15): 1616–24. doi:10.1161/CIRCULATIONAHA.106.639450. PMID 17015786. Retrieved 2011-03-17. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 2.2 2.3 Vahl TP, Kodali SK, Leon MB (2016). "Transcatheter Aortic Valve Replacement 2016: A Modern-Day "Through the Looking-Glass" Adventure". J Am Coll Cardiol. 67 (12): 1472–87. doi:10.1016/j.jacc.2015.12.059. PMID 27012409.
- ↑ Vavuranakis M, Voudris V, Vrachatis DA, Thomopoulou S, Toutouzas K, Karavolias G, Tolios I, Sbarouni E, Lazaros G, Chrysohoou C, Khoury M, Brili S, Balanika M, Moldovan C, Stefanadis C (2010). "Transcatheter aortic valve implantation, patient selection process and procedure: two centres' experience of the intervention without general anaesthesia" (PDF). Hellenic Journal of Cardiology : HJC = Hellēnikē Kardiologikē Epitheōrēsē. 51 (6): 492–500. PMID 21169181. Retrieved 2011-03-21.
- ↑ Schäfer U, Conradi L, Diemert P, Deuschl F, Schofer N, Seiffert M, Lubos E, Schirmer J, Reichenspurner H, Blankenberg S, Treede H (2015). "Symetis ACURATE TAVI: review of the technology, developments and current data with this self-expanding transcatheter heart valve". Minerva Cardioangiol. 63 (5): 359–69. PMID 26198875.
- ↑ Heart Mirror J 2010; 157-159.
- ↑ CARDIAC INTERVENTIONS TODAY,TAVI using the CoreValve revalving system,July.August 2010
- ↑ Heart Mirror J 2010; 157-159.
- ↑ Bapat VN, Attia RQ, Thomas M (2012). "Distribution of calcium in the ascending aorta in patients undergoing transcatheter aortic valve implantation and its relevance to the transaortic approach". JACC Cardiovasc Interv. 5 (5): 470–6. doi:10.1016/j.jcin.2012.03.006. PMID 22625183.
- ↑ Zajarias A, Cribier AG (2009). "Outcomes and safety of percutaneous aortic valve replacement". Journal of the American College of Cardiology. 53 (20): 1829–36. doi:10.1016/j.jacc.2008.11.059. PMID 19442881. Retrieved 2011-03-18. Unknown parameter
|month=ignored (help) - ↑ Webb JG, Chandavimol M, Thompson CR, Ricci DR, Carere RG, Munt BI, Buller CE, Pasupati S, Lichtenstein S (2006). "Percutaneous aortic valve implantation retrograde from the femoral artery". Circulation. 113 (6): 842–50. doi:10.1161/CIRCULATIONAHA.105.582882. PMID 16461813. Retrieved 2011-03-18. Unknown parameter
|month=ignored (help) - ↑ Thomas M, Schymik G, Walther T, Himbert D, Lefèvre T, Treede H, Eggebrecht H, Rubino P, Michev I, Lange R, Anderson WN, Wendler O (2010). "Thirty-day results of the SAPIEN aortic Bioprosthesis European Outcome (SOURCE) Registry: A European registry of transcatheter aortic valve implantation using the Edwards SAPIEN valve". Circulation. 122 (1): 62–9. doi:10.1161/CIRCULATIONAHA.109.907402. PMID 20566953. Retrieved 2011-03-18. Unknown parameter
|month=ignored (help) - ↑ Fraccaro C, Napodano M, Tarantini G, Gasparetto V, Gerosa G, Bianco R, Bonato R, Pittarello D, Isabella G, Iliceto S, Ramondo A (2009). "Expanding the eligibility for transcatheter aortic valve implantation the trans-subclavian retrograde approach using: the III generation CoreValve revalving system". JACC. Cardiovascular Interventions. 2 (9): 828–33. doi:10.1016/j.jcin.2009.06.016. PMID 19778770. Retrieved 2011-03-23. Unknown parameter
|month=ignored (help) - ↑ Ruge H, Lange R, Bleiziffer S, Hutter A, Mazzitelli D, Will A, Schreiber C, Laborde JC, Bauernschmitt R (2008). "First successful aortic valve implantation with the CoreValve ReValving System via right subclavian artery access: a case report". The Heart Surgery Forum. 11 (5): E323–4. doi:10.1532/HSF98.20081021. PMID 18948247. Retrieved 2011-03-23.
- ↑ 14.0 14.1 Kahlert P, Knipp SC, Schlamann M, Thielmann M, Al-Rashid F, Weber M, Johansson U, Wendt D, Jakob HG, Forsting M, Sack S, Erbel R, Eggebrecht H (2010). "Silent and apparent cerebral ischemia after percutaneous transfemoral aortic valve implantation: a diffusion-weighted magnetic resonance imaging study". Circulation. 121 (7): 870–8. doi:10.1161/CIRCULATIONAHA.109.855866. PMID 20177005. Retrieved 2011-03-22. Unknown parameter
|month=ignored (help) - ↑ Jilaihawi H, Chin D, Vasa-Nicotera M, Jeilan M, Spyt T, Ng GA, Bence J, Logtens E, Kovac J (2009). "Predictors for permanent pacemaker requirement after transcatheter aortic valve implantation with the CoreValve bioprosthesis". American Heart Journal. 157 (5): 860–6. doi:10.1016/j.ahj.2009.02.016. PMID 19376312. Retrieved 2011-03-22. Unknown parameter
|month=ignored (help) - ↑ Gerckens U, Latsios G, Mueller R, et al. Left main PCI after trans-subclavian CoreValve implantation. Successful outcome of a combined procedure for management of a rare complication.Clin Res Cardiol. 2009;98:687-690.
- ↑ Piazza N, Onuma Y, Jesserun E, Kint PP, Maugenest AM, Anderson RH; et al. (2008). "Early and persistent intraventricular conduction abnormalities and requirements for pacemaking after percutaneous replacement of the aortic valve". JACC Cardiovasc Interv. 1 (3): 310–6. doi:10.1016/j.jcin.2008.04.007. PMID 19463319.
- ↑ Piazza N, Grube E, Gerckens U, den Heijer P, Linke A, Luha O; et al. (2008). "Procedural and 30-day outcomes following transcatheter aortic valve implantation using the third generation (18 Fr) corevalve revalving system: results from the multicentre, expanded evaluation registry 1-year following CE mark approval". EuroIntervention. 4 (2): 242–9. PMID 19110790.
- ↑ Fraccaro C, Buja G, Tarantini G, Gasparetto V, Leoni L, Razzolini R; et al. (2011). "Incidence, predictors, and outcome of conduction disorders after transcatheter self-expandable aortic valve implantation". Am J Cardiol. 107 (5): 747–54. doi:10.1016/j.amjcard.2010.10.054. PMID 21247519.
- ↑ http://www.medpagetoday.com/MeetingCoverage/EUROPACE/27358 accessed on July 1, 2011
- ↑ Khawaja MZ, Rajani R, Cook A, Khavandi A, Moynagh A, Chowdhary S, Spence MS, Brown S, Khan SQ, Walker N, Trivedi U, Hutchinson N, De Belder AJ, Moat N, Blackman DJ, Levy RD, Manoharan G, Roberts D, Khogali SS, Crean P, Brecker SJ, Baumbach A, Mullen M, Laborde JC, Hildick-Smith D (2011). "Permanent Pacemaker Insertion After CoreValve Transcatheter Aortic Valve Implantation: Incidence and Contributing Factors (the UK CoreValve Collaborative)". Circulation. doi:10.1161/CIRCULATIONAHA.109.927152. PMID 21339482. Retrieved 2011-02-23. Unknown parameter
|month=ignored (help) - ↑ CARDIAC INTERVENTIONS TODAY,TAVI using the CoreValve revalving system,July.August 2010
- ↑ "www.census.gov" (PDF).
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O'Gara PT, Rigolin VH, Sundt TM, Thompson A (2017). "2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Circulation. 135 (25): e1159–e1195. doi:10.1161/CIR.0000000000000503. PMID 28298458.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O'Gara PT, Rigolin VH, Sundt TM, Thompson A (2017). "2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". J. Am. Coll. Cardiol. 70 (2): 252–289. doi:10.1016/j.jacc.2017.03.011. PMID 28315732.
- ↑ Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Muñoz DR, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL (2017). "2017 ESC/EACTS Guidelines for the management of valvular heart disease". Eur. Heart J. 38 (36): 2739–2791. doi:10.1093/eurheartj/ehx391. PMID 28886619.

