Thrombophilia: Difference between revisions
No edit summary |
No edit summary |
||
| Line 14: | Line 14: | ||
MeshID = D019851 | | MeshID = D019851 | | ||
}} | }} | ||
{{ | {{Thrombophilia}} | ||
{{CMG}};'''Associate Editor(s)-In-Chief:''' [[User:Kashish Goel|Kashish Goel, M.D.]] | {{CMG}};'''Associate Editor(s)-In-Chief:''' [[User:Kashish Goel|Kashish Goel, M.D.]] | ||
{{SK}} Hypercoagulability, coagulability, hypercoagulable state | |||
==Overview== | ==Overview== | ||
Revision as of 13:15, 21 September 2012
| Thrombophilia | |
| OMIM | 188050 |
|---|---|
| DiseasesDB | 29080 |
| MeSH | D019851 |
|
Thrombophilia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Thrombophilia On the Web |
|
American Roentgen Ray Society Images of Thrombophilia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-In-Chief: Kashish Goel, M.D.
Synonyms and keywords: Hypercoagulability, coagulability, hypercoagulable state
Overview
Thrombophilia is defined as an increased risk of thrombosis in the body, due to an abnormality in the system of coagulation. Thrombophilia can be inherited or acquired. More than 50% of the cases of thrombosis are associated with an underlying thrombophilia. Thrombophilias are mostly associated with venous thromboembolism like deep vein thrombosis in lower extremities or pulmonary embolism. Relatively less is known about thrombophilias that predispose to arterial thromboembolism[1].
Classification
Thrombophilia can be classified in various forms.
- The most common classification is by the nature of the thrombosis: arterial, venous or combined.
- Crowther & Kelton (2003) propose to classify the abnormality by the molecular deficiency, type I being the (severe) deficiencies of inhibitors, and type II being the less severe elevation of coagulation factors.[2]
- Inherited vs. acquired
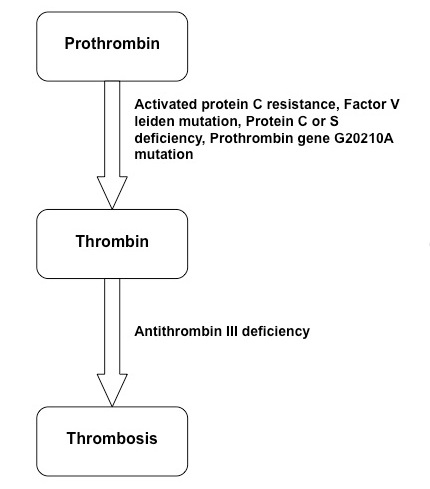
Pathophysiology
The Virchow's triad has been described classically as the patho-physiologic mechanism responsible for any thrombosis, which includes 3 components:
The mechanism of thrombophilia involves affecting the pathway of thrombosis[1]:
Adapted from: N Engl J Med. 2001 Apr 19;344(16):1222-31.
Epidemiology and Demographics
Prevalence of various inherited thrombophilias and their clinical impact
| Disorder | Healthy subjects/General population (%) | Patients with known thrombosis (%) | Estimated increase in thrombosis risk |
|---|---|---|---|
| Antithrombin deficiency | 0.02 | 1 - 4 | 10 - 20X |
| Dysfibrinogenemia | <1 | <1 | Variable |
| Protein C deficiency | 0.2 - 0.4 | 3 - 5 | 10X |
| Protein S deficiency | 0.3 - 0.13 | 2 - 4 | 10X |
| Factor V Leiden | 1 - 15 | 18 - 40 | 5X |
| G20210A prothrombin gene mutation | 2 - 5 | 7 - 16 | 3X |
| Hyperhomocystenemia | 5 | 10 | 3X |
| Elevated factor VIII levels | 11 | 25 | 5X |
The table has been adapted from Best Pract Res Clin Obstet Gynaecol. 2003 Jun;17(3):397-411[3] and data has been obtained from references[1][4][5].
Causes
Inherited
Common types:
- G1691A mutation in factor V gene (Factor V, Leiden type; 5% of the population are heterozygous for FVL)
- Prothrombin (factor II) mutation (G20210A, 5'UTR)
- Homozygous C677T mutation in the MTHFR gene
Rare forms:
- Plasminogen and fibrinolysis disorders
- Paroxysmal nocturnal hemoglobinuria
- Protein C deficiency
- Protein S deficiency
- Antithrombin III deficiency
- Dysfibrinogenemia
- Homozygous homocystinuria
- Increased levels of factor VIII, factor IX, factor XI, or fibrinogen.
Acquired
- Antiphospholipid antibodies
- Renal disease (renal loss of antithrombin)
- High homocysteine levels due to vitamin deficiency (vitamins B6, B12 and folic acid).
- Immobility
- Pregnancy and puerperium
- Oral contraceptive pills
- Malignancy
- Obesity
- African American race
- Hormone replacement therapy
- Surgery and trauma
- Older age
- Myeloproliferative disorders
- Previous thrombosis
Differential Diagnosis of Thrombophilia
(By organ system)
Laboratory testing
Indications for screening
Routine screening is not indicated in those individuals with an obvious acquired cause. For example, if the thrombosis is due to immobilisation after recent orthopedic surgery, it is unlikely that an underlying cause is found. Comprehensive testing in any patient should include complete assessment of risk factors and its effect on long-term therapy. Some of the indications of further testing may include[6][1]:
- Unexplained venous thromboembolism at an age of less than 50 years
- Recurrent spontaneous thrombosis
- Unusual sites like portal, splenic, mesenteric, hepatic or renal veins
- Family history in first-degree relatives
- Recurrent pregnancy losses[7]
- Recurrence of venous thromboembolism while adequately anticoagulated
- Warfarin-induced skin necrosis
- Unexplained arterial thromboembolism in a younger patient without significant arteriosclerosis risk factors and no cardioembolic source
Timing
The timing of tests is very important as it influences the levels of various thrombogenic factors in the body.
- Testing at the time of acute venous thrombosis is not indicated or during ongoing anti-coagulation.
- Best time to test is 4 weeks after completion of anticoagulation.
- Avoid intercurrent severe illness
- Pregnancy, oral contraceptives, hormone replacement therapy and cancer chemotherapy may also affect some tests.
- Factor V Leiden and Prothrombin mutation can be done in patients on anticoagulants and even in acute phase, as these are PCR tests. However, other tests can be done only at a later stage to rule out two disorders.
Type of tests
Tests for thrombophilia are categorized according to their priority, as discussed below:
1. General tests: These include prothrombin time, INR, and partial thromboplastin time.
2. High priority tests:
- Activated protein C resistance
- Factor V Leiden (Homozygosity or heterozygosity)
- Prothrombin gene mutation (G20210A)
- Homocysteine levels
- Factor VIII
- Lupus anticoagulant
3. Intermediate priority
- Protein C activity
- Protein S activity
- Antithrombin activity
- Anticardiolipin antibodies
4. Low priority
- Thrombin time
- Fibrinogen levels
- Factor IX activity
- Factor X activity
- MTHR gene
- High priority and intermediate priority tests should be performed in those with an unprovoked thrombotic event and have a recurrent event, cerebral-or visceral thrombosis, stillbirth, three or more unexplained spontaneous abortions, family history of venous thrombosis, or are younger than 45 years.
- High priority tests only should be conducted in those who have a first unprovoked event, age > 45 years, event provoked by pregnancy/puerperium/use of oral contraceptives or hormone-replacement therapy, proximal-vein thrombosis, pulmonary embolism, or both provoked by surgery, trauma, or immobilization.
- It is recommended that all these patients be treated with anticoagulation for at least 6 months, unless contraindicated.
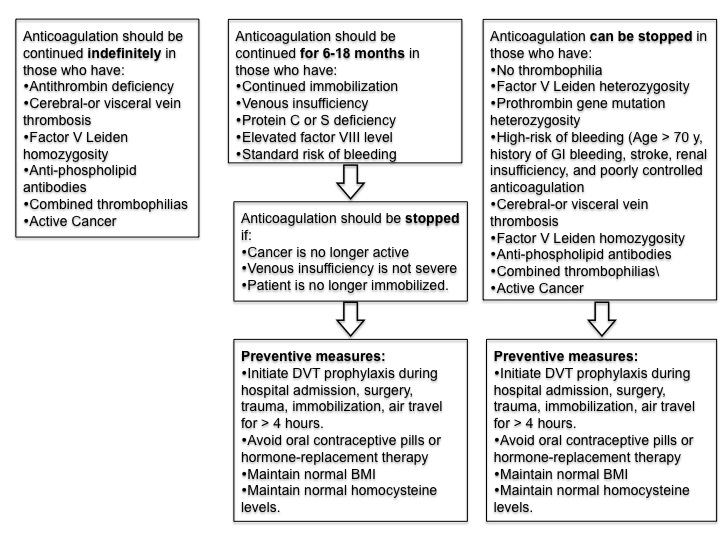
Treatment
The treatment algorithm for various thrombophilias is presented below:
The figure has been adapted from Seligsohn et al. N Engl J Med. 2001 Apr 19;344(16):1222-31.[1]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Seligsohn U, Lubetsky A (2001). "Genetic susceptibility to venous thrombosis". N. Engl. J. Med. 344 (16): 1222–31. doi:10.1056/NEJM200104193441607. PMID 11309638. Unknown parameter
|month=ignored (help) - ↑ Crowther MA, Kelton JG (2003). "Congenital thrombophilic states associated with venous thrombosis: a qualitative overview and proposed classification system". Ann. Intern. Med. 138 (2): 128–34. PMID 12529095.
- ↑ Buchanan GS, Rodgers GM, Ware Branch D (2003). "The inherited thrombophilias: genetics, epidemiology, and laboratory evaluation". Best Pract Res Clin Obstet Gynaecol. 17 (3): 397–411. PMID 12787534. Unknown parameter
|month=ignored (help) - ↑ Franco RF, Reitsma PH (2001). "Genetic risk factors of venous thrombosis". Hum. Genet. 109 (4): 369–84. doi:10.1007/s004390100593. PMID 11702218. Unknown parameter
|month=ignored (help) - ↑ Haverkate F, Samama M (1995). "Familial dysfibrinogenemia and thrombophilia. Report on a study of the SSC Subcommittee on Fibrinogen". Thromb. Haemost. 73 (1): 151–61. PMID 7740487. Unknown parameter
|month=ignored (help) - ↑ Foy P, Moll S (2009). "Thrombophilia: 2009 update". Curr Treat Options Cardiovasc Med. 11 (2): 114–28. PMID 19289024. Unknown parameter
|month=ignored (help) - ↑ Dawood, F., Farquharson, R., Quenby, S.Recurrent miscarriage. Current Obstetrics & Gynaecology, 2004; 14:247-253.