Thiazide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
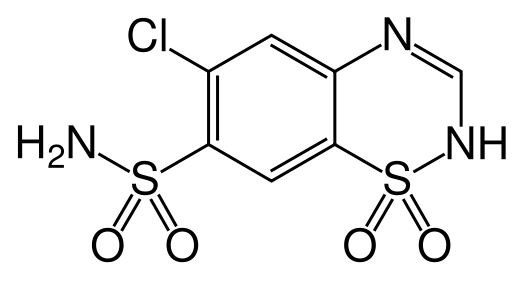
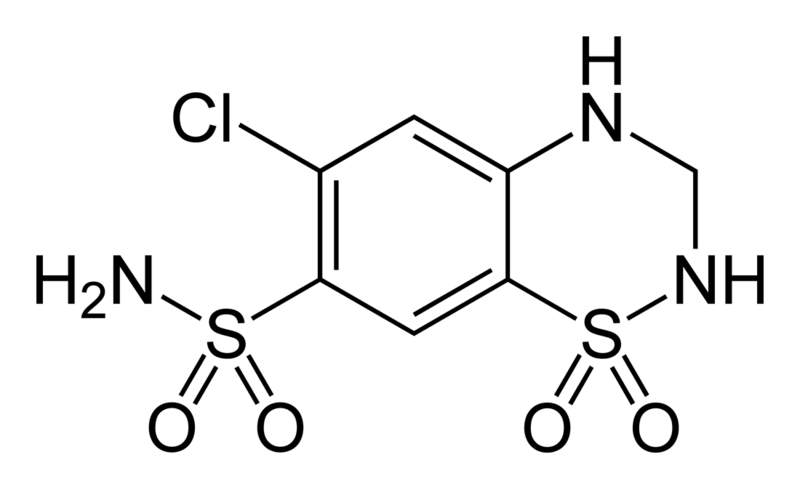
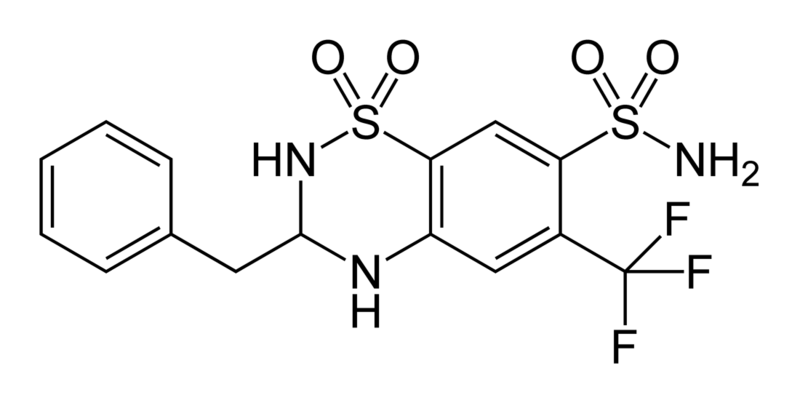
Thiazide is a term used to describe a type of molecule[1] and a class of diuretic.[2]
The members of these diuretics are derived from benzothiadiazine. They inhibit Na+/Cl- reabsorption from the distal convoluted tubules in the kidneys by blocking the thiazide-sensitive Na+-Cl- symporter. Thiazides also cause loss of potassium and an increase in serum uric acid. The chemical structure of the original thiazide diuretics contained a thiazide ring system; the term is also used for drugs with a similar action that are not chemically thiazides, such as chlortalidone and metolazone.
Denomination
That thiazide both refers to the type of molecule and the medication can sometimes lead to confusion, because some molecules can be considered thiazide diuretics, although they are not thiazides from a chemical perspective. In this context, "thiazide" refers to a drug which acts at a "thiazide receptor"[3], which is believed to be a sodium-chloride symporter.
Primary uses
Because of their vasodilator properties, Thiazides are often used to treat hypertension. They are the recommended first-line treatment in the US (JNC VII)[4] guidelines and a recommended treatment in the European (ESC/ESH)[5] guidelines. They have been shown to prevent hypertension-related morbidity and mortality although the mechanism is not fully understood. Thiazides cause vasodilation by desensitizing the vascular smooth muscle cells to calcium release induced by norepinephrine.[6]
Among the thiazides and thiazide-like diurectics, chlorthalidone may be more effective for hypertension control than hydrochlorothiazide.[7]
Side effects
Side effects can include hypokalemia, increased serum cholesterol, and impotence. The side effect of hypokalemia has motivated combining thiazides with potassium sparing diuretics (eg with amiloride in co-amilozide) and with the newer ACE inhibitors, which also lower blood pressure but cause hyperkalemia as a side effect.
Long-term usage of thiazides is also linked to increased levels of homocysteine, a toxic amino acid byproduct, that has been associated with atherosclerosis. It is recommended that patients receiving long-term thiazide treatments also receive folic acid supplements to combat the risk. They have been known to cause a paradoxical effect in Diabetes insipidus, where they reduce the volume of urine. Thiazide diuretics are capable of inhibiting urate secretions.
About 3% of the population will have an allergic reaction to a thiazide. Signs and symptoms of an allergic reaction include a rash(either eczematous reaction with red itchy scaly skin and crusting or erythema anular centrifugum), hives, itching, nasal congestion, shortness of breath, wheezing, tachycardia, cough, nausea or diarrhea. Anaphylactic reactions with hypotension, angioedema and a leukocytoclastic vasculitis are rare.
Other uses
Thiazides also lower urinary calcium excretion, making them useful in preventing calcium-containing kidney stones. This effect is associated with positive calcium balance and is associated with an increase in bone mineral density and reductions in fracture rates attributable to osteoporosis. Because of those properties, they are also used in the treatment of Dent's Disease or idiopathic hypercalciuria.
Thiazide may be combined with ACE inhibitors to increase diuresis without changing plasma potassium concentrations. While ACE inhibitors cause diuresis with potassium retention, thiazide increases potassium excretion. Their combined effects on potassium cancel each other out.
Breast milk
It should be noted that thiazides pass through breast milk, and in some cases, decrease the flow of breast milk. There is no specific information regarding the use of thiazides in children, but it is still advised that mothers avoid using thiazides during the first month of breast feeding.
Mechanisms of hypokalemia
There are several mechanisms by which thiazide diuretics cause hypokalaemia (decreased plasma potassium concentration):
- Increased delivery of sodium to the collecting ducts causes the Na/K exchanger to be activated resulting in K (and H+) loss.
- Activation of renin-angiotensin-aldosterone system by the diuretic hypovolaemia: body responds to hypovolaemia by opposing diuresis, one effect of which is to produce aldosterone which stimulates the Na/K exchanger, resulting in further loss of potassium. For this reason, ACE inhibitors, which inhibit angiotensin II production and therefore aldosterone activation, are frequently used in combination with thiazides to combat hypokalaemia.
- Flow rate in nephron is increased under diuresis, reducing potassium concentration in the lumen, thus increasing the potassium gradient. Potassium loss through the many potassium channels, such as ROMK. These are not exchangers; they allow facilitated diffusion, so the increased gradient is directly responsible for increased diffusion.
Thiazides overuse must be differentiated from other causes of hypercalcaemia
| Differential diagnosis of hyperparathyroidism on the basis of hypercalcemia | ||||||||
|---|---|---|---|---|---|---|---|---|
| Disorder | Mechanism of hypercalcemia | Clinical features | Laboratory findings | Imaging & diagnostic modalities | ||||
| PTH | Calcium | Phosphate | Other findings | |||||
| Hyperparathyroidism | Primary hyperparathyroidism | Increase in secretion of parathyroid hormone (PTH) from a primary process in parathyroid gland. Parathyroid hormone causes increase in serum calcium. |
|
↑ | ↑ | ↓/Normal | Normal/↑ calcitriol | Findings of bone resorption:
Preoperative localization of hyperfunctioning parathyroid gland:
Predicting post-operative success:
|
| Secondary hyperparathyroidism | Increase in secretion of parathyroid hormone (PTH) from a secondary process. Parathyroid hormone causes increase in serum calcium after long periods. |
|
↑ | ↓/Normal | ↑ | -- | ||
| Tertiary hyperparathyroidism | Continuous elevation of parathyroid hormone (PTH) even after successful treatment of the secondary cause of elevated parathyroid hormone. Parathyroid hormone causes increase in serum calcium. |
|
↑ | ↑ | ↑ | -- | ||
| Familial hypocalciuric hypercalcemia | This is a genetic disorder caused my mutation in calcium-sensing receptor gene. |
|
Normal/↑ | Normal/↑ | -- | -- |
| |
| Malignancy[8] | Humoral hypercalcemia of malignancy[9][10][11] | Tumor cells secretes parathyroid hormone-related protein (PTHrP) which has similar action as parathyroid hormone. |
|
-- | ↑ | ↓/Normal | ↑ PTHrP
Normal/↑ calcitriol |
|
| Osteolytic tumors | Multiple myeloma produces osteolysis of bones causing hypercalcemia. Osteolytic metasteses can cause bone resorption causing hypercalcemia. |
|
↓ | ↑ | -- | -- | ||
| Production of calcitirol | Some tumors has ectopic activity of 1-alpha-hydroxylase leading to increased production of calcitriol. Calcitriol is active form of vitamin D and causes hypercalcemia. |
|
-- | ↑ | -- | ↑ Calcitriol | ||
| Ectopic parathyroid hormone[12] | Some tumors leads to ectopic production of parathyroid hormone. |
|
↑ | ↑ | ↓/Normal | Normal/↑ calcitriol | ||
| Medication induced | Lithium[13] | Lithium lowers urinary calcium and causes hypercalcemia. Lithium has been reported to cause an increase in parathyroid hormone and enlargement if parathyroid gland after weeks to months of therapy. |
|
↑ | ↑ | -- | -- |
|
| Thiazide diuretics | Thiazide diuretics lowers urinary calcium excretion and causes hypercalcemia. |
|
-- | ↑ | -- | -- | -- | |
| Nutritional | Milk-alkali syndrome | Hypercalcemia is be caused by high intake of calcium carbonate. |
|
-- | ↑ | -- | -- | |
| Vitamin D toxicity | Excess vitamin D causes increased absorption of calcium from intestine causing hypercalcemia. |
|
-- | ↑ | -- | ↑ Vitamin D (calcidiol and/or calcitriol) | -- | |
| Granulomatous disease | Sarcoidosis[16] | Hypercalcemia is causes by endogeous production of calcitriol by disease-activated macrophages. |
|
-- | ↑ | -- | ↑ Calcitriol
↑ ACE levels |
|
References
Moreno, E (2006). Affinity-defining Domains in the Na-Cl Cotransporter. J. Biol. Chem. 281, 17266-17275.
- ↑ Thiazides at the US National Library of Medicine Medical Subject Headings (MeSH)
- ↑ Thiazide+Diuretics at the US National Library of Medicine Medical Subject Headings (MeSH)
- ↑ thiazide+receptor at the US National Library of Medicine Medical Subject Headings (MeSH)
- ↑ "The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7)".
- ↑ "escardio.org".
- ↑ Zhu Z, Zhu S, Liu D, Cao T, Wang L, Tepel M (2005). "Thiazide-like diuretics attenuate agonist-induced vasoconstriction by calcium desensitization linked to Rho kinase". Hypertension. 45 (2): 233–9. doi:10.1161/01.HYP.0000152701.97426.5f. PMID 15611360.
- ↑ Bakris GL, Sica D, White WB, Cushman WC, Weber MA, Handley A; et al. (2012). "Antihypertensive Efficacy of Hydrochlorothiazide vs Chlorthalidone Combined with Azilsartan Medoxomil". Am J Med. 125 (12): 1229.e1–1229.e10. doi:10.1016/j.amjmed.2012.05.023. PMID 22939358.
- ↑ Mirrakhimov AE (2015). "Hypercalcemia of Malignancy: An Update on Pathogenesis and Management". N Am J Med Sci. 7 (11): 483–93. doi:10.4103/1947-2714.170600. PMC 4683803. PMID 26713296.
- ↑ Ratcliffe WA, Hutchesson AC, Bundred NJ, Ratcliffe JG (1992). "Role of assays for parathyroid-hormone-related protein in investigation of hypercalcaemia". Lancet. 339 (8786): 164–7. doi:10.1016/0140-6736(92)90220-W. PMID 1346019.
- ↑ Ikeda K, Ohno H, Hane M, Yokoi H, Okada M, Honma T, Yamada A, Tatsumi Y, Tanaka T, Saitoh T (1994). "Development of a sensitive two-site immunoradiometric assay for parathyroid hormone-related peptide: evidence for elevated levels in plasma from patients with adult T-cell leukemia/lymphoma and B-cell lymphoma". J. Clin. Endocrinol. Metab. 79 (5): 1322–7. doi:10.1210/jcem.79.5.7962324. PMID 7962324.
- ↑ Horwitz MJ, Tedesco MB, Sereika SM, Hollis BW, Garcia-Ocaña A, Stewart AF (2003). "Direct comparison of sustained infusion of human parathyroid hormone-related protein-(1-36) [hPTHrP-(1-36)] versus hPTH-(1-34) on serum calcium, plasma 1,25-dihydroxyvitamin D concentrations, and fractional calcium excretion in healthy human volunteers". J. Clin. Endocrinol. Metab. 88 (4): 1603–9. doi:10.1210/jc.2002-020773. PMID 12679445.
- ↑ VanHouten JN, Yu N, Rimm D, Dotto J, Arnold A, Wysolmerski JJ, Udelsman R (2006). "Hypercalcemia of malignancy due to ectopic transactivation of the parathyroid hormone gene". J. Clin. Endocrinol. Metab. 91 (2): 580–3. doi:10.1210/jc.2005-2095. PMID 16263810.
- ↑ Mallette LE, Khouri K, Zengotita H, Hollis BW, Malini S (1989). "Lithium treatment increases intact and midregion parathyroid hormone and parathyroid volume". J. Clin. Endocrinol. Metab. 68 (3): 654–60. doi:10.1210/jcem-68-3-654. PMID 2918061.
- ↑ Jacobus CH, Holick MF, Shao Q, Chen TC, Holm IA, Kolodny JM, Fuleihan GE, Seely EW (1992). "Hypervitaminosis D associated with drinking milk". N. Engl. J. Med. 326 (18): 1173–7. doi:10.1056/NEJM199204303261801. PMID 1313547.
- ↑ Hoeck HC, Laurberg G, Laurberg P (1994). "Hypercalcaemic crisis after excessive topical use of a vitamin D derivative". J. Intern. Med. 235 (3): 281–2. PMID 8120527.
- ↑ Dusso AS, Kamimura S, Gallieni M, Zhong M, Negrea L, Shapiro S, Slatopolsky E (1997). "gamma-Interferon-induced resistance to 1,25-(OH)2 D3 in human monocytes and macrophages: a mechanism for the hypercalcemia of various granulomatoses". J. Clin. Endocrinol. Metab. 82 (7): 2222–32. doi:10.1210/jcem.82.7.4074. PMID 9215298.
External links