The heart in takayasu arteritis: Difference between revisions
Rim Halaby (talk | contribs) No edit summary |
Rim Halaby (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{SI}} | {{SI}} | ||
{{CMG}} | {{CMG}} | ||
Revision as of 16:58, 2 February 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Assistant Editor-in-Chief: Brian Blank
Synonyms and related keywords: Pulseless disease, non-specific aorto-arteritis, reverse coarctation, aortic arch syndrome, aortitis syndrome.
Overview
Cardiac complications of takayasu arteritis (TA) may include aortic regurgitation, myocarditis and congestive heart failure.
Pathophysiology and Classification
The classification scheme for late-phase Takayasu arteritis is based upon the site of involvement:
Type I
Classic pulseless type that involves the brachiocephalic trunk, carotid arteries, and subclavian arteries
Type II
Combination of type I and III
Type III
Atypical coarctation type that involves the thoracic and abdominal aorta distal to the aortic arch and its major branches
Type IV
Dilated type that involves extensive dilatation of the length of the aorta and its major branches
The most common type is type III, which is found in as many as 65% of patients. The most commonly involved vessels include the left subclavian artery (50%), left common carotid artery (20%), brachiocephalic trunk, renal arteries, celiac trunk, superior mesenteric artery, and pulmonary arteries (50%). Infrequently, the axillary, brachial, vertebral, coronary, and iliac arteries are involved.
Diagnosis
Initially, a diagnosis of TA can be missed for months or years because its symptoms can be nonspecific (fever, lethargy, etc.).
Physical Examination
While Takayasu arteritis is sometimes referred to as the "pulseless disease", it is important to note that a missing peripheral pulse usually occurs late in the course of TA. More often individuals with TA present with an asymmetric pulse.[1]
Imaging Studies
The diagnosis of TA is sometimes made when a widened mediastinum is noted on a chest x ray. A follow-up CT scan will often demonstrate a widened aortic arch. [1]
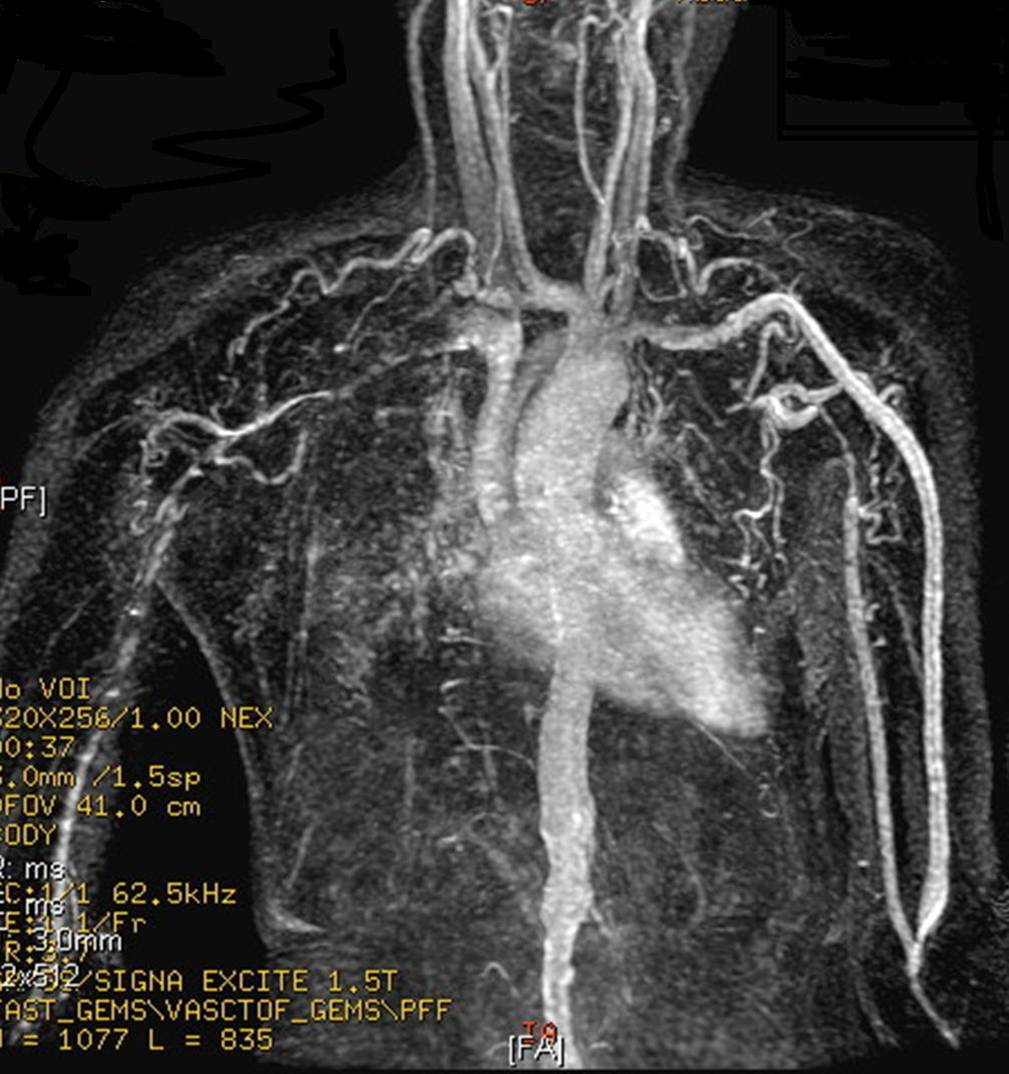
Computed Tomography and Magnetic Resonance Angiography
Computed Tomography (CT) and Magnetic Resonance Angiography (MRA) are the gold standrad imaging modalities for TA and may demonstrate mural thickening of the aorta and luminal narrowing. Use of contrast may reveal inflammatory lesions prior to the development of stenoses; these lesions may be missed by angiography. Aortic lesions including stenosis, dilatation, wall thickening, and mural thrombi are well visualized on MRI, which is less adequate in visualizing distal lesions of the subclavian vessels and common carotids. [2] Non-contrast T2-weighted STIR images may be used to monitor edema in the aortic wall, which may be a surrogate for inflammation; edema may present more than 94% of patients with clinically active disease. One disadvantage of MRA is that pressure differentials cannot be measured across lesions in which imaging findings regarding their hemodynamic significance are inconclusive.
-
This MR angiogram demonstrates findings typical of Takayasu arteritis. A 32 years old Asian female has CRF and weak functioning iatrogenic fistula in left upper limb. The cause of malfunction can be explained by narrowing and occlusion of upper limb arteries. Notice also narrowed abdominal aorta. (Image courtesy of Dr Ahmed Haroun)
-
MRA: A 15 year-old girl with known Takayasu arteritis presented for MRI to investigate back pain. The axial T1-weighted post-gadolinium MRI above shows thickened, enhancing aortic wall, consistent with large vessel vasculitis. (Image courtesy of Dr Laughlin Dawes)
Warning: Gadolinium-based contrast agents [gadopentetate dimeglumine (Magnevist), gadobenate dimeglumine (MultiHance), gadodiamide (Omniscan), gadoversetamide (OptiMARK), gadoteridol (ProHance)] have recently been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. In December 2006, the FDA had received reports of 90 such cases. Worldwide, over 200 cases have been reported, according to the FDA. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. [3]
While computed tomography and MRA are the best imaging modalities, findings on other imaging modalities include:
Chest radiography
Chest radiographs may reveal widening of the ascending aorta, irregular descending aorta, aortic calcifications, and rib notching (late findings).
Duplex Doppler
This modality may be used to evaluate and monitor disease in the common carotids and subclavian arteries; however, this imaging study is not useful in evaluating the aorta.
Carotid Ultrasound
Carotid ultrasound demonstrates a homogenous circumferential thickening of the vessel wall that is distinguishable from atherosclerotic thickening.
Gallium-67 radionuclide scan
This scan may demonstrate increased uptake in the aorta and branches.
Prognosis
Five year survival in TA is over 90%, but TA is associated with significant morbidity.[1]
References